Abstract
Background
Budget impact analyses (BIAs) describe changes in intervention- and disease-related costs of new technologies. Evidence on the quality of BIAs for cancer screening is lacking.
Objectives
We systematically reviewed the literature and methods to assess how closely BIA guidelines are followed when BIAs are performed for cancer-screening programs.
Data sources
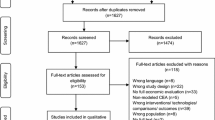
Systematic searches were conducted in MEDLINE, EMBASE, EconLit, CRD (Centre for Reviews and Dissemination, University of York), and CEA registry of the Tufts Medical Center.
Study eligibility criteria
Eligible studies were BIAs evaluating cancer-screening programs published in English, 2010–2018.
Synthesis methods
Standardized evidence tables were generated to extract and compare study characteristics outlined by the ISPOR BIA Task Force.
Results
Nineteen studies were identified evaluating screening for breast (5), colorectal (6), cervical (3), lung (1), prostate (3), and skin (1) cancers. Model designs included decision-analytic models (13) and simple cost calculators (6). From all studies, only 53% reported costs for a minimum of 3 years, 58% compared to a mix of screening options, 42% reported model validation, and 37% reported uncertainty analysis for participation rates. The quality of studies appeared to be independent of cancer site.
Limitations
“Gray” literature was not searched, misinterpretation is possible due to limited information in publications, and focus was on international methodological guidelines rather than regional guidelines.
Conclusions
Our review highlights considerable variability in the extent to which BIAs evaluating cancer-screening programs followed recommended guidelines. The annual budget impact at least over the next 3–5 years should be estimated. Validation and uncertainty analysis should always be conducted. Continued dissemination efforts of existing best-practice guidelines are necessary to ensure high-quality analyses.
Similar content being viewed by others
References
Mauskopf JA, Sullivan SD, Annemans L, Caro J, Mullins CD, Nuijten M, Orlewska E, Watkins J, Trueman P. Principles of good practice for budget impact analysis: report of the ISPOR Task Force on good research practices—budget impact analysis. Value Health. 2007;10(5):336–47.
Trueman P, Drummond M, Hutton J. Developing guidance for budget impact analysis. Pharmacoeconomics. 2001;19(6):609–21.
Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, Orlewska E, Penna P, Rodriguez Barrios JM, Shau WY. Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health. 2014;17(1):5–14.
Organization WH. Cancer fact sheet N°297”. 2014.
Malvezzi M, Carioli G, Bertuccio P, Boffetta P, Levi F, La Vecchia C, Negri E. European cancer mortality predictions for the year 2017, with focus on lung cancer. Ann Oncol. 2017;28(5):1117–23.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30.
Organization WH. World cancer report 2014. 2014.
Smith RA, Andrews K, Brooks D, DeSantis CE, Fedewa SA, Lortet-Tieulent J, Manassaram-Baptiste D, Brawley OW, Wender RC. Cancer screening in the United States, 2016: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2016;66(2):96–114.
Andermann A, Blancquaert I, Beauchamp S, Dery V. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull World Health Organ. 2008;86(4):317–9.
Rawlins M. Paying for modern cancer care–a global perspective. Lancet Oncol. 2007;8(9):749–51.
(PBAC). PBAC. Guidelines for preparing a submission to the PBAC. Version 5. Draft for public consultation. 2016.
Neyt M, Cleemput I, Sande SV, Thiry N. Belgian guidelines for budget impact analyses. Acta Clin Belg. 2015;70(3):175–80.
van de Vooren K, Duranti S, Curto A, Garattini L. A critical systematic review of budget impact analyses on drugs in the EU countries. Appl Health Econ Health Policy. 2014;12(1):33–40.
(NICE) NIfHaCE. Guide to the methods of economic appraisal 2013. 2013.
Mauskopf J, Earnshaw S. A methodological review of US budget—impact models for new drugs. Pharmacoeconomics. 2016;34(11):1111–31.
Mauskopf JA, Earnshaw S, Mullins CD. Budget impact analysis: review of the state of the art. Expert Rev Pharmacoecon Outcomes Res. 2005;5(1):65–79.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Wright T, Huang J, Baker E, Garfield S, Hertz D, Cox JT. The budget impact of cervical cancer screening using HPV primary screening. Am J Manag Care. 2016;22(3):e95–105.
Pil L, Hoorens I, Vossaert K, Kruse V, Tromme I, Speybroeck N, Annemans L, Brochez L. Cost-effectiveness and budget effect analysis of a population-based skin cancer screening. JAMA Dermatol. 2016;153(2):147–53. https://doi.org/10.1001/jamadermatol.2016.4518.
