Abstract
The appearance and dissemination of antibiotic-resistant bacteria, particularly in specific closed environments such as intensive care units of acute care hospitals, have become a major health concern. The intestinal microbiota has various functions including host protection from overgrowth or colonization by unwanted bacteria. The exposure to antibiotics significantly reduces the bacterial density of intestinal microbiota leaving an ecologic void that can be occupied by potentially pathogenic and/or resistant bacteria frequently present in hospital settings. Consequently, the intestinal microbiota of inpatients acts as a major reservoir and plays a critical role in perpetuating the spread of resistant bacteria. There are novel innovative methods to protect the host microbiota during antibiotic treatment, but they do not offer a solution for already established colonization by resistant microorganisms. Fecal microbiota transfer (FMT) is a promising intervention to achieve this goal; however, controlled trials report lower success rates than initial retrospective studies, especially in case of gram negatives. The aim of the present article is to highlight the importance of the intestinal microbiota in the global spread of multi-drug-resistant (MDR) microorganisms and to review the recent advances to protect the human microbiota from the action of antibiotics as well as a critical discussion about the evidence of decolonization of MDR microorganisms by FMT.
Similar content being viewed by others
The human gut acts as a major reservoir of MDR bacteria, where they overgrow and share genetic determinants of resistance with other species, perpetuating their spread. |
The most common strategy for gut decolonization is the use of oral, non-absorbable antibiotics, although fecal microbiota transference (FMT) is a promising intervention. |
We summarize 145 FMTs performed for intestinal decolonization of MDR bacteria in the last 5 years from 25 publications. |
According to our analysis, FMT was significantly more successful against GPC than GNB, with no antibiotic consumption after FMT in the case of concomitant CDI and in older versus recent reports. |
Introduction
Antibiotic treatment has significantly improved the outcome of infected patients and has significantly reduced the number of surgical infections. Bacteria are considered multi-drug resistant (MDR) when they become resistant to at least 1 agent in ≥ 3 antibiotic classes to which they are normally expected to be susceptible. During the last 15 years, the spread of genetic determinants of resistance has led to the emergence of extensively drug-resistant (resistant to at least 1 agent in all but ≤ 2 antibiotic classes) and pandrug-resistant bacteria (resistant to all agents in all antibiotic classes) [1]. Although some resistant bacteria are present in the community, the majority are found in hospitals where these bacteria find susceptible hosts but also the perfect environment to spread through the activity of health care workers. The most relevant MDR gram negatives include third-generation cephalosporin-resistant (3GCR) and carbapenem-resistant (CR) Enterobacterales, CR Acinetobacter baumanii and CR Pseudomonas aeruginosa [2]. These pathogens are associated with severe infections including ventilator-associated pneumonia, catheter-related bacteremia and surgical site infections that have a significantly higher morbidity and mortality than those caused by the same susceptible species [3,4,5]. Hand hygiene, isolation precautions [6], antibiotic stewardship programs [7] and decolonization with non-absorbable antibiotics [8] have proved to be only partially effective to diminish the spread of MDR microorganisms.
In this context, it is evident that alternative methods to combat the spread of MDR bacteria are warranted. The human gut contains > 100 million bacteria that play an important role in metabolic processes, immune modulation and protection against the colonization or overgrowth of pathogenic microorganisms (colonization resistance). A dysbiotic microbiota is an imbalance in the intestinal microbial community (including bacteria, yeast, viruses and parasites) characterized by quantitative and qualitative changes in the composition of the microbiota itself, which entails a loss of its functions [9]. Clostridioides difficile infection (CDI), the most common cause of diarrhea in hospitalized patients, is the consequence of antibiotic-induced dysbiosis [10]. The lack of microbiota recovery after an episode of diarrhea is associated with recurrent episodes and has been successfully treated with fecal microbiota transfer (FMT) from healthy volunteers. Whether this therapeutic approach can be applied to other entities related to dysbiosis is under debate [11].
The objective of this narrative review is to discuss the importance of intestinal microbiota as a reservoir of MDR pathogens and review original strategies that aim to preserve and/or modulate the composition of intestinal microbiota, with special focus on FMT. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Intestinal Microbiota as a Reservoir for MDR Gram Negatives and Factors Associated with Persistent Carriage
The worldwide spread of 3GCR Enterobacterales has led to a significant increase of carbapenem prescription in the last decade, which, in turn, has greatly contributed to the recent emergence of CR gram-negative bacteria. Currently, in Europe, one out of every three Klebsiella pneumoniae isolates is resistant to third-generation cephalosporins, and one-third of these strains have additional resistance to fluoroquinolones and aminoglycosides as well. The mean prevalence of CR K. pneumoniae is 7.2%, but this percentage is as high as 29% in Italy and 64% in Greece [12]. The prevalence of 3GCR and CR Enterobacterales in inpatients from the USA is 12.6% and 1.2%, respectively [13]. In addition, the problem of MDR in other gram negatives such as A. baumanii and P. aeruginosa is a major concern in intensive care units worldwide with percentages of carbapenem resistance > 20% [14].
