Abstract
Polycystic ovary syndrome is a complex and heterogenous disorder involving multiple organ systems and different molecular pathways. It is tightly associated with obesity and especially abdominal obesity. As body weight reduction is the main modifiable risk factor for polycystic ovary syndrome, therapeutic approaches in overweight or obese women with polycystic ovary syndrome have been developed. Liraglutide is a glucagon-like peptide-1 receptor agonist that promotes sustained weight loss, as well as abdominal fat reduction, in individuals with obesity, prediabetes, and type 2 diabetes mellitus. The majority of current clinical studies have demonstrated that liraglutide therapy achieved significant reductions in body weight, body mass index, and abdominal circumference in overweight and obese women with polycystic ovary syndrome. Liraglutide therapy promoted significant improvements in free testosterone and sex hormone-binding globulin levels in some studies. Important metabolic and hormonal improvements were also reported after the combination of liraglutide with metformin. Increased menstrual frequency, as well as potential positive effects in reproduction, were described. However, the small number of participants, short duration, and low daily liraglutide dose are some of the main limitations of these studies. Larger and longer, multi-centred, double-blind, placebo-controlled trials of liraglutide monotherapy or combination therapy, with prolonged post-interventional monitoring, are crucially anticipated. Metabolic, hormonal, and reproductive primary outcomes should be uniformly addressed, to tailor future targeted treatment approaches, according to the patient phenotype and needs. This will improve long-term therapeutic outcomes in this population.

Similar content being viewed by others
References
Mahalingaiah S, Diamanti-Kandarakis E. Targets to treat metabolic syndrome in polycystic ovary syndrome. Expert Opin Ther Targets. 2015;19:1561–74.
Stein IF, Leventhal ML. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstet Gynecol. 1935;29:181–91.
Zawadzki J, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In: Dunaif A, Givens J, Haseltine F, Merriam G, editors. Polycystic ovary syndrome. Cambridge: Blackwell Scientific Publications; 1992. p. 377–384.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25.
Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, et al. Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an androgen excess society guideline. J Clin Endocrinol Metab. 2006;91:4237–45.
Balen AH, Laven JS, Tan SL, Dewailly D. Ultrasound assessment of the polycystic ovary: international consensus definitions. Hum Reprod Update. 2003;9:505–14.
Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016;37:467–520.
Dumesic DA, Oberfield SE, Stener-Victorin E, Marshall JC, Laven JS, Legro RS. Scientific statement on the diagnostic criteria, epidemiology, pathophysiology, and molecular genetics of polycystic ovary syndrome. Endocr Rev. 2015;36:487–525.
Diamanti-Kandarakis E. Insulin resistance in PCOS. Endocrine. 2006;30:13–7.
Dunaif A, Segal KR, Futterweit W, Dobrjansky A. Profound peripheral insulin resistance, independent of obesity, in polycystic ovary syndrome. Diabetes. 1989;38:1165–74.
Diamanti-Kandarakis E. Role of obesity and adiposity in polycystic ovary syndrome. Int J Obes (Lond). 2007;31(Suppl. 2):S8–13 (discussion S31–2).
Papaetis GS, Papakyriakou P, Panagiotou TN. Central obesity, type 2 diabetes and insulin: exploring a pathway full of thorns. Arch Med Sci. 2015;11:463–82.
Lim SS, Davies MJ, Norman RJ, Moran LJ. Overweight, obesity and central obesity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2012;18:618–37.
Papaetis GS, Orphanidou D, Panagiotou TN. Thiazolidinediones and type 2 diabetes: from cellular targets to cardiovascular benefit. Curr Drug Targets. 2011;12:1498–512.
Robinson S, Kiddy D, Gelding SV, Willis D, Niththyananthan R, Bush A, et al. The relationship of insulin insensitivity to menstrual pattern in women with hyperandrogenism and polycystic ovaries. Clin Endocrinol (Oxf). 1993;39:351–5.