Pil L, Fobelets M, Putman K, Trybou J, Annemans L. Cost-effectiveness and budget impact analysis of a population-based screening program for colorectal cancer. Eur J Intern Med. 2016;32:72–8.
Arrospide A, Rue M, van Ravesteyn NT, Comas M, Soto-Gordoa M, Sarriugarte G, Mar J. Economic evaluation of the breast cancer screening programme in the Basque Country: retrospective cost-effectiveness and budget impact analysis. BMC Cancer. 2016;16:344.
Bonafede MM, Kalra VB, Miller JD, Fajardo LL. Value analysis of digital breast tomosynthesis for breast cancer screening in a commercially-insured US population. Clinicoecon Outcomes Res. 2015;7:53–63.
Comas M, Arrospide A, Mar J, Sala M, Vilaprinyo E, Hernandez C, Cots F, Martinez J, Castells X. Budget impact analysis of switching to digital mammography in a population-based breast cancer screening program: a discrete event simulation model. PLoS One. 2014;9(5):e97459.
Liss DT, French DD, Buchanan DR, Brown T, Magner BG, Kollar S, Baker DW. Outreach for annual colorectal cancer screening: a budget impact analysis for community health centers. Am J Prev Med. 2016;50(2):e54–61.
Goulart BH, Bensink ME, Mummy DG, Ramsey SD. Lung cancer screening with low-dose computed tomography: costs, national expenditures, and cost-effectiveness. J Natl Compr Cancer Netw. 2012;10(2):267–75.
Nichol MB, Wu J, An JJ, Huang J, Denham D, Frencher S, Jacobsen SJ. Budget impact analysis of a new prostate cancer risk index for prostate cancer detection. Prostate Cancer Prostatic Dis. 2011;14(3):253–61.
Shi JF, Chen JF, Canfell K, Feng XX, Ma JF, Zhang YZ, Zhao FH, Li R, Ma L, Li ZF, Lew JB, Ning Y, Qiao YL. Estimation of the costs of cervical cancer screening, diagnosis and treatment in rural Shanxi Province, China: a micro-costing study. BMC Health Serv Res. 2012;12:123.
Kim B, Lairson DR, Chung TH, Kim J, Shokar NK. Budget impact analysis of against colorectal cancer in our neighborhoods (ACCION): a successful community-based colorectal cancer screening program for a medically underserved minority population. Value Health. 2017;20(6):809–18.
Lew JB, St John DJB, Xu XM, Greuter MJE, Caruana M, Cenin DR, He E, Saville M, Grogan P, Coupe VMH, Canfell K. Long-term evaluation of benefits, harms, and cost-effectiveness of the National Bowel Cancer Screening Program in Australia: a modelling study. Lancet Public Health. 2017;2(7):e331–40.
Miller JD, Bonafede MM, Herschorn SD, Pohlman SK, Troeger KA, Fajardo LL. Value analysis of digital breast tomosynthesis for breast cancer screening in a US medicaid population. J Am Coll Radiol. 2017;14(4):467e5–474.e5.
Movik E, Dalsbo TK, Fagelund BC, Friberg EG, Haheim LL, Skar A. NIPH Systematic reviews. Digital breast tomosynthesis with hologic 3d mammography selenia dimensions system for use in breast cancer screening: a single technology assessment. Oslo, Norway: Knowledge Centre for the Health Services at The Norwegian Institute of Public Health (NIPH) Copyright (c) 2017 by The Norwegian Institute of Public Health (NIPH). 2017.
Voigt JD, Dong Y, Linder V, Zappala S. Use of the 4Kscore test to predict the risk of aggressive prostate cancer prior to prostate biopsy: Overall cost savings and improved quality of care to the us healthcare system. Rev Urol. 2017;19(1):1–10.
Petry KU, Barth C, Wasem J, Neumann A. A model to evaluate the costs and clinical effectiveness of human papilloma virus screening compared with annual papanicolaou cytology in Germany. Eur J Obstet Gynecol Reprod Biol. 2017;212:132–9.
Murphy J, Halloran S, Gray A. Cost-effectiveness of the faecal immunochemical test at a range of positivity thresholds compared with the guaiac faecal occult blood test in the NHS Bowel Cancer Screening Programme in England. BMJ Open. 2017;7(10):e017186.
Sweet A, Lee D, Gairy K, Phiri D, Reason T, Lock K. The impact of CT colonography for colorectal cancer screening on the UK NHS: costs, healthcare resources and health outcomes. Appl Health Econ Health Policy. 2011;9(1):51–64.
Goto D, Rosser C, Kim C. Budget impact model for the use of PCA3 urine testing in prostate cancer screening. Urol Pract. 2015;2(6):298–303.