The presence of MDR bacteria was initially associated with acute care hospitals; however, with the increased survival of susceptible patient populations in the Western world, the problem has been extended to rehabilitation centers and nursing homes in recent years, converting these into major sources of patients colonized with MDR bacteria [15]. Interestingly, the MDR Enterobacterales in Europe and America remain confined to the health care-related population, while the gut colonization in the community is < 5%. However, in Africa and Asia this percentage increases up to 15% and 46%, respectively [16], suggesting that MDR bacteria are able to colonize even healthy people if the exposure, usually from contaminated foods [17, 18], is high enough. As a consequence, traveling to certain developing countries is a risk factor for MDR bacteria acquisition [19]. Two prospective trials [20, 21] followed > 2500 returned European travelers for a year, and the pooled median duration of post-travel colonization was 30 days [22]. In contrast, in another European study, the percentage of persistent carbapenemase-producing K. peumoniae carriers at 6, 12 and 24 months after discharge from an acute-care hospital was 55%, 30% and 20%, respectively. The main risk factors for being a persistent carrier were the presence of any catheter, living in a long-term care facility, a low functional status measured by Barthel’s index and important comorbidity according to Charlson’s score [23]. The conclusion from these results is that under high exposure to MDR gram negatives (Asia, Africa), healthy people may be transiently colonized, but once the exposure disappears, the microbiota is able to avoid the definitive engraftment of these microorganisms. In contrast, “fragile” patients (older, with comorbidities) [24] have been associated with a dysbiotic microbiota [25] that is aggravated by antibiotic consumption, which favors prolong colonization.
On the other hand, the number of new antibiotics has dropped considerably in recent years, and there are hardly any novel antibiotic classes on the horizon (Fig. 1). Consequently, the above situation gave rise to the renaissance of the utilization of the highly toxic colistin, which promptly brought about the appearance of a new type of colistin resistance that may pose a severe public health threat in the next years [26].

(Adapted from https://www.cdc.gov/drugresistance/about.html)
Year of commercialization of the principal antibiotics and time of first detection of resistant strains. XDR extensively drug resistant, PDR pandrug resistant. *Described in Staphylococcus.
The intestine harbors one of the most important microbial communities of the human body regarding microbial density and diversity [27]. The intestinal microbiota is implicated in different physiologic processes that are essential to the host health. One of these processes is colonization resistance, which consists of the gut microbiota's ability to avoid intestinal pathogen or MDR bacteria colonization by directly competing for the ecologic niche with these microorganisms or indirectly stimulating the human immune defenses [28]. One example of the colonization resistance mechanism is the butyrate-producing obligate anaerobe members of the Firmicutes and Bacteroidetes phyla, a major and critical component of the intestinal microbiota. Microbially produced butyrate promotes local immune system homeostasis, gut epithelial barrier function, proliferation of health-associated anaerobes and suppression of facultative anaerobes such as Enterobacterales [29]. Administration of antimicrobial agents is one of the main causes of intestinal microbiota disturbances that can lead to dysbiosis (see definition above). The intensity of the microbiota damage induced by antibiotic consumption and consequently the risk of dysbiosis depends on: (1) the active antibiotic concentration in feces, which is related to the dose, route of administration, oral bioavailability, bile elimination and potential in vivo inactivation, (2) antibiotic spectrum and (3) exposure duration [30]. However, the intestinal microbiota has the ability to restore its equilibrium after an external perturbation (i.e., antibiotic treatment) known as the resilience phenomenon [31], which varies from one individual to another, suggesting that the risk of developing dysbiosis also depends on the diversity and specific composition of the intestinal microbiota of each individual [32].
During a state of dysbiosis, the niches that are left open after disturbances can be occupied by the overgrowth of microorganisms that at low densities are symbionts but have pathogenic potential at high densities (pathobionts). Members of the phylum Proteobacteria (Escherichia coli or K. pneumoniae) normally represent < 2% of the microbiota, but in dysbiotic state these bacteria can represent > 30% of the total species. On the other hand, through health care workers’ hands as a vector of transmission, this ecologic void can be occupied by environmental opportunistic pathogens (K. pneumoniae, P. aeruginosa, A. baumanii, S. maltophilia) that frequently carry genetic determinants of resistance in a hospital setting. Additionally, considering that the intestine also provides an optimal environment for horizontal gene transfer between microbes, exchange of resistance determinants is also favored [33]. From this perspective, the dysbiotic microbiota is a key factor (reservoir) to perpetuate the spread of MDR gram negatives. In recent years, oral beta-lactamases and products that absorb antibiotics in the proximal colon have been developed to minimize the deleterious effect of antibiotics on intestinal microbiota [34,35,36].
