Abstract
Background and Objective
Patients with atrial fibrillation (AF) and advanced chronic kidney disease (CKD) are at high risk of adverse events and are complicated to manage. There is little evidence on the effects of non-vitamin K oral anticoagulants in patients with severe CKD. Preliminary data in patients taking edoxaban whose creatinine clearance fell below 30 mL/min showed a low risk of stroke and major bleeding. The aim of our study is to test the safety of edoxaban 30 mg/day in patients with severe renal impairment with an estimated glomerular filtration rate (eGFR) of 15–29 mL/min.
Methods
We analyzed retrospective data from 46 patients who had documented AF with severe renal impairment (eGFR between 15 and 29 mL/min). The follow-up, characterized by clinical examination and blood analysis, was performed at 3, 6, and 12 months. The main endpoint was the incidence of major bleedings or clinically relevant non-major (CRNM) bleedings or thromboembolic events.
Results
At the time of the data collection, the average follow-up was 9.13 ± 3.0 months. There were no major bleedings, strokes, systemic embolisms, or cardiovascular deaths reported: one non-cardiac death and five minor hemorrhages occurred. No differences related to the severity of CKD were observed in the left ventricular ejection fraction at echocardiography and in the thrombotic and hemorrhagic risk profile.
Conclusion
In this explorative study analyzing patients with severe CKD treated with edoxaban 30 mg once daily, no major bleeding or thrombotic events were observed. Some minor bleedings were observed. While additional studies are necessary to confirm the results of this exploratory study, edoxaban 30 mg once daily appears to be safe in patients with severe CKD.
Similar content being viewed by others
In this explorative retrospective study analyzing patients with severe chronic kidney disease (CKD) (estimated glomerular filtration rate 15–29 mL/min) treated with edoxaban 30 mg once daily, no major bleeding or thrombotic events were observed. |
Only minor bleedings were observed, not related to the severity of CKD; therefore, edoxaban 30 mg appears to be safe in patients with severe CKD. |
Additional studies or registries are necessary to confirm this exploratory study. |
1 Introduction
Atrial fibrillation (AF) is the most common arrhythmia in the general population and is one of the strongest risk factors for ischemic stroke and an independent predictor of death. Patients with AF and advanced chronic kidney disease (CKD) with a glomerular filtration rate (GFR) < 30 mL/min or who are on dialysis are at high risk of adverse events and are complicated to manage [1]. Several studies indicate that the combination of end-stage renal failure and AF confers a significantly greater risk of both thromboembolic and hemorrhagic events that increase as kidney function worsens [2].
According to the American Heart Association, American College of Cardiology, and Heart Rhythm Society guidelines for the management of patients with AF, patients with moderate or moderate-to-severe CKD (GFR 15–50 mL/min) can be treated with reduced doses of direct thrombin or factor Xa inhibitors, but safety and efficacy have not been established in patients with severe renal impairment. For end-stage kidney disease [estimated GFR (eGFR) < 15 mL/min] or hemodialysis, it is reasonable to prescribe warfarin [international normalized ratio (INR) 2.0–3.0] [3]. Although patients with advanced CKD are at higher risk of stroke, this risk has not been significantly modified by warfarin, with a lower margin of benefit due to uremia-induced platelet dysfunction or warfarin-induced nephropathy [4]. For these reasons, it becomes crucial to choose an anticoagulant regimen that is associated with a more favorable net clinical outcome than warfarin.
A dose reduction is recommended for all non-vitamin K oral anticoagulants (NOACs) in the setting of moderate to severe renal dysfunction [5]. The recent European Society of Cardiology guidelines indicate that the use of NOACs has not been tested in patients with a GFR < 30 mL/min, and there is very little evidence regarding the effects of NOACs in patients on hemodialysis or on other forms of renal replacement therapy [1].
