Abstract
Background
Few studies have addressed recent trends in hospitalization costs for inflammatory bowel disease (IBD).
Objective
We explored trends and described patient and hospital factors associated with hospitalization costs for IBD.
Methods
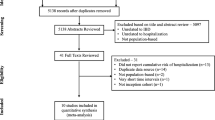
Using data from the 2003–2014 National Inpatient Sample for adults aged ≥ 18 years, we estimated costs using multivariable linear models and assessed linear trends by time periods using piecewise linear regressions.
Results
In 2014, there were an estimated 56,290 hospitalizations for Crohn’s disease (CD), with a mean cost of US$11,345 and median cost of US$7592; and 33,585 hospitalizations for ulcerative colitis (UC), with a mean cost of US$13,412 and median cost of US$8873. Higher costs were observed among Hispanic [adjusted cost ratio (ACR) = 1.07; 95% confidence interval (CI) = 1.00–1.14; p = 0.04] or other non-Hispanic (ACR = 1.09; 95% CI = 1.02–1.17; p = 0.01) CD patients than for non-Hispanic White CD patients. For UC patients, higher costs were observed among men (ACR = 1.09; 95% CI = 1.05–1.13; p < 0.001) compared with women and among patients aged 35–44 years, 45–54 years, and 55–64 years compared with those aged 18–24 years. Among all patients, factors associated with higher costs included higher household income, more comorbidities, and hospitals that were government nonfederal versus private, were large versus small, and were located in the West versus Northeast regions. From 2003 to 2008, total costs increased annually by 3% for CD (1.03; 95% CI = 1.02–1.05; p < 0.001) and 4% for UC (1.04; 95% CI = 1.02–1.06; p < 0.001), but remained unchanged from 2008 to 2014.
Conclusions
The findings are important to identify IBD patients with higher hospitalization costs and to inform policy plans on hospital resource allocation.


Similar content being viewed by others
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available because a Data User Agreement is individually required for HCUP NIS and MarketScan databases, but the software code underpinning the analysis is available from the corresponding author on reasonable request.
References
Dahlhamer JM, Zammitti EP, Ward BW, Wheaton AG, Croft JB. Prevalence of inflammatory bowel disease among adults aged ≥18 Years—United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:1166–9.
Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: results of the European Federation of Crohn’s and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis. 2007;1:10–20.
Vidal A, Gomez-Gil E, Sans M, et al. Health-related quality of life in inflammatory bowel disease patients: the role of psychopathology and personality. Inflamm Bowel Dis. 2008;14:977–83.
Bokemeyer B, Hardt J, Huppe D, et al. Clinical status, psychosocial impairments, medical treatment and health care costs for patients with inflammatory bowel disease (IBD) in Germany: an online IBD registry. J Crohns Colitis. 2013;7:355–68.
Annese V, Duricova D, Gower-Rousseau C, Jess T, Langholz E. Impact of new treatments on hospitalisation, surgery, infection, and mortality in IBD: a focus paper by the Epidemiology Committee of ECCO. J Crohns Colitis. 2016;10:216–25.
Malarcher CA, Wheaton AG, Liu Y, et al. Hospitalizations for Crohn’s disease—United States, 2003–2013. MMWR Morb Mortal Wkly Rep. 2017;66:377–81.
Crohn’s & Colitis Foundation. The facts about inflammatory bowel disease. 2014; http://www.crohnscolitisfoundation.org/assets/pdfs/updatedibdfactbook.pdf. Accessed 29 September 2017.
Moss AC. Optimizing the use of biological therapy in patients with inflammatory bowel disease. Gastroenterol Rep. 2015;3:63–8.
Frolkis AD, Dykeman J, Negron ME, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145:996–1006.
Bouguen G, Peyrin-Biroulet L. Surgery for adult Crohn’s disease: what is the actual risk? Gut. 2011;60:1178–81.
Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg. 2011;15:267–76.
Vester-Andersen MK, Prosberg MV, Jess T, et al. Disease course and surgery rates in inflammatory bowel disease: a population-based, 7-year follow-up study in the era of immunomodulating therapy. Am J Gastroenterol. 2014;109:705–14.
Kappelman MD, Rifas-Shiman SL, Porter CQ, et al. Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology. 2008;135:1907–13.
Prenzler A, Bokemeyer B, von der Schulenburg JM, Mittendorf T. Health care costs and their predictors of inflammatory bowel diseases in Germany. Eur J Health Econ. 2011;12:273–83.
Gibson TB, Ng E, Ozminkowski RJ, et al. The direct and indirect cost burden of Crohn’s disease and ulcerative colitis. J Occup Environ Med. 2008;50:1261–72.
Limsrivilai J, Stidham RW, Govani SM, Waljee AK, Huang W, Higgins PD. Factors that predict high health care utilization and costs for patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2017;15(385–392):e382.
Agency for Healthcare Research & Quality. Data innovations—ICD-10-CM/PCS resources. 2017; https://www.hcup-us.ahrq.gov/datainnovations/icd10_resources.jsp. Accessed 3 January 2018.
Agency for Healthcare Research & Quality. Nationwide inpatient sample redesign report. 2018; https://www.hcup-us.ahrq.gov/db/nation/nis/reports/NISRedesignFinalReport040914.pdf. Accessed 3 January 2018.
IBM Watson Health. Putting research data into your hands with the MarketScan databases. 2018; http://truvenhealth.com/markets/state-and-medicaid/products/data-and-tools/marketscan-database. Accessed 12 January 2018.
Agency for Healthcare Research & Quality. Overview of the national (Nationwide) inpatient sample (NIS). 2017; https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 2 October 2017.
Truven Health Analytics. Commercial claims and encounters Medicare supplemental. 2017; https://marketscan.truvenhealth.com/marketscanuniversity/userguide/2015%20MarketScanCCAE-MDCRUserGuide.pdf.