Benefit of Eradication or Reduction in the Predominance of MDR Gram Negatives in the Intestinal Microbiota
On the one hand, intestinal colonization by MDR bacteria in hospitalized patients increases the risk of dissemination of the bacteria in the ward. On the other hand, it increases the risk of an infection by the same bacteria. As mentioned before, Proteobacteria normally represent < 2% of the microbiota, but a longitudinal study in patients undergoing allogenic hematopoietic stem cell transplantation demonstrated marked shifts in bacterial populations inhabiting the gut. Intestinal domination, defined as occupation of at least 30% of the microbiota by a single predominating bacterial taxon, occurred frequently. Commonly encountered dominating organisms included Enterococcus, Streptococcus and various Proteobacteria. Enterococcal and proteobacterial domination increased the risk of Enterococcus spp. and gram-negative rod bacteremia nine- and fivefold, respectively [37].
The most common strategy for gut decolonization is the use of oral, non-absorbable antibiotics, which may reach sufficiently high concentrations in the digestive tube to inhibit bacterial growth [38, 39]. A recent retrospective study on patients colonized by carbapenemase-producing K. pneumoniae showed that oral aminoglycoside reduced the risk of being infected by the same colonizing K. pneumoniae by > 80% and also reduced the mortality rate [40]. Interestingly, these differences were achieved although the microbiologic eradication (two consecutive negative rectal swabs) was only obtained in 59% of the treated cases. This great impact suggests that it is not necessary to eradicate the microorganism but to reduce its density to exert a benefit on the patients’ outcome. We do not know what the impact of density reduction on the bacterial dissemination is, but it seems reasonable to also expect a positive effect. The major concern of this study is that there were significantly more gentamicin-resistant microorganisms detected in treated patients than in the control group (13.6% vs. 3%, p = 0.008) [40]. Similarly, the appearance of resistance in gram-negative bacteria was also observed after topical administration of colistin [41]. Additionally, non-absorbable antibiotics inevitably perpetuate intestinal dysbiosis. Therefore, it is of paramount importance to find alternative solutions to eradicate or reduce the density of MDR bacteria in the gut of colonized patients and restore a healthy microbiota composition in these patients.
Fecal Microbiota Transfer
FMT from a healthy donor is a well-recognized treatment of multiple recurrences of CDI where the fundamental underlying problem is a severe dysbiosis [10]. Classically, this procedure has been named fecal microbiota transplantation. However, the intestinal microbiota is not an organ like the liver or kidney. We consider that transfer is a more adequate designation. The aim of this section is to review the published experience on using FMT for intestinal decolonization of MDR microorganisms.
We conducted a literature search in PubMed using the following keywords: fecal microbiota transplantation, gut microbiota, multi-drug-resistant microorganisms and gut, but we found more articles by reviewing the literature. Revision articles, duplications of the same data and articles where the end point was not clearly decolonization rate were excluded [42,43,44]. We identified 25 publications that summarize 145 FMTs performed in MDR bacteria-carrying patients in the last 5 years (Table 1). Fourteen of these publications were case reports (n = 17), three articles described retrospective cohorts (n = 29), and eight publications reported prospective data, mostly uncontrolled trials (n = 99). Of the reported 145 cases, 39 (26.9%) corresponded to patients colonized by a MDR microorganism and a concomitant CDI. Forty-eight FMTs (33.1%) were performed in patients carrying MDR gram-positive cocci (GPC), 92 (63.4%) in carriers of gram-negative bacilli (GNB) and 5 in patients colonized by both GPC and GNB (3.4%). Of the 97 GNB colonizations, 59 (60.8%) were due to carbapenem-resistant strains.