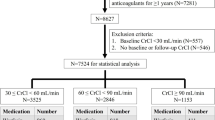
Kidneys clear approximately 50% of unmetabolized edoxaban, which is the most recently approved factor Xa inhibitor. Total drug exposure increases by 32%, 74%, and 72% in patients with mild, moderate, and severe renal impairment, respectively [6]. In patients with moderate CKD in the ENGAGE AF-TIMI 48 (Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation–Thrombolysis in Myocardial Infarction 48) trial, edoxaban showed similar efficacy to warfarin in preventing stroke but offered a lower risk of bleeding and cardiovascular death [7]. In this trial, the edoxaban dose was reduced by 50% in patients with moderate renal impairment, while patients with severe renal impairment were excluded. Moreover, in a post hoc analysis for patients on edoxaban (vs. warfarin) whose creatinine clearance (CLCR) fell below 30 mL/min after baseline (n = 1202), stroke (2.36 vs. 1.89 events per 100 patient-years) and major bleeding (6.83 vs. 6.49 events per 100 patient-years) rates were similar [8]. In addition, a recent short-term study in Japanese non-valvular AF (NVAF) patients with severe renal impairment (GFR 15–29 mL/min), edoxaban 15 mg once daily exhibited a similar safety and bioavailability profile to the 30 and 60 mg doses in patients with normal renal function [9]. However, complete information regarding the safety and efficacy of edoxaban in patients with AF and severe CKD is still missing.
Therefore, we hypothesized that edoxaban 30 mg/day treatment will be safe in patients with severe impairment of renal function and an eGFR of 15–29 mL/min.
2 Patients and Methods
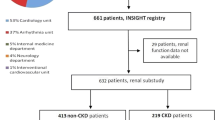
The data for the present study were retrospectively obtained from consecutive patients evaluated for AF in two high-volume Italian cardiological centers by analyzing the reports of patients with NVAF who were included in the Italian Registry of Drugs (AIFA registry). Selected patients received a prescription for edoxaban 30 mg daily with at least 6 months of follow-up between October 2016 and October 2017.
The inclusion criteria were patients with at least one episode of documented AF of any duration in the preceding 12 months; a CHA2DS2-VASc [Congestive heart failure, Hypertension, Age ≥ 75 years, Diabetes mellitus, previous Stroke/transient ischemic attack [double weight]–Vascular disease, Age 65–74 years, (female) Sex category] score of ≥ 2; any type of NVAF; age > 18 years; and severe renal impairment with an eGFR between 15 and 29 mL/min, calculated using the Cockroft–Gault formula. Patients were classified as having paroxysmal AF (episodes of AF for < 7 days), persistent AF (duration 1 week to 1 year), or permanent AF (duration ≥ 1 year or failed electric cardioversion), as defined by the AF guidelines [1]. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration. Informed consent was obtained from all individual participants included in the study, who consented to the analysis and storage of their data in the AIFA registry. Due to the retrospective nature of the study, the ethical committees were retrospectively informed of the present study.
The exclusion criteria were eGFR < 15 or > 29 mL/min; concomitant use of P-glycoprotein inhibitors such as erythromycin, cyclosporine (ciclosporin), dronedarone, or ketoconazole; a high risk of bleeding; use of dual antiplatelet therapy; moderate to severe mitral stenosis; other indications for anticoagulation different from AF; acute coronary syndrome or coronary revascularization; or stroke within 30 days.
Standard two-dimensional transthoracic echocardiographic examination with second harmonic mode was performed with an Aloka ProSound Alpha-6 Ultrasound System (Aloka Co., Ltd, Tokyo, Japan) and an iE33 Ultrasound System and S4 Ultrasound Probe (Philips Medical Systems, Andover, MA, USA). Left ventricular end-diastolic volume, end-systolic volume, and ejection fraction (LVEF) were measured using the modified Simpson’s rule from the apical view.
Follow-up, characterized by clinical examination and blood analysis, was performed at 3, 6, and 12 months.
The main endpoint was the incidence of major bleedings according to the International Society on Thrombosis and Haemostasis definition [10], or clinically relevant non-major (CRNM) bleedings or thromboembolic events such as adverse drug reactions, ischemic or hemorrhagic stroke, systemic embolism, and cardiovascular death. A secondary safety endpoint was total minor bleedings.
3 Statistical analysis
All patients’ follow-up data were blinded and analyzed with the SPSS® Statistics 24.0 (IBM, Armonk, NY, USA) software.
