Abstract
Background
Permanent childhood hearing loss is one of the most common birth conditions associated with speech and language delay. A hearing screening can result in early detection and intervention for hearing loss.
Objectives
To update and expand previous systematic reviews of economic evaluations of childhood hearing screening strategies, and explore the methodological differences.
Data Sources
MEDLINE, Embase, the Cochrane database, National Health Services Economic Evaluation Database (NHS EED), the Health Technology Assessment (HTA) database, and Canadian Agency for Drugs and Technologies in Health’s (CADTH) Grey matters.
Study Eligibility Criteria, Participants and Interventions
Economic evaluations reporting costs and outcomes for both the intervention and comparator arms related to childhood hearing screening strategies.
Results
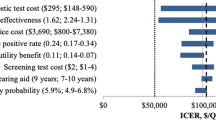
Thirty evaluations (from 29 articles) were included for review. Several methodological issues were identified, including: few evaluations reported outcomes in terms of quality-adjusted life years (QALYs); none estimated utilities directly from surveying children; none included disutilities and costs associated with adverse events; few included costs and outcomes that differed by severity; few included long-term estimates; none considered acquired hearing loss; some did not present incremental results; and few conducted comprehensive univariate or probabilistic sensitivity analysis. Evaluations published post-2011 were more likely to report QALYs and disability-adjusted life years (DALYs) as outcome measures, include long-term treatment and productivity costs, and present incremental results.
Limitations
We were unable to access the economic models and, although we employed an extensive search strategy, potentially not all relevant economic evaluations were identified.
Conclusions and Implications
Most economic evaluations concluded that childhood hearing screening is value for money. However, there were significant methodological limitations with the evaluations.

Similar content being viewed by others
Change history
01 March 2019
The third author’s first name should have been spelled “Teresa” rather than “Theresa”.
References
Centers for Disease Control and Prevention (CDC). United States Hearing Screening and Follow-up Survey 2009.
Levi H, Tell L, Cohen T. Sensorineural hearing loss in Jewish children born in Jerusalem. Int J Pediatr Otorhinolaryngol. 2004;68(10):1245–50.
Russ SA, Poulakis Z, Barker M, Wake M, Rickards F, Sounders K, et al. Epidemiology of congenital hearing loss in Victoria, Australia: epidemiología de la hipoacusia congénita en Victoria, Australia. Int J Audiol. 2003;42(7):385–90.
Morzaria S, Westerberg BD, Kozak FK. Systematic review of the etiology of bilateral sensorineural hearing loss in children. Int J Pediatr Otorhinolaryngol. 2004;68(9):1193–8.
Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120(4):898–921. https://doi.org/10.1542/peds.2007-2333.
Institute of Health Economics. The safety and efficacy/effectiveness of using automated testing devices for universal newborn hearing screening: an update. Edmonton: Institute of Health Economics (IHE); 2012.
Ching TY, Leigh G, Dillon H. Introduction to the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study: background, design, sample characteristics. Int J Audiol. 2013;52(sup2):S4–9.
Kennedy CR, McCann DC, Campbell MJ, Law CM, Mullee M, Petrou S, et al. Language ability after early detection of permanent childhood hearing impairment. N Engl J Med. 2006;354(20):2131–41. https://doi.org/10.1056/NEJMoa054915.
Wolff R, Hommerich J, Riemsma R, et al. Hearing screening in newborns: systematic review of accuracy, effectiveness, and effects of interventions after screening. Arch Dis Child. 2010;95:130–5.
Yoshinaga-Itano C, Coulter D, Thomson V. Developmental outcomes of children with hearing loss born in Colorado hospitals with and without universal newborn hearing screening programs. Semin Neonatol. 2001;6(6):521–9. https://doi.org/10.1053/siny.2001.0075.
Ching TYC. Is early intervention effective in improving spoken language outcomes of children with congenital hearing loss? Am J Audiol. 2015;24(3):345–8. https://doi.org/10.1044/2015_AJA-15-0007.
Ching TY, Dillon H, Button L, Seeto M, Van Buynder P, Marnane V, et al. Age at intervention for permanent hearing loss and 5-year language outcomes. Pediatrics. 2017;140(3):e20164274.
Aurélio FS, Tochetto TM. Newborn hearing screening: experiences of different countries. Arquivos Internacionais de Otorrinolaringologia. 2010;14(3):355–63.