Legro RS, Dodson WC, Kris-Etherton PM, et al. Randomized controlled trial of preconception interventions in infertile women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2015;100:4048–58.
Conway G, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Franks S, Gambineri A, et al. The polycystic ovary syndrome: a position statement from the European Society of Endocrinology. Eur J Endocrinol. 2014;171:P1–29.
Vassilatou E. Nonalcoholic fatty liver disease and polycystic ovary syndrome. World J Gastroenterol. 2014;20:8351–63.
Horton R, Tait JF. Androstenedione production and interconversion rates measured in peripheral blood and studies on the possible site of its conversion to testosterone. J Clin Investig. 1966;45:301–13.
Kirschner MA, Bardin CW. Androgen production and metabolism in normal and virilized women. Metabolism. 1972;21:667–88.
Ehrmann DA, Barnes RB, Rosenfield RL. Polycystic ovary syndrome as a form of functional ovarian hyperandrogenism due to dysregulation of androgen secretion. Endocr Rev. 1995;16:322–53.
Nelson VL, Qin KN, Rosenfield RL, Wood JR, Penning TM, Legro RS, et al. The biochemical basis for increased testosterone production in theca cells propagated from patients with polycystic ovary syndrome. J Clin Endocrinol Metab. 2001;86:5925–33.
Coffler MS, Patel K, Dahan MH, Malcom PJ, Kawashima T, Deutsch R, et al. Evidence for abnormal granulosa cell responsiveness to follicle-stimulating hormone in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2003;88:1742–7.
Wilson EA, Erickson GF, Zarutski P, Finn AE, Tulchinsky D, Ryan KJ. Endocrine studies of normal and polycystic ovarian tissues in vitro. Am J Obstet Gynecol. 1979;134:56–63.
Vendola KA, Zhou J, Adesanya OO, Weil SJ, Bondy CA. Androgens stimulate early stages of follicular growth in the primate ovary. J Clin Investig. 1998;101:2622–9.
Weil S, Vendola K, Zhou J, Bondy CA. Androgen and follicle-stimulating hormone interactions in primate ovarian follicle development. J Clin Endocrinol Metab. 1999;84:2951–6.
Franks S, Stark J, Hardy K. Follicle dynamics and anovulation in polycystic ovary syndrome. Hum Reprod Update. 2008;14:367–78.
Azziz R, Black V, Hines GA, Fox LM, Boots LR. Adrenal androgen excess in the polycystic ovary syndrome: sensitivity and responsivity of the hypothalamic–pituitary–adrenal axis. J Clin Endocrinol Metab. 1998;83:2317–23.
Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. 2012;33:981–1030.
Wu XK, Zhou SY, Liu JX, Pöllänen P, Sallinen K, Mäkinen M, et al. Selective ovary resistance to insulin signalling in women with polycystic ovary syndrome. Fertil Steril. 2003;80:954–65.
Barbieri R, Makris A, Randall R, Daniels G, Kistner R, Ryan K. Insulin stimulates androgen accumulation in incubations of ovarian stroma obtained from women with hyperandrogenism. J Clin Endocrinol Metab. 1986;62:904–10.
Ciaraldi TP, Aroda V, Mudaliar S, Chang RJ, Henry RR. Polycystic ovary syndrome is associated with tissue-specific differences in insulin resistance. J Clin Endocrinol Metab. 2009;94:157–63.
Franks S, Gilling-Smith C, Watson H, Willis D. Insulin action in the normal and polycystic ovary. Endocrinol Metab Clin N Am. 1999;28:361–78.
Cara JF, Rosenfield RL. Insulin-like growth factor I and insulin potentiate luteinizing hormone-induced androgen synthesis by rat ovarian theca-interstitial cells. Endocrinology. 1988;123:733–9.
Rosenfield RL, Barnes RB, Ehrmann DA. Studies of the nature of 17-hydroxyprogesterone hyperresponsiveness to gonadotropin-releasing hormone agonist challenge in functional ovarian hyperandrogenism. J Clin Endocrinol Metab. 1994;79:1686–92.