Patients were analyzed for occurrence of events and for main clinical and laboratory characteristics as well as concomitant medications.
4 Results
The main clinical and laboratory characteristics as well as concomitant medications for the 46 patients in the study are shown in the Table 1. Among them, 16 (34.8%) utilized anticoagulation prior to edoxaban (seven warfarin, one dabigatran, six rivaroxaban, two apixaban). The main clinical and laboratory data from the two groups with more severe CKD (15–22 mL/min) and less severe CKD (23–29 mL/min) are also listed.
At the time of the data collection, the average follow-up was 9.13 ± 3.0 months. There were no major bleedings, strokes, systemic embolisms, or cardiovascular deaths reported. In the more severe CKD group (15–22 mL/min), one non-cardiac death (terminal neoplasy) and three minor hemorrhages (two hematuria and one epistaxis, none of which required blood transfusion or hospital admission) occurred. In the less severe CKD group (23–29 mL/min), two minor hemorrhages (one rectal bleeding and one epistaxis, neither requiring blood transfusion or hospital admission) occurred (Fig. 1). No differences among the two groups were observed in LVEF at echocardiography and in the thrombotic and hemorrhagic risk profile (mean CHA2DS2-Vasc and HAS-BLED [Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile INR, Elderly, Drugs/alcohol concomitantly] scores).
There were no significant differences in minor hemorrhages or in eGFR among the 20 patients with a CHA2DS2-Vasc score of 2 and 3 and the 26 patients with a CHA2DS2-Vasc score > 3; the LVEF was significantly higher in patients with a lower CHA2DS2-Vasc (51.0 ± 6.4% vs. 43.8 ± 12.5%; p < 0.05) due to the presence in the second group of 12 patients with an ejection fraction < 45% because of ischemic (nine) or primary dilated (three) cardiomyopathy.
Detailed data from the five patients with minor hemorrhages are listed in Table 2, with no differences observed in LVEF or left atrial dimension at echocardiography, body surface area, and the thrombotic and hemorrhagic risk profile (mean CHA2DS2-Vasc and HAS-BLED scores).
All patients remained on edoxaban during follow-up, except for temporary interruptions in four patients for minor procedures (dental extractions).
5 Discussion
CKD is typically classified according to severity, diagnosis, treatment, and prognosis. The Kidney Disease Quality Outcome Initiative retains a classification based on five progressively more severe stages, based on GFR [11]. The CKD prevalence in the five stages, as estimated by the National Health and Nutrition Examination Surveys, decreases dramatically with the progression of CKD stages, from 4.3% in stage 3 (moderate CKD) to 0.2% in stage 4 (severe CKD); both stages increase with risk factors such as age, hypertension, heart failure, coronary artery disease, valvular heart disease, obesity, and diabetes mellitus [12].
Since these are the same risk factors that cause AF, the prevalence of AF is two to three times higher in patients with severe CKD (GFR of 15–29 mL/min) than in moderate CKD or normal renal function, independent of other known risk factors for AF [13, 14]. This strong linkage depends not only on the common risk factors but also on pathophysiological explanation. Individuals with CKD are at higher risk of developing hypertension, left ventricular hypertrophy, inflammation, and cardiovascular disease; in addition, CKD can also lead to alterations in the renin–angiotensin–aldosterone system and sympathetic activation, which may produce atrial fibrosis and increase the risk of AF [15, 16]. Recent studies have tried to identify the different interactions between CKD and AF, highlighting the prognostic role of renal damage markers in the incidence of AF, such as the presence of albuminuria, which is strongly and independently associated with the incidence of AF [14], or of fibroblast growth factor 23, which is elevated in patients with mild to severe CKD and independently associated with AF through cardiac remodeling, diastolic dysfunction, left ventricular hypertrophy, atrial enlargement, and clinical heart failure [17]. Additionally, elevated levels of inflammatory markers have been reported in CKD even in its early stages [18, 19], underlining that inflammation plays a significant role in predicting progression of kidney dysfunction and in the pathogenesis of AF [20, 21]. Imaging techniques such as echocardiography could be helpful to evaluate morphological and functional cardiac indicators of thromboembolic risk in patients with CKD [22,23,24], especially in cases of treatment with vitamin K antagonists out of therapeutic range or with NOACs in the presence of poor compliance [25, 26].