Demographic data and technical details of FMT were not available in all publications; for this reason we provide the numerator and denominator of each characteristic. Based on available data, 42/94 (44.7%) of FMT recipients were female, with a median age of 59 (IQR 43.5–70) years. Donors were unrelated in 113/132 studies (85.6%), and the gender was available in only 49, with 26.5% (13/49) being female. FMT was performed using a fresh donation in 49.1% (53/108) and frozen microbiota in 50.9% (55/108) of the cases. The median amount of feces used for FMT was 50 g (IQR 50–150 g). More patients received the FMT through a nasogastric tube (80/145, 61.9%) than by the oral route (24/145, 17.9%) or enema (22/145, 16.4%). Additionally, in three patients FMT was administered via colonoscopy (2.2%), in each case (0.7%) via gastroscopy or a combination of enema and nasogastric tube. On 101 occasions (69.7%), a single FMT was performed, while 2, 3 and 4 FMTs were performed in 37 (25.5%), 5 (3.4%) and 2 cases (1.4%), respectively.
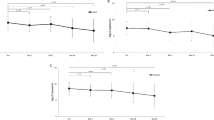
The criterion for success differed between studies, but was based on a certain number of negative follow-up rectal swabs in most cases. Median follow-up time was 90 days (IQR 30–150 days, range 14–1220 days). Overall success rate was 70.1% (101/144). Table 2 summarizes the comparison of successful and failed FMTs according to relevant characteristics. The main findings were that FMT was significantly more successful: (1) against GPC than GNB, (2) in the case of concomitant CDI, (3) in older reports (2014–2016 vs. 2017–2019) and (4) when no antibiotic was given after FMT.
The temporal difference could be attributed to the fact that GPC colonization and concomitant CDI were more frequent in older studies (mostly case reports and retrospective cohorts) while most recent publications were prospective trials. However, the type of microorganism and concomitant CDI remained statistically significant for outcome even when limiting the analysis to prospective trials. The success rate in GNB colonization was 56.9% vs. 87.9% in GPC (p = 0.003) and 89.5% in the case of concomitant CDI vs. 62.0% in its absence (p = 0.028). In both situations, decolonization also tended to be achieved earlier (Fig. 2). The explanation for better results in GPC (mainly Enterococcus spp.) is not evident, but a recent animal model demonstrated that predominance of ampicillin-resistant enterococci induced by ampicillin can be cleared by using a simple combination of four species (Clostridium bolteae, Blautia producta, Bacteroides sartorii and Parabacteroides distasonis) [45]. We hypothesize that greater diversity in the donor microbiota increases its competitive ability and clearing of GNB. Indeed, one of the largest studies focusing on GNB showed that donor microbiota richness and biodiversity were significantly associated with gut decolonization [46]. As mentioned, also concomitant CDI was associated with a higher decolonization rate after FMT, suggesting that the deeper the dysbiosis, the easier the donor microbiota engraftment and displacement of MDR bacteria. In line with this, it has been suggested that intestinal preparation before FMT reduces the bacterial content in the gut lumen and enhances engraftment of the microbiota transferred [47, 48].
Taken together, the data support that the decolonization of MDR-GNB using FMT needs to be tuned more finely to obtain better results. Based on evidence from CDI, colonoscopic administration of fresh microbiota obtained from 50 g of feces of a healthy donor is associated with the highest efficacy. To improve decolonization of GNB by FMT, we suggest the following: (1) to select donors with rich and diverse microbiota, (2) to reduce the host microbiota by bowel preparation as we do before a colonoscopy and to give non-absorbable antibiotics before FMT and (3) to increase the microbiota dose, particularly among patients without CDI and those who receive antibiotics after FMT. In these patients it may be necessary to increase the total amount of microbiota by multiple FMTs in short periods of time or by repeating FMT every time the patient receives an antibiotic. Alternatively, the impact of FMT may be increased by multiple capsules containing a high microbiota concentrate (e.g., by lyophilization) several times. In the future, it will be necessary to promote prospective studies to evaluate each of these proposals.
Conclusion
The rise of MDR bacteria is a growing global threat. The intestinal microbiota of patients acts as a major reservoir where these bacteria overgrow, dominate and share genetic determinants of resistance with other strains and species, thus perpetuating the spread of MDR bacteria. There are novel innovative methods to protect host microbiota during antibiotic treatment, but they do not offer a solution for established MDR colonization. FMT is a promising intervention to achieve this goal, although recent controlled trials report lower success rates than initial retrospective studies, especially in the case of GNB. It seems that microbiota engraftment and clearance of MDR GNB are favored by a profound host dysbiosis as in the case of CDI, whereas in other situations the results of FMT are only modest. Apparently, improved protocols need to be adapted for different clinical situations. Well-designed prospective trials addressing individual details of the procedure are needed to elucidate this complex issue.
References
Magiorakos A, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Bacteria: an international expert proposal for interim standard definitions for acquired resistance. Microbiology. 2012;18(3):268–81.
Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–27.