Agency for Healthcare Research & Quality. Cost-to-charge ratio files. 2017; https://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp#overview. Accessed 3 October 2017.
Peterson C, Xu L, Florence C, Grosse SD, Annest JL. Professional fee ratios for US hospital discharge data. Med Care. 2015;53:840–9.
Statistics Bureau of Labor. Databases, tables and calculators by subject. 2017; https://data.bls.gov/timeseries/CUUR0000SA0.
Agency for Healthcare Research & Quality. Elixhauser comorbidity software, version 3.7. 2017; https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed 12 January 2018.
Agency for Healthcare Research & Quality. Overview of disease severity measures disseminated with Nationwide Inpatient Sample (NIS) and Kids’ Inpatient Database (KID). https://www.hcup-us.ahrq.gov/db/nation/nis/OverviewofSeveritySystems.pdf. Accessed 3 October 2007.
Agency for Healthcare Research & Quality. NIS description of data elements: HOSP_BEDSIZE—bedsize of hospital. 2008; https://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp. Accessed 3 January 2018.
Nguyen GC, Murthy SK, Bressler B, et al. Quality of care and outcomes among hospitalized inflammatory bowel disease patients: a multicenter retrospective study. Inflamm Bowel Dis. 2017;23:695–701.
Bernstein CN, Papineau N, Zajaczkowski J, Rawsthorne P, Okrusko G, Blanchard JF. Direct hospital costs for patients with inflammatory bowel disease in a Canadian tertiary care university hospital. Am J Gastroenterol. 2000;95:677–83.
Hay JW, Hay AR. Inflammatory bowel disease: costs-of-illness. J Clin Gastroenterol. 1992;14:309–17.
Xu F, Dahlhamer JM, Zammitti EP, Wheaton AG, Croft JB. Health-risk behaviors and chronic conditions among adults with inflammatory bowel disease—United States, 2015 and 2016. MMWR Morb Mortal Wkly Rep. 2018;67:190–5.
Bahler C, Schoepfer AM, Vavricka SR, Brungger B, Reich O. Chronic comorbidities associated with inflammatory bowel disease: prevalence and impact on healthcare costs in Switzerland. Eur J Gastroenterol Hepatol. 2017;29:916–25.
Román ALS, Muñoz F. Comorbidity in inflammatory bowel disease. World J Gastroenterol. 2011;17:2723–33.
Zezos P, Kouklakis G, Saibil F. Inflammatory bowel disease and thromboembolism. World J Gastroenterol. 2014;20:13863–78.
Stadnicki A. Involvement of coagulation and hemostasis in inflammatory bowel diseases. Curr Vasc Pharmacol. 2012;10:659–69.
Oikonomou K, Kapsoritakis A, Eleftheriadis T, Stefanidis I, Potamianos S. Renal manifestations and complications of inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:1034–45.
Hait E, Bousvaros A, Grand R. Pediatric inflammatory bowel disease: what children can teach adults. Inflamm Bowel Dis. 2005;11:519–27.
Bernstein CN, Longobardi T, Finlayson G, Blanchard JF. Direct medical cost of managing IBD patients: a Canadian population-based study. Inflamm Bowel Dis. 2012;18:1498–508.
Sewell JL, Velayos FS. Systematic review: the role of race and socioeconomic factors on IBD healthcare delivery and effectiveness. Inflamm Bowel Dis. 2013;19:627–43.
Nguyen GC, Chong CA, Chong RY. National estimates of the burden of inflammatory bowel disease among racial and ethnic groups in the United States. J Crohns Colitis. 2014;8:288–95.
Weiss AJ, Elixhauser A. Overview of hospital stays in the United States, 2012: Statistical Brief #180. Healthcare Cost and Utilization Project (HCUP) statistical briefs. Rockville: Agency for Healthcare Research and Quality (US); 2006.
Park MD, Bhattacharya J, Park K. Differences in healthcare expenditures for inflammatory bowel disease by insurance status, income, and clinical care setting. PeerJ. 2014;2:e587.
Stranges E, Holmquist L, Andrews RM. Inpatient stays in rural hospitals, 2007: Statistical Brief #85. Healthcare Cost and Utilization Project (HCUP) statistical briefs. Rockville: Agency for Healthcare Research and Quality (US); 2006.
Bernstein CN, Loftus EV Jr, Ng SC, Lakatos PL, Moum B. Hospitalisations and surgery in Crohn’s disease. Gut. 2012;61:622–9.
Pillai N, Dusheiko M, Burnand B, Pittet V. A systematic review of cost-effectiveness studies comparing conentional, biological and surgical interventions for inflammatory bowel disease. PLoS One. 2017;12:e0185500.
Danese S, Vuitton L, Peyrin-Biroulet L. Biologic agents for IBD: practical insights. Nat Rev Gastroenterol Hepatol. 2015;12:537–45.
Author information
Authors and Affiliations
Contributions
Study design: FX, YL, JBC. Study analysis: FX, YL, KMR. Results interpretation: FX, YL, AGW, KMR, JBC. Manuscript writing: FX, YL, AGW, KMR, JBC. Manuscript approval: FX, YL, AGW, KMR, JBC.
Corresponding author
Ethics declarations
Funding
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of Interest
Fang Xu, Yong Liu, Anne G. Wheaton, Kristina M. Rabarison, and Janet B. Croft have no conflict of interest in the study.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Xu, F., Liu, Y., Wheaton, A.G. et al. Trends and Factors Associated with Hospitalization Costs for Inflammatory Bowel Disease in the United States. Appl Health Econ Health Policy 17, 77–91 (2019). https://doi.org/10.1007/s40258-018-0432-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-018-0432-4