Moreover, patients with AF and advanced CKD or who are on dialysis have a significantly higher risk of stroke and other adverse events. Although an eGFR < 60 mL/min is indicative of moderate CKD, all four pivotal trials of NOACs in AF patients used an eGFR < 50 mL/min (estimated using the Cockroft-Gault formula) to define moderate CKD, and often adjusted anticoagulant dosage based on this single value [27]. Additionally, patients with end-stage renal disease—particularly those on hemodialysis—are also at an increased risk of bleeding [28]. Warfarin and NOACs have been shown to be effective in preventing stroke and to have a low rate of major bleeding when used in AF patients with moderate CKD [29]. Despite the large number of patients studied, the large randomized trials of antithrombotic therapy in patients with AF have typically excluded those who have moderate-to-severe CKD [30,31,32], and the treatment of these patients has been based on data obtained from smaller observational studies [33].
Concerning the warfarin treatment in AF patients with severe CKD, data are controversial. A recent analysis from Danish registries found warfarin to be beneficial for stroke prevention in patients with CKD, showing lower risks of all-cause mortality and cardiovascular death with no increased risk of hemorrhagic stroke or major bleeding with warfarin when compared with no antithrombotic therapy [34]. Contrary to these findings, a retrospective analysis by a Canadian group demonstrated a higher risk of bleeding with warfarin than with no warfarin [35]. This finding is supported by a large Swedish database, in which stroke risk was lower while bleeding was slightly increased in CKD patients with AF treated with warfarin, especially during therapy initiation [36].
Moreover, warfarin treatment in AF patients with CKD presents additional risks (e.g., inducing vascular calcification may possibly have a detrimental effect on renal function) that are less common in the non-CKD population. In addition, vitamin K antagonists have been shown to accelerate pre-existing vascular calcifications, whereas vitamin K substitution has been shown to improve these processes [8, 37]. Böhm et al. [38] demonstrated via an analysis of the RE-LY (Randomized Evaluation of Long-term Anticoagulation Therapy) trial that there was a greater decline in renal function at 30 months of follow-up in elderly patients with AF treated with warfarin than in those treated with dabigatran [38]. These findings agree with animal studies showing induction of nephropathy with high doses of warfarin [39].
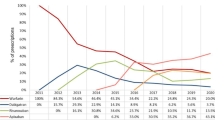
Thus, it is critical for patients with CKD to choose an anticoagulant regimen associated with a more favorable net clinical outcome than warfarin. NOACs have emerged as a promising alternative to warfarin for the prevention of stroke and systemic thromboembolism. Contemporary trials of apixaban, dabigatran, edoxaban, and rivaroxaban showed efficacy and safety that were comparable or superior to warfarin in patients with AF and moderate CKD. Specifically, analyses of dabigatran versus warfarin in the RE-LY trial and apixaban versus warfarin in the ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial found no difference in efficacy in subgroups defined by a GFR ≤ 50, 50–80, or > 80 mL/min [30, 40]. In the ARISTOTLE trial, the major bleeding rate in patients with moderate renal impairment was lower with apixaban than with warfarin [40]. Similarly, major bleeding was similar with dabigatran (both doses) and warfarin in the RE-LY trial [30]. In the analysis of rivaroxaban versus warfarin in patients with moderate GFR and mild or no renal dysfunction, no difference in efficacy was observed [31].
In the ENGAGE AF-TIMI 48 trial, patients with AF with a GFR > 50 mL/min received edoxaban 60 mg, or 30 mg if their GFR was between 30 and 50 mL/min, their body weight was < 60 kg, or a strong P-glycoprotein inhibitor was coadministered. Edoxaban was non-inferior in preventing stroke and systemic embolism and superior in preventing major bleeding (hazard ratio: 0.80; 95% confidence interval 0.71–0.91) compared with warfarin in all subgroups of the trial [7].