Hernandez ER, Resnick CE, Holtzclaw WD, Payne DW, Adashi EY. Insulin as a regulator of androgen biosynthesis by cultured rat ovarian cells: cellular mechanism (s) underlying physiological and pharmacological hormonal actions. Endocrinology. 1988;122:2034–43.
Comim FV, Teerds K, Hardy K, Franks S. Increased protein expression of LHCG receptor and 17α-hydroxylase/17-20-lyase in human polycystic ovaries. Hum Reprod. 2013;28:3086–92.
Nestler JE, Powers LP, Matt DW, Steingold KA, Plymate SR, Rittmaster RS, et al. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991;72:83–9.
Moll GW Jr, Rosenfield RL. Testosterone binding and free plasma androgen concentrations under physiological conditions: characterization by flow dialysis technique. J Clin Endocrinol Metab. 1979;49:730–3.
Lovejoy JC, Bray GA, Bourgeois MO, Macchiavelli R, Rood JC, Greeson C, et al. Exogenous androgens influence body composition and regional body fat distribution in obese postmenopausal women: a clinical research center study. J Clin Endocrinol Metab. 1996;81:2198–203.
Romualdi D, Giuliani M, Draisci G, Costantini B, Cristello F, Lanzone A, et al. Pioglitazone reduces the adrenal androgen response to corticotropin-releasing factor without changes in ACTH release in hyperinsulinemic women with polycystic ovary syndrome. Fertil Steril. 2007;88:131–8.
Dumont A, Robin G, Catteau-Jonard S, Dewailly D. Role of anti-Müllerian hormone in pathophysiology, diagnosis and treatment of polycystic ovary syndrome: a review. Reprod Biol Endocrinol. 2015;13:137.
Creutzfeldt W. The incretin concept today. Diabetologia. 1979;16:75–85.
Papaetis GS. Incretin-based therapies in prediabetes: current evidence and future perspectives. World J Diabetes. 2014;5:817–34.
Holst JJ. Glucagon-like peptide-1: from extract to agent. The Claude Bernard Lecture, 2005. Diabetologia. 2006;49:253–60.
Nishiyama Y, Hasegawa T, Fujita S, Iwata N, Nagao S, Hosoya T, et al. Incretins modulate progesterone biosynthesis by regulating bone morphogenetic protein activity in rat granulosa cells. J Steroid Biochem Mol Biol. 2018;178:82–8.
Jensterle M, Janez A, Fliers E, DeVries JH, Vrtacnik-Bokal E, Siegelaar SE. The role of glucagon-like peptide-1 in reproduction: from physiology to therapeutic perspective. Hum Reprod Update. 2019;25:504–17.
Maclusky N, Cook S, Scrocchi L, Shin J, Kim J, Vaccarino F, et al. Neuroendocrine function and response to stress in mice with complete disruption of glucagon-like peptide-1 receptor signaling. Endocrinology. 2000;141:752–62.
Moffett RC, Naughton V. Emerging role of GIP and related gut hormones in fertility and PCOS. Peptides. 2020;125:170233.
Zhu L, Zhou J, Pan Y, Lv J, Liu Y, Yu S, et al. Glucagon-like peptide-1 receptor expression and its functions are regulated by androgen. Biomed Pharmacother. 2019;120:109555.
Vrbikova J, Hill M, Bendlova B, Grimmichova T, Dvorakova K, Vondra K, et al. Incretin levels in polycystic ovary syndrome. Eur J Endocrinol. 2008;159:121–7.
Aydin K, Arusoglu G, Koksal G, Cinar N, Aksoy DY, Yildiz BO. Fasting and postprandial glucagon like peptide 1 and oral contraception in polycystic ovary syndrome. Clin Endocrinol (Oxf). 2014;81:588–92.