Xu L, Sun X, Ma X. Systematic review and meta-analysis of mortality of patients infected with carbapenem-resistant Klebsiella pneumoniae. Ann Clin Microbiol Antimicrob. 2017;16(1):1–12.
Lemos EV, de la Hoz FP, Einarson TR, Mcghan WF, Quevedo E, Castañeda C, et al. Carbapenem resistance and mortality in patients with Acinetobacter baumannii infection: systematic review and meta-analysis. Clin Microbiol Infect. 2014;20(5):416–23.
Liu Q, Li X, Li W, Du X, He JQ, Tao C, et al. Influence of carbapenem resistance on mortality of patients with Pseudomonas aeruginosa infection: a meta-analysis. Sci Rep. 2015;5(June):1–10.
Magiorakos AP, Burns K, Rodríguez Baño J, Borg M, Daikos G, Dumpis U, et al. Infection prevention and control measures and tools for the prevention of entry of carbapenem-resistant Enterobacteriaceae into healthcare settings: guidance from the European centre for disease prevention and control. Antimicrob Resist Infect Control. 2017;6(1):1–17.
Hulscher MEJL, Prins JM. Antibiotic stewardship: does it work in hospital practice? A review of the evidence base. Clin Microbiol Infect. 2017;23(11):799–805.
Tacconelli E, Mazzaferri F, de Smet AM, Bragantini D, Eggimann P, Huttner BD, et al. ESCMID-EUCIC clinical guidelines on decolonization of multidrug-resistant gram-negative bacteria carriers. Clin Microbiol Infect. 2019;25(7):807–17.
Stecher B, Maier L, Hardt WD. “Blooming” in the gut: how dysbiosis might contribute to pathogen evolution. Nat Rev Microbiol. 2013;11(4):277–84.
Debast SB, Bauer MP, Kuijper EJ. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect. 2014;20(Suppl 2):1–26.
Allegretti JR, Mullish BH, Kelly C, Fischer M. The evolution of the use of faecal microbiota transplantation and emerging therapeutic indications. Lancet. 2019;394(10196):420–31.
European Centre for Disease Prevention and Control. Surveillance of antimicrobial resistance in Europe: annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2017. 2018. pp. 1–97.
Gupta V, Ye G, Olesky M, Lawrence K, Murray J, Yu K. National prevalence estimates for resistant Enterobacteriaceae and Acinetobacter species in hospitalized patients in the United States. Int J Infect Dis. 2019;85:203–11.
Pérez A, Gato E, Pérez-Llarena J, Fernández-Cuenca F, Gude MJ, Oviaño M, et al. High incidence of MDR and XDR Pseudomonas aeruginosa isolates obtained from patients with ventilator-associated pneumonia in Greece, Italy and Spain as part of the MagicBullet clinical trial. J Antimicrob Chemother. 2019;74(5):1244–52.
van Duin D, Paterson D. Multidrug resistant bacteria in the community: trends and lessons learned. Infect Dis Clin N Am. 2016;30(2):377–90.
Karanika S, Karantanos T, Arvanitis M, Grigoras C, Mylonakis E. Fecal colonization with extended-spectrum beta-lactamase-producing Enterobacteriaceae and risk factors among healthy individuals: a systematic review and metaanalysis. Clin Infect Dis. 2016;63(3):310–8.
Hu Y, Yang X, Lu N, Zhu B. The abundance of antibiotic resistance genes in human guts has correlation to the consumption of antibiotics in animal. Gut Microbes. 2014;5(2):245–9.
Manyi-Loh C, Mamphweli S, Meyer E, Okoh A. Antibiotic use in agriculture and its consequential resistance in environmental sources: potential public health implications. Molecules. 2018;23(4):795.
Exner M. Antibiotic resistance: what is so special about multidrug-resistant gram-negative bacteria? GMS Hyg Infect Control. 2017;12:1–24.
Ruppé E, Armand-Lefèvre L, Estellat C, Consigny PH, El Mniai A, Boussadia Y, et al. High rate of acquisition but short duration of carriage of multidrug-resistant Enterobacteriaceae after travel to the tropics. Clin Infect Dis. 2015;61(4):593–600.
Arcilla MS, van Hattem JM, Haverkate MR, Bootsma MCJ, van Genderen PJJ, Goorhuis A, et al. Import and spread of extended-spectrum β-lactamase-producing Enterobacteriaceae by international travellers (COMBAT study): a prospective, multicentre cohort study. Lancet Infect Dis. 2017;17(1):78–85.
Ruppé E, Andremont A, Armand-Lefèvre L. Digestive tract colonization by multidrug-resistant Enterobacteriaceae in travellers: an update. Travel Med Infect Dis. 2017;2018(21):28–35.