Available data concerning severe renal impairment in AF are few and disorganized. In the ENGAGE AF-TIMI 48, ROCKET AF (Rivaroxaban—Once daily, oral, direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation), RE-LY, and ARISTOTLE trials severe renal impairment was an exclusion criterion [7, 30, 31, 40].
A post hoc analysis of the ENGAGE-AF TIMI48 trial data for patients whose CLCR fell below 30 mL/min after baseline (n = 1202) showed a trend of higher effectiveness of edoxaban than warfarin on stroke (2.36 vs. 1.89 events per 100 patient-years) and on major bleeding (6.83 vs. 6.49 events per 100 patient-years) rates [8].
A recent analysis by Koretsune et al. [9] evaluated the short-term safety and drug plasma concentrations of a NOAC in Japanese patients. The analysis found that edoxaban 15 mg once daily in patients with severe CKD did not markedly increase bleeding compared with patients with normal renal function who received edoxaban 30 or 60 mg once daily for 12 weeks. This suggests that these patients receiving edoxaban 15 mg may have similar bleeding risks as patients receiving the conventional edoxaban regimen [9].
However, to our knowledge, the present explorative retrospective study analysis is the largest retrospective analysis in patients with severe CKD (eGFR 15–29 mL/min) treated with NOACs. Despite a sample size too small to detect sufficient major or CRNM bleedings, the absence of these primary endpoints in patients with severe CKD treated with edoxaban 30 mg gives us a sign of safety. No other main endpoints—such as ischemic or hemorrhagic stroke, systemic embolism, cardiovascular death, and severe adverse drug reactions—were observed.
Some minor bleeding was observed in all groups regardless of CKD status. Concomitant drugs did not significantly influence the rate of minor bleedings.
6 Limitations
The limitations of the present study are the analysis performed in only two centers, the retrospective nature of the study, and the small sample size.
The sample size studied is too small and the observation period is short (average 9.3 months) to detect a sufficient number of major bleedings or CRNM bleedings; however, despite the presence of advanced age and high CHA2DS2-VASc and HAS-BLED scores, the edoxaban 30 mg once-daily treatment was safe, without incidences of the main safety endpoint (major bleedings or CRNM bleedings) at follow-up. A control group of patients who received warfarin anticoagulation therapy is missing, due to the very low prevalence of patients with severe CKD compared with moderate to severe CKD.
7 Conclusions
In this explorative retrospective study analyzing patients with severe CKD (eGFR 15–29 mL/min) treated with edoxaban 30 mg once daily, no major bleeding or thrombotic events were observed. Some minor bleedings were observed, but these were not related to the severity of CKD. While additional studies are necessary to confirm this exploratory study, edoxaban 30 mg once daily appears to be safe in patients with severe CKD.
References
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar Dan, et al. ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;2016(37):2893–962.
Go AS, Fang MC, Udaltsova N, Chang Y, Pomernacki NK, Borowsky L, et al. Impact of proteinuria and glomerular filtration rate on risk of thromboembolism in atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Circulation. 2009;119:1363–9.
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:2246–80.
Brodsky SV, Nadasdy T, Rovin BH, et al. Warfarin-related nephropathy occurs in patients with and without chronic kidney disease and is associated with an increased mortality rate. Kidney Int. 2011;80:181–9.
Steffel J, Verhamme P, Potpara TS, ESC Scientific Document Group, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1330–93.
Parasrampuria DA, Truitt KE. Pharmacokinetics and pharmacodynamics of edoxaban, a non-vitamin K antagonist oral anticoagulant that inhibits clotting factor Xa. Clin Pharmacokinet. 2016;55:641–55.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. ENGAGE AF-TIMI 48 Investigators. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104.
Chan KE, Giugliano RP, Patel MR, Abramson S, Jardine M, Zhao S, et al. Nonvitamin K anticoagulant agents in patients with advanced chronic kidney disease or on dialysis with AF. J Am Coll Cardiol. 2016;67(24):2888–99.