Lin T, Li S, Xu H, Zhou H, Feng R, Liu W, et al. Gastrointestinal hormone secretion in women with polycystic ovary syndrome: an observational study. Hum Reprod. 2015;30:2639–44.
Gama R, Norris F, Wright J, Morgan L, Hampton S, Watkins S, et al. The entero-insular axis in polycystic ovarian syndrome. Ann Clin Biochem. 1996;33:190–5.
Pontikis C, Yavropoulou MP, Toulis KA, Kotsa K, Kazakos K, Papazisi A, et al. The incretin effect and secretion in obese and lean women with polycystic ovary syndrome: a pilot study. J Womens Health (Larchmt). 2011;20:971–6.
Svendsen PF, Nilas L, Madsbad S, Holst JJ. Incretin hormone secretion in women with polycystic ovary syndrome: roles of obesity, insulin sensitivity, and treatment with metformin. Metabolism. 2009;58:586–93.
Cassar S, Teede HJ, Harrison CL, Joham AE, Moran LJ, Stepto NK. Biomarkers and insulin sensitivity in women with polycystic ovary syndrome: characteristics and predictive capacity. Clin Endocrinol (Oxf). 2015;83:50–8.
Ferjan S, Jensterle M, Oblak T, Zitnik IP, Marc J, Goricar K, et al. An impaired glucagon-like peptide-1 response is associated with prediabetes in polycystic ovary syndrome with obesity. J Int Med Res. 2019;47:4691–700.
Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2012;8:728–42.
Russell-Jones D. Molecular, pharmacological and clinical aspects of liraglutide, a once-daily human GLP-1 analogue. Mol Cell Endocrinol. 2009;297:137–40.
Knudsen LB. Liraglutide: the therapeutic promise from animal models. Int J Clin Pract Suppl. 2010;167:4–11.
Papaetis GS. Liraglutide therapy in a prediabetic state: rethinking the evidence. Curr Diabetes Rev. 2019. https://doi.org/10.2174/1573399816666191230113446.
Davies MJ, Bergenstal R, Bode B, Kushner RF, Lewin A, Skjøth TV, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE diabetes randomized clinical trial. JAMA. 2015;18(314):687–99.
Lamos EM, Malek R, Davis SN. GLP-1 receptor agonists in the treatment of polycystic ovary syndrome. Expert Rev Clin Pharmacol. 2017;10:401–8.
Tzotzas T, Karras SN, Katsiki N. Glucagon-like peptide-1 (GLP-1) receptor agonists in the treatment of obese women with polycystic ovary syndrome. Curr Vasc Pharmacol. 2017;15:218–29.
Legro RS. Obesity and PCOS: implications for diagnosis and treatment. Semin Reprod Med. 2012;30:496–506.
Escobar-Morreale HF, Botella-Carretero JI, Alvarez-Blasco F, Sancho J, San Millán JL. The polycystic ovary syndrome associated with morbid obesity may resolve after weight loss induced by bariatric surgery. J Clin Endocrinol Metab. 2005;90:6364–9.
Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33:1602–18.
Hoang V, Bi J, Mohankumar SM, Vyas AK. Liraglutide improves hypertension and metabolic perturbation in a rat model of polycystic ovarian syndrome. PLoS ONE. 2015;10:e0126119.
Torres Fernandez ED, Huffman AM, Syed M, Romero DG, Yanes Cardozo LL. Effect of GLP-1 receptor agonists in the cardiometabolic complications in a rat model of postmenopausal PCOS. Endocrinology. 2019;160:2787–99.
Singh A, Fernandes JRD, Chhabra G, Krishna A, Banerjee A. Liraglutide modulates adipokine expression during adipogenesis, ameliorating obesity, and polycystic ovary syndrome in mice. Endocrine. 2019;64:349–66.