Sloot F, Hoeve HL, De Kroon ML, Goedegebure A, Carlton J, Griffiths HJ, et al. Inventory of current EU paediatric vision and hearing screening programmes. J Med Screen. 2015;22(2):55–64.
Coates H, Gifkins K. Newborn hearing screening. Austral Prescrib. 2003;26(4):82–4.
Langer A, Holle R, John J. Specific guidelines for assessing and improving the methodological quality of economic evaluations of newborn screening. BMC Health Serv Res. 2012;12(1):300.
Colgan S, Gold L, Wirth K, Ching T, Poulakis Z, Rickards F, et al. The cost-effectiveness of universal newborn screening for bilateral permanent congenital hearing impairment: systematic review. Acad Pediatr. 2012;12(3):171–80.
Ching T, Day J, Seeto M, Dillon H, Marnane V, Street L. Predicting 3-year outcomes of early-identified children with hearing impairment. b-Ent. 2013:99.
Anderson R. Systematic reviews of economic evaluations: utility or futility? Health Econ. 2010;19(3):350–64.
Neumann PJ. Why don’t Americans use cost-effectiveness analysis. Am J Manag Care. 2004;10(5):308–12.
Prager DA, Stone DA, Rose DN. Hearing loss screening in the neonatal intensive care unit: auditory brain stem response versus Crib-O-Gram; a cost-effectiveness analysis. Ear Hear. 1987;8(4):213–6.
Brown J. Screening infants for hearing loss-an economic evaluation. J Epidemiol Community Health. 1992;46(4):350–6.
White KR, Maxon AB. Universal screening for infant hearing impairment: simple, beneficial, and presently justified. Int J Pediatr Otorhinolaryngol. 1995;32(3):201–10.
Friedland DR, Fahs MC, Catalano PJ. A cost-effectiveness analysis of the high risk register and auditory brainstem response. Int J Pediatr Otorhinolaryngol. 1996;38(2):115–30.
Kemper AR, Downs SM. A cost-effectiveness analysis of newborn hearing screening strategies. Arch Pediatr Adolesc Med. 2000;154(5):484–8.
Kezirian EJ, White KR, Yueh B, Sullivan SD. Cost and cost-effectiveness of universal screening for hearing loss in newborns. Otolaryngol Head Neck Surg. 2001;124(4):359–67.
Boshuizen H, Van der Lem G, Kauffman-de Boer M, Van Zanten G, Oudesluys-Murphy A, Verkerk P. Costs of different strategies for neonatal hearing screening: a modelling approach. Arch Dis Childh Fetal Neonatal Ed. 2001;85(3):F177–81.
Vohr BR, Oh W, Stewart EJ, Bentkover JD, Gabbard S, Lemons J, et al. Comparison of costs and referral rates of 3 universal newborn hearing screening protocols. J Pediatr. 2001;139(2):238–44.
Keren R, Helfand M, Homer C, McPhillips H, Lieu TA. Projected cost-effectiveness of statewide universal newborn hearing screening. Pediatrics. 2002;110(5):855–64.
Herrero C, Moreno-Ternero JD. Economic evaluation of newborn hearing screening procedures. Instituto Valenciano de Investigaciones Económicas; 2002.
Hessel F, Grill E, Schnell-Inderst P, Siebert U, Kunze S, Nickisch A, von Voß H, Wasem J. Economic evaluation of newborn hearing screening: modelling costs and outcomes. Ger Med Sci. 2003;1:Doc09.
Lin HC, Shu MT, Lee KS, Ho GM, Fu TY, Bruna S, et al. Comparison of hearing screening programs between one step with transient evoked otoacoustic emissions (TEOAE) and two steps with TEOAE and automated auditory brainstem response. Laryngoscope. 2005;115(11):1957–62.
Grill E, Uus K, Hessel F, Davies L, Taylor RS, Wasem J, et al. Neonatal hearing screening: modelling cost and effectiveness of hospital- and community-based screening. BMC Health Serv Res. 2006;6:14.
Uus K, Bamford J, Taylor R. An analysis of the costs of implementing the National Newborn Hearing Screening Programme in England. J Med Screen. 2006;13(1):14–9.
Schnell-Inderst P, Kunze S, Hessel F, Grill E, Siebert U, Nickisch A et al. Screening of the hearing of newborns—update. GMS Health Technol Assess. 2006;2:Doc20.