Cleemput I, Neyt M, Van de Sande S, Thiry N. Belgian guidelines for economic evaluations and budget impact analyses. 2nd ed. Brussels: Belgian Health Care Knowledge Centre (KCE); 2012.
Baltussen R, Leidl R, Ament A. Real world designs in economic evaluation. Bridging the gap between clinical research and policy-making. Pharmacoeconomics. 1999;16(5 Pt 1):449–58.
Organization WH. Health impact assessment.
Giersiepen K, Hense HW, Klug SJ, Antes G, Zeeb H. Planning, implementation and evaluation of cancer screening programs. Z Arztl Fortbild Qualitatssich. 2007;101(1):43–9.
Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K. False-negative results in screening programmes: systematic review of impact and implications. Health Technol Assess. 2000;4(5):1–120.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Augustovski F, Briggs AH, Mauskopf J, Loder E. Consolidated health economic evaluation reporting standards (CHEERS) statement. Int J Technol Assess Health Care. 2013;29(2):117–22.
Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol. 2015;3:32.
Lobb R, Colditz GA. Implementation science and its application to population health. Annu Rev Public Health. 2013;34:235–51.
McIsaac JL, Warner G, Lawrence L, Urquhart R, Price S, Gahagan J, McNally M, Jackson LA. The application of implementation science theories for population health: a critical interpretive synthesis. AIMS Public Health. 2018;5(1):13–30.
Centers for Medicare and Medicaid Services. Medicaid managed care enrollment and program characteristics 2014. https://www.medicaid.gov/medicaid-chip-program-information/by-topics/data-and-systems/medicaid-managed-care/downloads/2014-medicaidmanaged-care-enrollment-report.pdf. Accessed 7 Sept 2018.
Centers for Medicare and Medicaid Services, Medicaid Statistical Information System. FY2012 MSIS State Summary DataMart, “Table 12 FY 2012 Medicaid Beneficiaries by Age Group” and “Table 13 FY 2012 Medicaid Beneficiaries by Gender.”. https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidDataSourcesGenInfo/MSIS-Tables.html. Accessed 7 Sept 2018.
Arrospide A, Rue M, van Ravesteyn NT, Comas M, Larranaga N, Sarriugarte G, Mar J. Evaluation of health benefits and harms of the breast cancer screening programme in the Basque Country using discrete event simulation. BMC Cancer. 2015;15:671.
Truven Health Analytics, Inc. Truven Health Analytics MarketScan® Research Databases. http://truvenhealth.com/your-healthcare-focus/analytic-research/marketscan-research-databases. Accessed 7 Sept 2018.
Bonafede MM, Miller JD, Lenhart GM, Nelson J, Fajardo LL. Health insurer burden of patient recall following breast cancer screening mammography. Value in Health. 2014;17(3):A82.
INEbase. Instituto Nacional de Estadística website. http://www.ine.es/. Accessed 7 Sept 2018.
ACCION database. El Paso, TX: Texas Tech University Health Science Center, 2014.
Shokar NK, Byrd T, Lairson DR, Salaiz R, Kim J, Calderon-Mora J, Nguyen N, Ortiz M. Against colorectal cancer in our neighborhoods, a community-based colorectal cancer screening program targeting low-income hispanics: program development and costs. Health Promot Pract. 2015;16(5):656–66.
Australian Bureau of Statistics. 3101.0—Australian Demographic Statistics, Sept 2014. 2015. http://www.abs.gov.au/AUSSTATS. Accessed 7 Sept 2018.
Australian Bureau of Statistics. 3222.0—Population Projections, Australia, 2012 (base) to 2101. 2013. http://www.abs.gov.au/AUSSTATS. Accessed 7 Sept 2018.
Kuntz KM, Lansdorp-Vogelaar I, Rutter CM, Knudsen AB, van Ballegooijen M, Savarino JE, Feuer EJ, Zauber AG. A systematic comparison of microsimulation models of colorectal cancer: the role of assumptions about adenoma progression. Med Decis Making. 2011;31(4):530–9.
Greuter MJ, Xu XM, Lew JB, Dekker E, Kuipers EJ, Canfell K, Meijer GA, Coupe VM. Modeling the adenoma and serrated pathway to colorectal cancer (ASCCA). Risk Anal. 2014;34(5):889–910.
Health Resources and Services Administration. 2012 health center data. https://bphc.hrsa.gov/datareporting/index.html. Accessed 7 Sept 2018.
Goldman SN, Liss DT, Brown T, Lee JY, Buchanan DR, Balsley K, Cesan A, Weil J, Garrity BH, Baker DW. Comparative effectiveness of multifaceted outreach to initiate colorectal cancer screening in community health centers: a randomized controlled trial. J Gen Intern Med. 2015;30(8):1178–84.