Heppner KM, Baquero AF, Bennett CM, Lindsley SR, Kirigiti MA, Bennett B, et al. GLP-1R signaling directly activates arcuate nucleus kisspeptin action in brain slices but does not rescue luteinizing hormone inhibition in ovariectomized mice during negative energy balance. eNeuro. 2017. https://doi.org/10.1523/ENEURO.0198-16.2016.
Jensterle SM, Kocjan T, Pfeifer M, Kravos NA, Janez A. Short-term combined treatment with liraglutide and metformin leads to significant weight loss in obese women with polycystic ovary syndrome and previous poor response to metformin. Eur J Endocrinol. 2014;170:451–9.
Jensterle M, Kocjan T, Kravos NA, Pfeifer M, Janez A. Short-term intervention with liraglutide improved eating behavior in obese women with polycystic ovary syndrome. Endocr Res. 2015;40:133–8.
Jensterle M, Goricar K, Janez A. Metformin as an initial adjunct to low-dose liraglutide enhances the weight-decreasing potential of liraglutide in obese polycystic ovary syndrome: randomized control study. Exp Ther Med. 2016;11:1194–200.
Jensterle M, Kravos NA, Pfeifer M, Kocjan T, Janez A. A 12-week treatment with the long-acting glucagon-like peptide 1 receptor agonist liraglutide leads to significant weight loss in a subset of obese women with newly diagnosed polycystic ovary syndrome. Hormones (Athens). 2015;14:81–90.
Palomba S, Kurzthaler D, Hadziomerovic-Pekic D, Wildt L, Seeber BE. Metformin induces a prompt decrease in LH-stimulated testosterone response in women with PCOS independent of its insulin-sensitizing effects. Reprod Biol Endocrinol. 2014;12:98.
Jensterle M, Salamun V, Kocjan T, Vrtacnik Bokal E, Janez A. Short term monotherapy with GLP-1 receptor agonist liraglutide or PDE 4 inhibitor roflumilast is superior to metformin in weight loss in obese PCOS women: a pilot randomized study. J Ovarian Res. 2015;8:32.
Wouters EF, Bredenbröker D, Teichmann P, Brose M, Rabe KF, Fabbri LM, et al. Effect of the phosphodiesterase 4 inhibitor roflumilast on glucose metabolism in patients with treatment-naive, newly diagnosed type 2 diabetes mellitus. J Clin Endocrinol Metab. 2012;97:E1720–E17251725.
Jensterle M, Kravos NA, Goričar K, Janez A. Short-term effectiveness of low dose liraglutide in combination with metformin versus high dose liraglutide alone in treatment of obese PCOS: randomized trial. BMC Endocr Disord. 2017;17:5.
Palomba S, Falbo A, Zullo F, Orio F Jr. Evidence-based and potential benefits of metformin in the polycystic ovary syndrome: a comprehensive review. Endocr Rev. 2009;30:1–50.
Diamanti-Kandarakis E, Christakou CD, Kandaraki E, Economou FN. Metformin: an old medication of new fashion: evolving new molecular mechanisms and clinical implications in polycystic ovary syndrome. Eur J Endocrinol. 2010;162:193–21212.
Ferjan S, Janez A, Jensterle M. Dipeptidyl peptidase-4 inhibitor sitagliptin prevented weight regain in obese women with polycystic ovary syndrome previously treated with liraglutide: a pilot randomized study. Metab Syndr Relat Disord. 2017;15:515–20.
Salamun V, Jensterle M, Janez A, Vrtacnik B. Liraglutide increases IVF pregnancy rates in obese PCOS women with poor response to first-line reproductive treatments: a pilot randomized study. Eur J Endocrinol. 2018;179:1–11.
Tso LO, Costello MF, Albuquerque LE, Andriolo RB, Macedo CR. Metformin treatment before and during IVF or ICSI in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2014;2014(11):CD006105.
Kahal H, Aburima A, Ungvari T, Rigby AS, Coady AM, Vince RV, et al. The effects of treatment with liraglutide on atherothrombotic risk in obese young women with polycystic ovary syndrome and controls. BMC Endocr Disord. 2015;15:14.