Feldman N, Adler A, Molshatzki N, Navon-Venezia S, Khabra E, Cohen D, et al. Gastrointestinal colonization by KPC-producing Klebsiella pneumoniae following hospital discharge: duration of carriage and risk factors for persistent carriage. Clin Microbiol Infect. 2013;19(4):E190–6.
Kwetkat A, Pfister W, Pansow D, Pletz MW, Sieber CC, Hoyer H. Naso- and oropharyngeal bacterial carriage in nursing home residents: impact of multimorbidity and functional impairment. PLoS One. 2018;13(1):1–13.
Claesson MJ, Jeffery IB, Conde S, Power SE, O’connor EM, Cusack S, et al. Gut microbiota composition correlates with diet and health in the elderly. Nature. 2012;488(7410):178–84.
Caniaux I, van Belkum A, Zambardi G, Poirel L, Gros MF. MCR: modern colistin resistance. Eur J Clin Microbiol Infect Dis. 2017;36(3):415–20.
Costello EK, Lauber CL, Hamady M, Fierer N, Jeffrey I, Knight R. Bacterial community variation in human body habitats across space and time. Science. 2013;326(5960):1694–7.
Casals-Pascual C, Vergara A, Vila J. Intestinal microbiota and antibiotic resistance: perspectives and solutions. Hum Microbiome J. 2018;2018(9):11–5.
Byndloss MX, Olsan EE, Rivera-chávez F, Tiffany CR, Cevallos SA, Lokken KL, et al. Microbiota-activated PPAR-γ-signaling inhibits dysbiotic Enterobacteriaceae expansion. Science. 2017;357(6351):570–5.
Sullivan Å, Edlund C, Nord CE. Effect of antimicrobial agents on the ecological balance of human microflora. Lancet Infect Dis. 2002;1(2):101–14.
Sommer F, Anderson JM, Bharti R, Raes J, Rosenstiel P. The resilience of the intestinal microbiota influences health and disease. Nat Rev Microbiol. 2017;15(10):630–8.
Dethlefsen L, Relman DA. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci. 2011;108(Supplement_1):4554–61.
Bag S, Ghosh T, Banerjee S, Mehta O, Verma J, Dayal M, et al. molecular insights into antimicrobial resistance traits of commensal human gut microbiota. Microb Ecol. 2018;77(2):546–57.
Kokai-kun JF, Roberts T, Coughlin O, Sicard E, Rufiange M, Fedorak R, et al. The oral B-lactamase SYN-004 (ribaxamase) degrades ceftriaxone excreted into the intestine in phase 2a clinical studies. Antimicrob Agents Chemother. 2017;61(3):e02197.
Connelly S, Furlan-Freguia C, Fanelli B, Hasan NA, Colwell RR, Kaleko M. Oral β-lactamase therapies prevent microbiome damage and attenuate antibiotic resistance from IV and oral antibiotics in large animal models of antibiotic-mediated gut dysbiosis. Open Forum Infect Dis. 2018;5(Suppl 1):S226.
Burdet C, Sayah-Jeanne S, Nguyen TT, Miossec C, Saint-Lu N, Pulse M, et al. Protection of hamsters from mortality by reducing fecal moxifloxacin concentration with DAV131A in a model of moxifloxacin-induced Clostridium difficile colitis. Antimicrob Agents Chemother. 2017;61(10):1–9.
Taur Y, Xavier JB, Lipuma L, Ubeda C, Goldberg J, Gobourne A, et al. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin Infect Dis. 2012;55(7):905–14.
Oren I, Sprecher H, Finkelstein R, Hadad S, Neuberger A, Hussein K, et al. Eradication of carbapenem-resistant Enterobacteriaceae gastrointestinal colonization with nonabsorbable oral antibiotic treatment: a prospective controlled trial. Am J Infect Control. 2013;41(12):1167–72.
Bar-Yoseph H, Hussein K, Braun E, Paul M. Natural history and decolonization strategies for ESBL/carbapenem-resistant Enterobacteriaceae carriage: systematic review and meta-analysis. J Antimicrob Chemother. 2016;71:2729–39.
Machuca I, Gutiérrez-Gutiérrez B, Pérez Cortés S, Gracia-Ahufinger I, Serrano J, Madrigal MD, et al. Oral decontamination with aminoglycosides is associated with lower risk of mortality and infections in high-risk patients colonized with colistin-resistant KPC-producing Klebsiella pneumoniae. J Antimicrob Chemother. 2016;71(11):3242–9.