Institute of Health Economics. Screening newborns for hearing: the use of the automated auditory brainstem response and otoacoustic emissions tests for newborn hearing screening. Edmonton: Institute of Health Economics (IHE). 2007. p. 102.
Merlin T, Hedayati H, Sullivan T, Buckley E, Newton S, Hodgkinson B et al. Universal neonatal hearing screening. MSAC reference 17 Assessment report. Canberra: MSAC; 2007.
Lin H-C, Shu M-T, Lee K-S, Lin H-Y, Lin G. Reducing false positives in newborn hearing screening program: how and why. Otol Neurotol. 2007;28(6):788–92.
Porter HL, Neely ST, Gorga MP. Using benefit-cost ratio to select universal newborn hearing screening test criteria. Ear Hear. 2009;30(4):447–57.
Olusanya BO, Emokpae A, Renner JK, Wirz SL. Costs and performance of early hearing detection programmes in Lagos, Nigeria. Trans R Soc Trop Med Hyg. 2009;103(2):179–86.
Uilenburg N, Kauffman-de Boer M, van der Ploeg K, Oudesluys-Murphy AM, Verkerk P. An implementation study of neonatal hearing screening in the Netherlands. Int J Audiol. 2009;48(3):108–16.
Burke MJ, Shenton RC, Taylor MJ. The economics of screening infants at risk of hearing impairment: an international analysis. Int J Pediatr Otorhinolaryngol. 2012;76(2):212–8.
Huang LH, Zhang L, Tobe RY, Qi FH, Sun L, Teng Y, et al. Cost-effectiveness analysis of neonatal hearing screening program in China: should universal screening be prioritized? BMC Health Serv Res. 2012;12:97.
Tobe RG, Mori R, Huang L, Xu L, Han D, Shibuya K. Cost-effectiveness analysis of a national neonatal hearing screening program in China: conditions for the scale-up. PLOS ONE. 2013;8:e51990.
Fortnum H, Ukoumunne OC, Hyde C, Taylor RS, Ozolins M, Errington S, et al. A programme of studies including assessment of diagnostic accuracy of school hearing screening tests and a cost-effectiveness model of school entry hearing screening programmes. Health Technol Assess. 2016;20(36):1–210.
Chiou ST, Lung HL, Chen LS, Yen AM, Fann JC, Chiu SY, et al. Economic evaluation of long-term impacts of universal newborn hearing screening. Int J Audiol. 2017;56(1):46–52.
Chen X, Yuan M, Lu J, Zhang Q, Sun M, Chang F. Assessment of universal newborn hearing screening and intervention in Shanghai, China. Int J Technol Assess Health Care. 2017;33(2):206–14.
Heidari S, Manesh AO, Rajabi F, Moradi-Joo M. Cost-effectiveness analysis of automated auditory brainstem response and otoacoustic emission in universal neonatal hearing screening. Iran J Pediatr. 2017;27 (2)(e5229).
Rivera AS, Lam HY, Chiong CM, Reyes-Quintos MRT, Ricalde RR. The cost-effectiveness and budget impact of a community-based universal newborn hearing screening program in the Philippines. Acta Medica Philippina. 2017;51(1):28.
Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. Oxford: OUP; 2006.
Schroeder L, Petrou S, Kennedy C, McCann D, Law C, Watkin PM, et al. The economic costs of congenital bilateral permanent childhood hearing impairment. Pediatrics. 2006;117(4):1101–12.
Heidari S, Manesh AO, Rajabi F. The sensitivity and specificity of automated auditory brainstem response and otoacoustic emission in neonatal hearing screening: a systematic review. Audit Vestibul Res. 2015;24(3):141–51.
World Health Organization. Prevention of blindness and deafness. Grades of hearing impairment [on‐line]. Available at http://www.who.int/pbd/deafness/hearing_impairment_grades/en/.
Mathers C, Smith A, Concha M. Global burden of hearing loss in the year 2000. Glob Burden Dis. 2000;18(4):1–30.
Malek M. Implementing QALYs. Fordham: Hayward medical communications; 2000.
Semenov YR, Yeh ST, Seshamani M, Wang N-Y, Tobey EA, Eisenberg LS, et al. Age-dependent cost-utility of pediatric cochlear implantation. Ear Hear. 2013;34(4):402.
Thorrington D, Eames K. Measuring health utilities in children and adolescents: a systematic review of the literature. PLoS One. 2015;10(8):e0135672.