Kahal H, Abouda G, Rigby AS, Coady AM, Kilpatrick ES, Atkin SL. Glucagon-like peptide-1 analogue, liraglutide, improves liver fibrosis markers in obese women with polycystic ovary syndrome and nonalcoholic fatty liver disease. Clin Endocrinol (Oxford). 2014;81:523–8.
Kahal H, Kilpatrick E, Rigby A, Coady A, Atkin S. The effects of treatment with liraglutide on quality of life and depression in young obese women with PCOS and controls. Gynecol Endocrinol. 2019;35:142–5.
Nylander M, Frøssing S, Clausen HV, Kistorp C, Faber J, Skouby SO. Effects of liraglutide on ovarian dysfunction in polycystic ovary syndrome: a randomized clinical trial. Reprod Biomed Online. 2017;35:121–7.
Frøssing S, Nylander M, Chabanova E, Frystyk J, Holst JJ, Kistorp C, et al. Effect of liraglutide on ectopic fat in polycystic ovary syndrome: a randomized clinical trial. Diabetes Obes Metab. 2018;20:215–8.
Nylander M, Frøssing S, Kistorp C, Faber J, Skouby SO. Liraglutide in polycystic ovary syndrome: a randomized trial, investigating effects on thrombogenic potential. Endocr Connect. 2017;6:89–99.
Frøssing S, Nylander M, Aziz M, Skouby SO, Kistorp C, Faber J. Atrial natriuretic peptide, copeptin and adrenomedullin levels in polycystic ovary syndrome: a case–control study. Gynecol Endocrinol. 2017;33:30–3.
Rasmussen CB, Lindenberg S. The effect of liraglutide on weight loss in women with polycystic ovary syndrome: an observational study. Front Endocrinol (Lausanne). 2014;5:140.
Niafar M, Pourafkari L, Porhomayon J, Nader N. A systematic review of GLP-1 agonists on the metabolic syndrome in women with polycystic ovaries. Arch Gynecol Obstet. 2016;293:509–15.
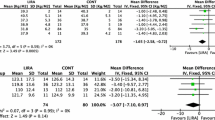
Han Y, Li Y, He B. GLP-1 receptor agonists versus metformin in PCOS: a systematic review and meta-analysis. Reprod Biomed Online. 2019;39:332–42.
Gao LH, Zhang CL, Liu XY, Liu J, Zhong CF. Pilot clinical study of the efficacy of liraglutide in treating polycystic ovary syndrome patients with type 2 diabetes mellitus. Clin Focus. 2016;31:539–42.
Wang FF, Wu Y, Zhu YH, Ding T, Batterham RL, Qu F, et al. Pharmacologic therapy to induce weight loss in women who have obesity/overweight with polycystic ovary syndrome: a systematic review and network meta-analysis. Obes Rev. 2018;19:1424–45.
Durmus U, Duran C, Ecirli S. Visceral adiposity index levels in overweight and/or obese, and non-obese patients with polycystic ovary syndrome and its relationship with metabolic and inflammatory parameters. J Endocrinol Investig. 2017;40:487–97.
Glueck CJ, Papanna R, Wang P, Goldenberg N, Sieve-Smith L. Incidence and treatment of metabolic syndrome in newly referred women with confirmed polycystic ovarian syndrome. Metabolism. 2003;52:908–15.
Reid TS. Practical use of glucagon-like-peptide-1 receptor agonists therapy in primary care. Clin Diabetes. 2013;31:148–57.
Pyke C, Heller RS, Kirk RK, Ørskov C, Reedtz-Runge S, Kaastrup P, et al. GLP-1 receptor localization in monkey and human tissue: novel distribution revealed with extensively validated monoclonal antibody. Endocrinology. 2014;155:1280–90.