Koretsune Y, Yamashita T, Kimura T, Fukuzawa M, Abe K, et al. Short-term safety and plasma concentrations of edoxaban in Japanese patients with non-valvular atrial fibrillation and severe renal impairment. Circ J. 2015;79(7):1486–95.
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–4.
Levey AS, Eckardt KU, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int. 2005;67(6):2089–100.
Snyder JJ, Foley RN, Collins AJ. Prevalence of CKD in the United States: a sensitivity analysis using the National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2009;53(2):218–28.
Baber U, Howard VJ, Halperin JL, Soliman EZ, Zhang X, McClellan W, et al. Association of chronic kidney disease with atrial fibrillation among adults in the United States: REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Circ Arrhythm Electrophysiol. 2011;4:26–32.
Alonso A, Lopez FL, Matsushita K, Loehr LR, Agarwal SK, et al. Chronic kidney disease is associated with the incidence of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011;123:2946–53.
Ehrlich JR, Hohnloser SH, Nattel S. Role of angiotensin system and effects of its inhibition in atrial fibrillation: clinical and experimental evidence. Eur Heart J. 2006;27:512–8.
Schlaich MP, Socratous F, Hennebry S, Eikelis N, Lambert EA, Straznicky, et al. Sympathetic activation in chronic renal failure. J Am Soc Nephrol. 2009;20:933–9.
Mehta R, Cai X, Lee J, Scialla JJ, Bansal N, Sondheimer JH, Chronic Renal Insufficiency Cohort (CRIC) Study Investigators, et al. Association of fibroblast growth factor 23 with atrial fibrillation in chronic kidney disease, from the Chronic Renal Insufficiency Cohort Study. JAMA Cardiol. 2016;1(5):548–56.
Shlipak MG, Fried LF, Crump C, et al. Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation. 2003;107:87–92.
Amdur RL, Mukherjee M, Go A, Barrows IR, Ramezani A, et al. Interleukin-6 is a risk factor for atrial fibrillation in chronic kidney disease: findings from the CRIC study. PLoS One. 2016;11(2):e0148189.
Chung MK, Martin DO, Sprecher D, et al. C-reactive protein elevation in patients with atrial arrhythmias: inflammatory mechanisms and persistence of atrial fibrillation. Circulation. 2001;104:2886–91.
Aviles RJ, Martin DO, Apperson-Hansen C, et al. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003;108:3006–30010.
Sorino M, Colonna P, De Luca L, Carerj S, Oliva E, De Tommasi SM, et al. Post-cardioversion transesophageal echocardiography (POSTEC) strategy with the use of enoxaparin for brief anticoagulation in atrial fibrillation patients: the multicenter POSTEC trial (a pilot study). J Cardiovasc Med (Hagerstown). 2007;8(12):1034–42.
de Luca I, Colonna P, Sorino M, Del Salvatore B, De Luca L. New monodimensional transthoracic echocardiographic sign of left atrial appendage function. J Am Soc Echocardiogr. 2007;20(3):324–32. https://doi.org/10.1016/j.echo.2006.08.030.
de Luca I, Sorino M, De Luca L, Colonna P, Del Salvatore B, Corlianò L. Pre- and post-cardioversion transesophageal echocardiography for brief anticoagulation therapy with enoxaparin in atrial fibrillation patients: a prospective study with a 1-year follow-up. Int J Cardiol. 2005;102(3):447–54.
Colonna P, Dentamaro I. Echocardiography in patients undergoing cardioversion for atrial fibrillation and inadequate anticoagulation: a step beyond towards maximum safety! Pol Arch Intern Med. 2017;127(7–8):468–70.
Dentamaro I, Vestito D, Michelotto E, De Santis D, Ostuni V, et al. Evaluation of left atrial appendage function and thrombi in patients with atrial fibrillation: from transthoracic to real time 3D transesophageal echocardiography. Int J Cardiovasc Imaging. 2017;33(4):491–8.
Roldán V, Marín F, Fernández H, Manzano-Fernández S, Gallego P, et al. Renal impairment in a “real-life” cohort of anticoagulated patients with atrial fibrillation (implications for thromboembolism and bleeding). Am J Cardiol. 2013;111(8):1159–64.