Centrum voor Kankeropsporing. Annual report screening program 2013; 2014.
Castle PE, Stoler MH, Wright TC Jr, Sharma A, Wright TL, Behrens CM. Performance of carcinogenic human papillomavirus (HPV) testing and HPV16 or HPV18 genotyping for cervical cancer screening of women aged 25 years and older: a subanalysis of the ATHENA study. Lancet Oncol. 2011;12(9):880–90.
Cox JT, Castle PE, Behrens CM, Sharma A, Wright TC Jr, Cuzick J. Comparison of cervical cancer screening strategies incorporating different combinations of cytology, HPV testing, and genotyping for HPV 16/18: results from the ATHENA HPV study. Am J Obstet Gynecol. 2013;208(3):184.e1–11.
Wright TC Jr, Stoler MH, Behrens CM, Apple R, Derion T, Wright TL. The ATHENA human papillomavirus study: design, methods, and baseline results. Am J Obstet Gynecol. 2012;206(1):46.e1–11.
Ronco G, Giorgi-Rossi P, Carozzi F, Confortini M, Dalla Palma P, Del Mistro A, Ghiringhello B, Girlando S, Gillio-Tos A, De Marco L, Naldoni C, Pierotti P, Rizzolo R, Schincaglia P, Zorzi M, Zappa M, Segnan N, Cuzick J. Efficacy of human papillomavirus testing for the detection of invasive cervical cancers and cervical intraepithelial neoplasia: a randomised controlled trial. Lancet Oncol. 2010;11(3):249–57.
SEER data. Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2012, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2012/ [based on November 2014 SEER data submission, posted to the SEER website: http://seer.cancer.gov/statfacts/html/cervix.html]. Published April 2015. Accessed 7 Sept 2018.
Wright TC, Stoler MH, Behrens CM, Sharma A, Zhang G, Wright TL. Primary cervical cancer screening with human papillomavirus: end of study results from the ATHENA study using HPV as the first-line screening test. Gynecol Oncol. 2015;136(2):189–97.
U.S. Census Bureau. Population estimates. U.S. Census Bureau, 2010. https://www.census.gov/. Accessed 7 Sept 2018.
Ward BW, Lucas JW. Summary health statistics for U.S. adults: national health interview survey, 2009. Vital Health Stat. 2010;10(249):1–207.
Acknowledgements
This project has been part of the DEXHELPP (Decision Support for Health Policy and Planning: Methods, Models and Technologies based on Existing Health Care Data) project in the frame of COMET-Competence Centers for Excellent Technologies supported by BMVIT, BMWFW and the state Vienna, by UMIT (University for Health Sciences, Medical Informatics and Technology), and by Erasmus Mundus Western Balkans (ERAWEB), a project funded by the European Commission. We thank Kelley J. P. Lindberg for proofreading and language editing.
Author information
Authors and Affiliations
Contributions
BJ, JT, MB, and US made substantial contributions to conception and design, acquisition of information, analysis and interpretation of results. BJ, JT, MB, GS, ACF, UR, GE, IW, NM, NP, JC, DG, JM, and US were involved in drafting the manuscript and revising it critically for important intellectual content. BJ, JT, MB, GS, ACF, UR, GE, IW, NM, NP, JC, DG, JM, and US agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The study was registered at the ethics committee of UMIT (University for Health Sciences, Medical Computer Science and Technology), Hall i.T. Austria (Registration 2162). Ethical standards were followed.
Availability of data and material
All data and material are available in published, mentioned, and referenced studies.
Conflict of interest
The authors (Jahn B, Todorovic J, Bundo M, Sroczynski G, Conrads-Frank A, Rochau U, Endel G, Wilbacher I, Malbaski N, Popper N, Chhatwal J, Greenberg D, Mauskopf J, Siebert U) declare that they have no competing interests.
Funding
This project was supported in part by DEXHELPP (Decision Support for Health Policy and Planning: Methods, Models and Technologies based on Existing Health Care Data, Grant no. 843550). DEXHELPP is in the frame of COMET-Competence Centers for Excellent Technologies. DEXHELPP is supported by BMVIT, BMWFW and the state Vienna. The COMET program is transacted by the FFG. In parts, this work has also been financially supported through Erasmus Mundus Western Balkans (ERAWEB), a project funded by the European Commission. The funding body did not have any influence on the design of the study and collection, analysis, and interpretation of data and in manuscript writing.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jahn, B., Todorovic, J., Bundo, M. et al. Budget Impact Analysis of Cancer Screening: A Methodological Review. Appl Health Econ Health Policy 17, 493–511 (2019). https://doi.org/10.1007/s40258-019-00475-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-019-00475-6