Summary
Background
Mental health stigma (MHS) places a burden on those affected that far exceeds psychosocial harms. Contact-based anti-stigma work has been found effective for several target groups. For medical students however, its efficacy remains unclear.
Aim
The purpose of this study was to examine the efficacy of contact-based, trialogic anti-stigma training for medical students.
Methods
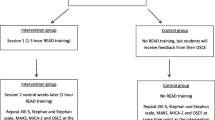
A randomized controlled trial (RCT) was conducted, controlling for standard clinical placement in psychiatry. External validity was maximized by including all students (n = 204) who started their 6‑week obligatory psychiatry course during the study period between March and July 2018. Assessments were conducted at the beginning of each of the two covered terms and immediately postintervention.
Results
Students who received the anti-stigma training displayed significantly less stigmatizing attitudes after the intervention, measured using the MICA (Mental Illness—Clinicians’ Attitudes) scale as primary outcome. Analogous findings were noted for social distance and stereotypes, whereas these could not be observed for emotional reactions. All significant changes were independent of gender and age.
Conclusion
The positive results underpin the research in this field and point towards the inclusion of comparable interventions in regular student curricula. Given the limitation of a missing late follow-up, however, further research regarding the persistence of stigma reduction is needed.
Zusammenfassung
Hintergrund
Stigmatisierung psychischer Erkrankungen stellt eine Belastung für Betroffene dar, deren Ausmaß die psychosozialen Folgen weit überschreitet. Kontaktbasierte Antistigma-Arbeit hat sich als effektiver Ansatz zum Abbau stigmatisierender Einstellungen für verschiedene Zielgruppen bewährt. Für die Wirksamkeit bei Medizinstudierenden fehlt jedoch ein empirischer Nachweis.
Ziel
Ziel der Studie war die Evaluation einer kontaktbasierten, trialogischen Antistigma-Kurzintervention für Medizinstudierende.
Methoden
Eine randomisierte, kontrollierte Studie (RCT) wurde durchgeführt mit regelhaftem praktischem Unterricht innerhalb der Psychiatrie als Kontrollbedingung. Zur Maximierung externer Validität erfolgte der Einschluss aller Studierenden (n = 204), welche im Studienzeitraum zwischen März und Juli 2018 ihr 6‑wöchiges Pflichtmodul in Psychiatrie belegten. Die Daten wurden zu Beginn beider eingeschlossener akademischer Phasen und direkt nach der Intervention erhoben.
Ergebnisse
Studierende zeigten nach Teilnahme an der Intervention ein signifikant geringeres Niveau stigmatisierender Einstellungen als vor der Intervention, gemessen anhand des MICA(Mental Illness – Clinicians’ Attitudes)-Fragebogens als „primary outcome“. Für soziale Distanz und die Zustimmung zu Stereotypen ergaben sich analoge Befunde, für emotionale Reaktionen dagegen ließ sich dieser Zusammenhang nicht nachweisen. Alle signifikanten Veränderungen traten unabhängig von Geschlecht und Alter auf.
Schlussfolgerung
Die positiven Ergebnisse untermauern die Forschungserkenntnisse in diesem Bereich und unterstreichen die Forderung nach Integration vergleichbarer Interventionen in das regelhafte Curriculum des Medizinstudiums. Angesichts der Limitation der Studie durch eine fehlende späte Follow-up-Phase ist jedoch weitere Forschung zur Persistenz der Stigmareduktion notwendig.

Similar content being viewed by others
References
Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. 2013;103(5):777–80. https://doi.org/10.2105/AJPH.2012.301056.
Thornicroft G. Shunned: discrimination against people with mental illness. Oxford, New York: Oxford University Press; 2006.
Mai Q, Holman CDAJ, Sanfilippo FM, Emery JD, Preen DB. Mental illness related disparities in diabetes prevalence, quality of care and outcomes: a population-based longitudinal study. BMC Med. 2011;9:118. https://doi.org/10.1186/1741-7015-9-118.
Chou FH, Tsai KY, Wu HC, Shen SP. Cancer in patients with schizophrenia: what is the next step? Psychiatry Clin Neurosci. 2016;70(11):473–88. https://doi.org/10.1111/pcn.12420.
Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. 2017;16(2):163–80. https://doi.org/10.1002/wps.20420.
Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–41. https://doi.org/10.1001/jamapsychiatry.2014.2502.
Wahlbeck K, Westman J, Nordentoft M, Gissler M, Laursen TM. Outcomes of nordic mental health systems: life expectancy of patients with mental disorders. Br J Psychiatry. 2011;199(6):453–8. https://doi.org/10.1192/bjp.bp.110.085100.