Qamar A, Bhatt DL. Stroke prevention in atrial fibrillation in patients with chronic kidney disease. Circulation. 2016;133(15):1512–5.
Olesen JB, Lip GY, Kamper AL, Hommel K, Køber L, et al. Stroke and bleeding in atrial fibrillation with chronic kidney disease. N Engl J Med. 2012;367(7):625–35.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Rocket AF, Study Investigators. Rivaroxaban—once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation: rationale and design of the ROCKET AF study. Am Heart J. 2010;159:340–7.
Marinigh R, Lane DA, Lip GY. Severe renal impairment and stroke prevention in atrial fibrillation: implications for thromboprophylaxis and bleeding risk. J Am Coll Cardiol. 2011;57:1339–48.
Yang F, Chou D, Schweitzer P, Hanon S. Warfarin in haemodialysis patients with atrial fibrillation: what benefit? Europace. 2010;12:1666–72.
Bonde AN, Lip GY, Kamper AL, Hansen PR, Lamberts M, et al. Net clinical benefit of antithrombotic therapy in patients with atrial fibrillation and chronic kidney disease: a nationwide observational cohort study. J Am Coll Cardiol. 2014;64(23):2471–82.
Shah M, Avgil Tsadok M, Jackevicius CA, Essebag V, Eisenberg MJ, et al. Warfarin use and the risk for stroke and bleeding in patients with atrial fibrillation undergoing dialysis. Circulation. 2014;129:1196–203.
Friberg L, Benson L, Lip GY. Balancing stroke and bleeding risks in patients with atrial fibrillation and renal failure: the Swedish Atrial Fibrillation Cohort study. Eur Heart J. 2015;36(5):297–306.
Schurgers LJ, Joosen IA, Laufer EM, Chatrou ML, Herfs M, Winkens MH, et al. Vitamin K-antagonists accelerate atherosclerotic calcification and induce a vulnerable plaque phenotype. PLoS One. 2012;7(8):e43229.
Böhm M, Ezekowitz MD, Connolly SJ, Eikelboom JW, Hohnloser SH, et al. Changes in renal function in patients with atrial fibrillation: an analysis from the RE-LY trial. J Am Coll Cardiol. 2015;65(23):2481–93.
Ware K, Brodsky P, Satoskar AA, et al. Warfarin-related nephropathy modeled by nephron reduction and excessive anticoagulation. J Am Soc Nephrol. 2011;22:1856–62.
Granger CB, Alexander JH, McMurray JJV, Lopes RD, Hylek EM, Hanna M, ARISTOTLE Committees and Investigators, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was provided for the present spontaneous research. Daiichi Sankyo funded the editorial technical language assistance in the manuscript preparation, according to the journal guidelines, and the open access fee for this manuscript.
Conflict of interest
The authors provide a full disclosure of real or perceived conflicts of interest as related to the specific content of this article. The opinions expressed in this article reflect the opinions of the authors. Giovanni Fazio, MD: no conflict to disclose. Ilaria Dentamaro, MD: payment as an individual for consulting fees from Daiichi Sankyo. Rosanna Gambacurta, MD: employee in the Medical Department of Daiichi Sankyo Italy. Pasquale Alcamo, MD: no conflict to disclose. Paolo Colonna, MD: co-author of the European Society of Cardiology (ESC) guidelines on atrial fibrillation (version 2010) and has received honoraria and institutional funds for trials from Bayer, Boehringer, Pfizer, and Daichii-Sankyo.
Ethics approval
All procedures in this study were in accordance with the 1964 Helsinki Declaration (and its amendments), and the institutional review board approved the study with data retrospectively obtained by analyzing the reports of patients included in the Italian Registry of Drugs (AIFA registry), with a written informed consent obtained from patients, parents, or caregivers.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Fazio, G., Dentamaro, I., Gambacurta, R. et al. Safety of Edoxaban 30 mg in Elderly Patients with Severe Renal Impairment. Clin Drug Investig 38, 1023–1030 (2018). https://doi.org/10.1007/s40261-018-0693-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-018-0693-6