Oostdijk EAN, Smits L, De Smet AMGA, Leverstein-Van Hall MA, Kesecioglu J, Bonten MJM. Colistin resistance in gram-negative bacteria during prophylactic topical colistin use in intensive care units. Intensive Care Med. 2013;39(4):653–60.
Millan B, Park H, Hotte N, Mathieu O, Burguiere P, Tompkins TA, et al. Fecal microbial transplants reduce antibiotic-resistant genes in patients with recurrent Clostridium difficile infection. Clin Infect Dis. 2016;62(12):1479–86.
Jouhten H, Mattila E, Arkkila P, Satokari R. Reduction of antibiotic resistance genes in intestinal microbiota of patients with recurrent Clostridium difficile infection after fecal microbiota transplantation. Clin Infect Dis. 2016;63(5):710–1.
Leung V, Vincent C, Edens TJ, Miller M, Manges AR. Antimicrobial resistance gene acquisition and depletion following fecal microbiota transplantation for recurrent Clostridium difficile infection. Clin Infect Dis. 2018;66(3):456–9.
Caballero S, Kim S, Carter RA, Leiner IM, Sušac B, Miller L, et al. Cooperating commensals restore colonization resistance to vancomycin-resistant Enterococcus faecium. Cell Host Microbe. 2017;21(5):592–602.
Bilinski J, Grzesiowski P, Sorensen N, Madry K, Muszynski J, Robak K, et al. Fecal microbiota transplantation in patients with blood disorders inhibits gut colonization with antibiotic-resistant bacteria: results of a prospective single-center study. Clin Infect Dis. 2017;65(3):364–70.
Huttner BD, de Lastours V, Wassenberg M, Maharshak N, Mauris A, Galperine T, et al. A 5-day course of oral antibiotics followed by faecal transplantation to eradicate carriage of multidrug-resistant Enterobacteriaceae: a randomized clinical trial. Clin Microbiol Infect. 2019;25:830–8.
Saïdani N, Lagier JC, Cassir N, Million M, Baron S, Dubourg G, et al. Faecal microbiota transplantation shortens the colonisation period and allows re-entry of patients carrying carbapenamase-producing bacteria into medical care facilities. Int J Antimicrob Agents. 2019;53(4):355–61.
Freedman A, Eppes S. Use of stool transplant to clear fecal colonization with carbapenem-resistant Enterobacteraciae (CRE): proof of concept. Open Forum Infect Dis. 2014;1(suppl.1):S1–65.
Singh R, Van Nood E, Nieuwdorp M, Van Dam B. Donor feces infusion for eradication of extended spectrum beta-lactamase producing Escherichia coli in a patient with end stage renal disease. Eur Soc Clin Infect Dis. 2014;20(11):O977–8.
Jang M-O, An JH, Jung S-I, Park K-H. Refractory Clostridium difficile infection cured with fecal microbiota transplantation in vancomycin-resistant enterococcus colonized patient. Intest Res. 2015;13(1):80–4.
Crum-Cianflone NF, Sullivan E, Ballon-Landa G. Fecal microbiota transplantation and successful resolution of multidrug-resistant-organism colonization. J Clin Microbiol. 2015;53(6):1986–9.
Stripling J, Kumar R, Baddley JW, Nellore A, Dixon P, Howard D, et al. Loss of vancomycin-resistant enterococcus fecal dominance in an organ transplant patient with Clostridium difficile colitis after fecal microbiota transplant. Open Forum Infect Dis. 2015;2:1–8.
Lagier J, Million M, Fournier P, Brouqui P, Raoult D. Faecal microbiota transplantation for stool decolonization of OXA-48 Klebsiella pneumoniae. J Hosp Infect. 2015;90(2):173–4.
Lombardo M, Vulic M, Ohsumi T, Cook D, Henn M, Kraft C, et al. Vancomycin-resistance enterococcal (VRE) titers diminish among patients with recurrent Clostridium difficile infection after administration of SER-109, a novel microbiome agent. Open Forum Infect Dis. 2015;2(suppl_1):S149.
Wei Y, Gong J, Zhu W, Guo D, Gu L, Li N, et al. Fecal microbiota transplantation restores dysbiosis in patients with methicillin resistant Staphylococcus aureus enterocolitis. BMC Infect Dis. 2015;15(1):265.
Bilinski J, Grzesiowski P, Muszynski J, Wróblewska M, Madry K, Robak K, et al. Fecal microbiota transplantation inhibits multidrug-resistant gut pathogens: preliminary report performed in an immunocompromised host. Arch Immunol Ther Exp. 2016;64:255–8.