Kumarathurai P, Anholm C, Larsen BS, Olsen RH, Madsbad S, Kristiansen O, et al. Effects of liraglutide on heart rate and heart rate variability: a randomized, double-blind, placebo-controlled crossover study. Diabetes Care. 2017;40:117–24.
Drucker DJ. The ascending GLP-1 road from clinical safety to reduction of cardiovascular complications. Diabetes. 2018;67:1710–9.
Greco D. Normal pregnancy outcome after first-trimester exposure to liraglutide in a woman with type 2 diabetes. Diabet Med. 2015;32:e29–30.
Younes ST, Maeda KJ, Sasser J, Ryan MJ. The glucagon-like peptide 1 receptor agonist liraglutide attenuates placental ischemia-induced hypertension. Am J Physiol Heart Circ Physiol. 2020;318:H72–H7777.
Liu X, Zhang Y, Zheng S-Y, Lin R, Xie Y-J, Chen H, et al. Efficacy of exenatide on weight loss, metabolic parameters and pregnancy in overweight/obese polycystic ovary syndrome. Clin Endocrinol (Oxf). 2017;87:767–74.
Jensterle M, Pirš B, Goričar K, Dolžan V, Janež A. Genetic variability in GLP-1 receptor is associated with inter-individual differences in weight lowering potential of liraglutide in obese women with PCOS: a pilot study. Eur J Clin Pharmacol. 2015;71:817–24.
ClinicalTrials.gov. Liraglutide 3 mg (Saxenda) on weight, body composition, hormonal and metabolic parameters in obese women with PCOS (SAXAPCOS). https://clinicaltrials.gov/ct2/show/NCT03480022?term=liraglutide&cond=PCOS&draw=1&rank=5. Accessed 18 Jun 2020.
Whitten JS. Liraglutide (Saxenda) for weight loss. Am Fam Physician. 2016;94:161–6.
Papamargaritis D, Al-Najim W, Lim J, Crane J, Lean M, le Roux C, et al. Effectiveness and cost of integrating a pragmatic pathway for prescribing liraglutide 3.0 mg in obesity services (STRIVE Study): study protocol of an open-label, real-world, randomized, controlled trial. BMJ Open. 2020;10:e034137.
Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol. 2018;14:270–84.
Moran LJ, Noakes M, Clifton PM, Tomlinson L, Galletly C, Norman RJ. Dietary composition in restoring reproductive and metabolic physiology in overweight women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2004;88:812–9.
Crosignani PG, Colombo M, Vegetti W, Somigliana E, Gessati A, Ragni G. Overweight and obese anovulatory patients with polycystic ovaries: parallel improvements in anthropometric indices, ovarian physiology and fertility rate induced by diet. Hum Reprod. 2003;18:1928–32.
Tan S, Hahn S, Benson S, Dietz T, Lahner H, Moeller LC, et al. Metformin improves polycystic ovary syndrome symptoms irrespective of pre-treatment insulin resistance. Eur J Endocrinol. 2007;157:669–76.
Maida A, Lamont BJ, Cao X, Drucker DJ. Metformin regulates the incretin receptor axis via a pathway dependent on peroxisome proliferator-activated receptor-α in mice. Diabetologia. 2011;54:339–49.
McKiney JM, Irwin N, Flatt PR, Bailey CJ, McClenaghan NH. Acute and long-term effects of metformin on the function and insulin secretory responsiveness of clonal-cells. Biol Chem. 2010;391:1451–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this article was not supported by any external funding.
Conflict of interest
Georgios S. Papaetis, Panagiota K. Filippou, Kiriaki G. Constantinidou, and Christina S. Stylianou have no conflicts of interest that are directly relevant to the content of this article.
Rights and permissions
About this article
Cite this article
Papaetis, G.S., Filippou, P.K., Constantinidou, K.G. et al. Liraglutide: New Perspectives for the Treatment of Polycystic Ovary Syndrome. Clin Drug Investig 40, 695–713 (2020). https://doi.org/10.1007/s40261-020-00942-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-020-00942-2