Wake M, Ching TYC, Wirth K, et al. Population outcomes of three approaches to detection of congenital hearing loss. Pediatrics. 2016;137:e20151722.
Barton GR, Bankart J, Davis AC, Summerfield QA. Comparing utility scores before and after hearing-aid provision. Appl Health Econ Health Policy. 2004;3(2):103–5.
Bisonni R, Lawler F, Pierce L. Recurrent otitis media: a cost-utility analysis of simulated treatment using tympanostomy tubes vs. antibiotic prophylaxis. Fam Pract Res J. 1991;11(4):371–8.
Summerfield AQ, Marshall DH, Barton GR, Bloor KE. A cost-utility scenario analysis of bilateral cochlear implantation. Arch Otolaryngol Head Neck Surg. 2002;128(11):1255–62.
Sassi F. Calculating QALYs, comparing QALY and DALY calculations. Health Policy Plan. 2006;21(5):402–8.
Adalsteinsson E, Toumi M. Benefits of probabilistic sensitivity analysis—a review of NICE decisions. J Mark Access Health Policy. 2013;1(1):21240.
Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 2010;96(1):5–21.
Pharmaceutical Benefits Advisory Committee (PBAC). Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (version 4.3). Canberra: Australian Government Department of Health and Ageing. 2008.
Morimoto T, Fukui T. Utilities measured by rating scale, time trade-off, and standard gamble: review and reference for health care professionals. J Epidemiol. 2002;12(2):160–78.
Ungar W. Economic evaluation in child health. Oxford: Oxford University Press; 2009.
Stevens KJ. Working with children to develop dimensions for a preference-based, generic, pediatric, health-related quality-of-life measure. Qual Health Res. 2010;20(3):340–51.
Stevens K. The Child Health Utility 9D (CHU9D)—a new paediatric preference based measure of health related quality of life. Pro Newslett. 2010;43:11–2.
Ratcliffe J. PRM125 whose values in health? A comparison of adult and adolescent values for the CHU9D and AQOL-6D. Value Health. 2012;15(7):A483.
Ratcliffe J, Huynh E, Chen G, Stevens K, Swait J, Brazier J, et al. Valuing the Child Health Utility 9D: using profile case best worst scaling methods to develop a new adolescent specific scoring algorithm. Soc Sci Med. 2016;157:48–59.
Kreimeier S, Oppe M, Ramos-Goñi JM, Cole A, Devlin N, Herdman M, et al. Valuation of EuroQol five-dimensional questionnaire, youth version (EQ-5D-Y) and EuroQol five-dimensional questionnaire, three-level version (EQ-5D-3L) health states: the impact of wording and perspective. Value Health. 2018;21(11):1291–8.
Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res. 2010;19(6):875–86.
UK Cochlear Implant Study Group. Criteria of candidacy for unilateral cochlear implantation in postlingually deafened adults II: cost-effectiveness analysis. Ear Hear. 2004;25(4):336–60.
Barton GR, Bloor KE, Marshall DH, Summerfield AQ. Health-service costs of pediatric cochlear implantation: multi-center analysis. Int J Pediatr Otorhinolaryngol. 2003;67(2):141–9.
Acknowledgements
RS, YG, and BP designed the systematic review. RS and BP applied the selection criteria to the identified studies. RS extracted and synthesised the data with input from BP. RS drafted the manuscript, with input from YG, TYCC, VM and BP. RS acts as guarantor for the paper and accepts full responsibility for the conduct of the review and decision to publish.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was a part of a Ph.D. project funded by International Macquarie University Research Excellence Scholarship (iMQRES). This work was also partially supported by the National Institute on Deafness and Other Communication Disorders (Grant no. R01DC008080) awarded to TYCC, and by the Commonwealth of Australia through the Office of Hearing Services and the HEARing CRC.
Conflict of interest
The authors (RS, YG, TYCC, VM, and BP) declare that they have no financial or non-financial conflict of interest in the subject matter or materials discussed in this manuscript.
Additional information
The original version of this article was revised: The third author's first name should have been spelled “Teresa” rather than “Theresa”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sharma, R., Gu, Y., Ching, T.Y.C. et al. Economic Evaluations of Childhood Hearing Loss Screening Programmes: A Systematic Review and Critique. Appl Health Econ Health Policy 17, 331–357 (2019). https://doi.org/10.1007/s40258-018-00456-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-018-00456-1