García-Fernández S, Morosini M-I, Cobo M, Foruny JR, López-Sanromán A, Cobo J, et al. Gut eradication of VIM-1 producing ST9 Klebsiella oxytoca after fecal microbiota transplantation for diarrhea caused by a Clostridium difficile hypervirulent R027 strain. Diagn Microbiol Infect Dis [Internet]. 2016;86(4):470–1. http://linkinghub.elsevier.com/retrieve/pii/S0732889316302917.
Eysenbach L, Allegretti JR, Aroniadis O, Brandt L, Donovan D, Fischer M, et al. Clearance of vancomycin-resistant enterococcus colonization with fecal microbiota transplantation among patients with recurrent Clostridium difficile infection. Open Forum Infect Dis. 2016;3(suppl 1):S599.
Dubberke ER, Mullane KM, Gerding DN, Lee CH, Louie TJ, Guthertz H, et al. Clearance of vancomycin-resistant Enterococcus concomitant with administration of a microbiota-based drug targeted at recurrent Clostridium difficile infection. Open Forum Infect Dis. 2016;3(3):ofw133.
Sohn KM, Cheon S, Kim Y-S. Can fecal microbiota transplantation (FMT) eradicate fecal colonization with vancomycin-resistant enterococci (VRE)? Infect Control Hosp Epidemiol. 2016;37(12):1519.
Stalenhoef JE, Terveer EM, Knetsch CW, van’t Hof PJ, Vlasveld IN, Keller JJ, et al. Fecal microbiota transfer for multidrug-resistant gram-negatives: a clinical success combined with microbiological failure. Open Forum Infect Dis. 2017;4(2):1–4.
Ponte A, Pinho R, Mota M. Fecal microbiota transplantation: is there a role in the eradication of carbapenem-resistant Klebsiella pneumoniae intestinal carriage? Rev Española Enfermedades Dig. 2017;109(5):392.
Davido B, Batista R, Michelon H, Lepainteur M, Bouchand F, Lepeule R, et al. Is faecal microbiota transplantation an option to eradicate highly drug-resistant enteric bacteria carriage? J Hosp Infect. 2017;95(4):433–7. https://doi.org/10.1016/j.jhin.2017.02.001.
Lahtinen P, Mattila E, Anttila VJ, Tillonen J, Teittinen M, Nevalainen P, Salminen S, Satokari RAP. Faecal microbiota transplantation in patients with Clostridium difficile and significant comorbidities as well as in patients with new indications: a case series. World J Gastroenterol. 2017;23:7174.
Innes AJ, Mullish BH, Fernando F, Adams G, Marchesi JR, Apperley JF, et al. Faecal microbiota transplant: a novel biological approach to extensively drug-resistant organism-related non-relapse mortality. Bone Marrow Transplant. 2017;52(10):1452–4.
Singh R, De Groot PF, Geerlings SE, Hodiamont CJ, Belzer C, Berge IJMT, et al. Fecal microbiota transplantation against intestinal colonization by extended spectrum beta-lactamase producing Enterobacteriaceae: a proof of principle study. BMC Res Notes. 2018;11(1):4–9.
Dias C, Pipa S, Duarte-Ribeiro F, Mota M. Fecal microbiota transplantation as a potential way to eradicate multiresistant microorganisms. IDCases. 2018;13:e00432.
Davido B, Batista R, Fessi H, Michelon H, Escaut L, Lawrence C, et al. Fecal microbiota transplantation to eradicate vancomycin-resistant enterococci colonization in case of an outbreak. Med Mal Infect. 2019;49(3):214–8.
Battipaglia G, Malard F, Rubio MT, Ruggeri A, Mamez AC, Brissot E, et al. Fecal microbiota transplantation before or after allogeneic hematopoietic transplantation in patients with hematological malignancies carrying multidrug-resistance bacteria. Haematologica. 2019;104(8):1682–8.
Acknowledgements
Funding
This study was funded by Instituto de Salud Carlos III through the project “PI16/01023” (co-funded by the European Regional Development Fund “Investing in your future”). No funding was received for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Alex Soriano has received grants from Pfizer and is part of the speaker's bureau of Pfizer, MSD, Angelini, Shionogy and Menarini. He has participated in advisory meetings for Pfizer, MSD, Menarini and Shionogy. Alex Soriano is the editor-in-chief of this journal. Andrea Aira, Csaba Fehér and Elisa Rubio declare no conflicts of interest to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.9988634.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Aira, A., Fehér, C., Rubio, E. et al. The Intestinal Microbiota as a Reservoir and a Therapeutic Target to Fight Multi-Drug-Resistant Bacteria: A Narrative Review of the Literature. Infect Dis Ther 8, 469–482 (2019). https://doi.org/10.1007/s40121-019-00272-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-019-00272-7