Avila C, Holloway AC, Hahn MK, Morrison KM, Restivo M, Anglin R, et al. An overview of links between obesity and mental health. Curr Obes Rep. 2015;4(3):303–10. https://doi.org/10.1007/s13679-015-0164-9.
Lipari RN, Van Horn S. Smoking and mental illness among adults in the United States. The CBHSQ report. 2013.
Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry. 2018;194(6):491–9. https://doi.org/10.1192/bjp.bp.107.045732.
Henderson C, Noblett J, Parke H, Clement S, Caffrey A, Gale-Grant O, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014;1(6):467–82. https://doi.org/10.1016/S2215-0366(14)00023-6.
Jones S, Howard L, Thornicroft G. ‘Diagnostic overshadowing’: worse physical health care for people with mental illness. Acta Psychiatr Scand. 2008;118(3):169–71. https://doi.org/10.1111/j.1600-0447.2008.01211.x.
Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387(10023):1123–32. https://doi.org/10.1016/S0140-6736(15)00298-6.
Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rusch N. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr Serv. 2012;63(10):963–73. https://doi.org/10.1176/appi.ps.201100529.
Corrigan PW. Best practices: strategic stigma change (SSC): five principles for social marketing campaigns to reduce stigma. Psychiatr Serv. 2011;62(8):824–6. https://doi.org/10.1176/ps.62.8.pss6208_0824.
Petkari E, Masedo Gutiérrez AI, Xavier M, Moreno Küstner B. The influence of clerkship on students’ stigma towards mental illness: a meta-analysis. Med Educ. 2018;52(7):694–704. https://doi.org/10.1111/medu.13548.
Yamaguchi S, Wu SI, Biswas M, Yate M, Aoki Y, Barley EA, et al. Effects of short-term interventions to reduce mental health-related stigma in university or college students: a systematic review. J Nerv Ment Dis. 2013;201(6):490–503. https://doi.org/10.1097/NMD.0b013e31829480df.
Kassam A, Glozier N, Leese M, Loughran J, Thornicroft G. A controlled trial of mental illness related stigma training for medical students. BMC Med Educ. 2011;11:51. https://doi.org/10.1186/1472-6920-11-51.
Amini H, Shoar S, Tabatabaee M, Arabzadeh S. The effect of clinical exposure to patients on medical students’ attitude towards mental illness. Iran J Psychiatry Behav Sci. 2016;10(3):e1887. https://doi.org/10.17795/ijpbs-1887.
Friedrich B, Evans-Lacko S, London J, Rhydderch D, Henderson C, Thornicroft G. Anti-stigma training for medical students: the education not discrimination project. Br J Psychiatry Suppl. 2013;55:s89–94. https://doi.org/10.1192/bjp.bp.112.114017.
Galletly C, Burton C. Improving medical student attitudes towards people with schizophrenia. Aust N Z J Psychiatry. 2011;45(6):473–6. https://doi.org/10.3109/00048674.2011.541419.
Papish A, Kassam A, Modgill G, Vaz G, Zanussi L, Patten S. Reducing the stigma of mental illness in undergraduate medical education: a randomized controlled trial. BMC Med Educ. 2013;13:141. https://doi.org/10.1186/1472-6920-13-141.
Bock T, Priebe S. Psychosis seminars: an unconventional approach. Psychiatr Serv. 2005;56(11):1441–3. https://doi.org/10.1176/appi.ps.56.11.1441.
Amering M, Schmolke M. Recovery in mental health: reshaping scientific and clinical responsibilities. London: Wiley; 2009.
Bock T, Schulz G, Sielaff G, Kuby A, Mahlke C. Overcoming stigma and discrimination “irre menschlich Hamburg”—example of a bottom-up project. In: Gaebel W, Roessler W, Sartorius N, editors. The stigma of mental illness—end of the story? Cham: Springer; 2017. pp. 469–83.
Bock T. Does humanity become more ill or illness more human? Psychiatr Prax. 2014;41(3):121–3. https://doi.org/10.1055/s-0034-1369919.
Kassam A, Glozier N, Leese M, Henderson C, Thornicroft G. Development and responsiveness of a scale to measure clinicians’ attitudes to people with mental illness (medical student version). Acta Psychiatr Scand. 2010;122(2):153–61. https://doi.org/10.1111/j.1600-0447.2010.01562.x.
Gabbidon J, Clement S, van Nieuwenhuizen A, Kassam A, Brohan E, Norman I, et al. Mental illness: clinicians’ attitudes (MICA) scale-psychometric properties of a version for healthcare students and professionals. Psychiatry Res. 2013;206(1):81–7. https://doi.org/10.1016/j.psychres.2012.09.028.
Indigo. MICA‑2 and MICA‑4 (mental illness: clinicians’ attitudes scale)—German version. 2020. http://www.indigo-group.org/stigma-scales/micav2-and-micav4-mental-illness-clinicians-attitudes-scale/. Accessed 30 Jan 2020.
Knudsen HC, Vázquez-Barquero JL, Welcher B, Gaite L, Becker T, Chisholm D, et al. Translation and cross-cultural adaptation of outcome measurements for schizophrenia: EPSILON study 2. Br J Psychiatry. 2018;177(S39):s8–s14. https://doi.org/10.1192/bjp.177.39.s8.
Dietrich S, Beck M, Bujantugs B, Kenzine D, Matschinger H, Angermeyer MC. The relationship between public causal beliefs and social distance toward mentally ill people. Aust N Z J Psychiatry. 2004;38(5):348–54. https://doi.org/10.1080/j.1440-1614.2004.01363.x.
Link BG, Cullen FT, Frank J, Wozniak JF. The social rejection of former mental patients: understanding why labels matter. Am J Sociol. 1987;92(6):1461–500.
Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–85. https://doi.org/10.1146/annurev.soc.27.1.363.
Angermeyer MC, Matschinger H. Labeling—stereotype—discrimination. Soc Psychiatry Psychiatr Epidemiol. 2005;40(5):391–5. https://doi.org/10.1007/s00127-005-0903-4.
Angermeyer MC, Matschinger H. The stigma of mental illness: effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatr Scand. 2003;108(4):304–9.
Speerforck S, Schomerus G, Matschinger H, Angermeyer MC. Treatment recommendations for schizophrenia, major depression and alcohol dependence and stigmatizing attitudes of the public: results from a German population survey. Eur Arch Psychiatry Clin Neurosci. 2017;267(4):341–50. https://doi.org/10.1007/s00406-016-0755-9.
Wong EC, Collins RL, Cerully JL, Yu JW, Seelam R. Effects of contact-based mental illness stigma reduction programs: age, gender, and asian, latino, and white American differences. Soc Psychiatry Psychiatr Epidemiol. 2018;53(3):299–308. https://doi.org/10.1007/s00127-017-1459-9.
Henderson C, Stuart H, Hansson L. Lessons from the results of three national antistigma programmes. Acta Psychiatr Scand. 2016;134(S446):3–5. https://doi.org/10.1111/acps.12605.
Brown H, Prescott R. Repeated measures data. Applied mixed models in medicine. New York: NY: John Wiley & Sons; 2015. pp. 231–88.
Pettigrew TF, Tropp LR, Wagner U, Christ O. Recent advances in intergroup contact theory. Int J Intercult Relat. 2011;35(3):271–80. https://doi.org/10.1016/j.ijintrel.2011.03.001.
Corrigan PW, Schmidt A, Bink AB, Nieweglowski K, Al-Khouja MA, Qin S, et al. Changing public stigma with continuum beliefs. J Ment Health. 2017;26(5):411–8. https://doi.org/10.1080/09638237.2016.1207224.
Angermeyer M, Schomerus G. A stigma perspective on recovery. World Psychiatry. 2012;11(3):163–4.
Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ. 2014;14:219. https://doi.org/10.1186/1472-6920-14-219.
Acknowledgements
The authors would like to thank the association “Irre Menschlich e. V.” and all its speakers. The involvement of service users is crucial to contact based anti-stigma work and made a successful implementation possible in the first place. This project is part of the dissertation process of D. Wechsler.
Author information
Authors and Affiliations
Contributions
D. Wechsler, C. Mahlke, G. Schomerus, and T. Bock conceived of the research question and/or designed the study. D. Wechsler oversaw the data acquisition. D. Wechsler and C. Mahlke analysed and interpreted the data. D. Wechsler drafted the report. All authors provided critical revisions to the report, important intellectual content and final approval.
Corresponding author
Ethics declarations
Conflict of interest
D. Wechsler, G. Schomerus, C. Mahlke, and T. Bock declare that they have no competing interests.
Ethical standards
An individual six-digit code was used for pseudonymization of participants and to match pre-and postquestionnaire scores. In agreement with the responsible department of research of the faculty of medicine, the study was conducted as part of the routinely administered evaluation of academic teaching and did not require additional ethical approval or written proof of consent exceeding the one given by students to the University of Hamburg for such purposes. Registration of this study was omitted as no patients were involved. The data that support this study’s findings are not uploaded due to legal restrictions.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
C. Mahlke and T. Bock equally share last authorship.
Rights and permissions
About this article
Cite this article
Wechsler, D., Schomerus, G., Mahlke, C. et al. Effects of contact-based, short-term anti-stigma training for medical students. Neuropsychiatr 34, 66–73 (2020). https://doi.org/10.1007/s40211-020-00337-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40211-020-00337-x