Abstract
Objective
Although complications and clinical symptoms of COVID-19 have been elucidated, the prevalence of long-term sequelae of COVID-19 is less clear in previously hospitalized COVID-19 patients. This review and meta-analysis present the occurrence of different symptoms up to 1 year of follow-up for previously hospitalized patients.
Methods
We performed a systematic review from PubMed and Web of Science using keywords such as “COVID-19”, “SARS-CoV-2”, “sequelae”, “long-term effect” and included studies with at least 3-month of follow-up. Meta-analyses using random-effects models were performed to estimate the pooled prevalence for different sequelae. Subgroup analyses were conducted by different follow-up time, regions, age and ICU admission.
Results
72 articles were included in the meta-analyses after screening 11,620 articles, identifying a total of 167 sequelae related to COVID-19 from 88,769 patients. Commonly reported sequelae included fatigue (27.5%, 95% CI 22.4–33.3%, range 1.5–84.9%), somnipathy (20.1%, 95% CI 14.7–26.9%, range 1.2–64.8%), anxiety (18.0%, 95% CI 13.8–23.1%, range 0.6–47.8%), dyspnea (15.5%, 95% CI 11.3–20.9%, range 0.8–58.4%), PTSD (14.6%, 95% CI 11.3–18.7%, range 1.2–32.0%), hypomnesia (13.4%, 95% CI 8.4–20.7%, range 0.6–53.8%), arthralgia (12.9%, 95% CI 8.4–19.2%, range 0.0–47.8%), depression (12.7%, 95% CI 9.3–17.2%, range 0.6–37.5%), alopecia (11.2%, 95% CI 6.9–17.6%, range 0.0–47.0%) over 3–13.2 months of follow-up. The prevalence of most symptoms reduced after > 9 months of follow-up, but fatigue and somnipathy persisted in 26.2% and 15.1%, respectively, of the patients over a year. COVID-19 patients from Asia reported a lower prevalence than those from other regions.
Conclusions
This review identified a wide spectrum of COVID-19 sequelae in previously hospitalized COVID-19 patients, with some symptoms persisting up to 1 year. Management and rehabilitation strategies targeting these symptoms may improve quality of life of recovered patients.
Similar content being viewed by others
Introduction
Since its emergence in December 2019, SARS-CoV-2 has rapidly spread around the world, leading to > 480 million confirmed cases and > 6 million deaths as of March 2022 [1]. As more people have recovered from COVID-19, the long-term sequelae of the disease and its impact to the healthcare system have become an important consideration.
Evidence has shown that hospitalized COVID-19 patients would develop various complications, including pneumonia (75%), acute liver injury (19%), heart injury (7% to 17%), acute respiratory distress syndrome (15%), acute kidney injury (9%), acute heart failure, disturbance of consciousness, etc. [2] A noticeable portion of hospitalized patients would also show symptoms such as fever (70–90%), shortness of breath (53–80%), dry cough (60–86%), myalgia (15–44%), fatigue (38%), nausea/vomiting or diarrhea (15–39%), weakness (25%), headache, loss of taste, loss of smell, etc. [3] Although these complications and symptoms have been elucidated in hospitalized patients, their persistence after recovery has not been clearly described to assess how quality of life is affected among the recovered patients. Up to now, 12 meta-analyses studied the long-term sequelae with follow-up time > 3 months [4,5,6,7,8,9,10,11,12,13,14,15]. Only two of them stratified the prevalence of headache, myalgia, arthralgia, and chest pain among hospitalized patients by < 6 and > 6 months follow-up [9, 10]. However, none of them reported prevalences of a wide range of symptoms among previously hospitalized patients at different months of follow-up which showed the time trend [11]. Hospitalized patients are more likely to suffer from more severe post-COVID symptoms; hence there is a need to clarify their severity and persistence.
Here we carried out a systematic review and meta-analysis of sequelae of hospital discharged COVID-19 patients to identify all aftermaths of COVID-19, which can help to prevent and manage the long-term sequelae of the discharged COVID-19 patients. In our study we focused on previously hospitalized patients who had more severe symptoms and more sequelae, and also focused on articles with at least a 3-month follow-up time, to study sequelae which likely have a longer impact on their quality of life. Our study will also provide pooled estimates at 12 months follow-up. Such information would inform health management strategies of COVID-19 patients by identifying sequelae that may persistently affect the quality of life.
Methods
Search strategy and eligibility criteria
This systematic review and meta-analysis followed the PRISMA guidelines [16]. The protocol was registered in PROSPERO (register no: CRD42022314319). Studies about long-term sequelae of COVID-19 were identified through PubMed and Web of Science for publications up to 1 March 2022 Search queries included terms such as “COVID-19”, “SARS-CoV-2”, “2019-nCoV”, “sequelae”, “long-term effect”, “long-term consequence”, “long-term manifestations”, “persistent effect”, “persistent symptom”, “persistent manifestations”, “post COVID-19 effect”, “post COVID-19 symptom”, “post COVID-19 manifestations” and “post COVID-19 syndrome” (Appendix 1). Reference lists of systematic reviews were also reviewed. We included studies published in English.
The eligibility criteria were as follows:(1) study designs included cohort studies, case–control studies, and cross-sectional studies with a clear follow-up duration.; (2) patients should be hospital discharged adult patients aged 18 years or above representative of the general population without any age restriction, with a pathologically confirmed COVID-19 infection; (3) patients should be confirmed before 2022 to exclude patients infected with the omicron variant which may have a different symptom profile (4). Outcomes were defined as all clinical symptoms after at least 90 days after discharge, admission, diagnosis or symptom onset, consistent with case definition of post COVID-19 condition by the World Health Organization [17]. Sequelae of COVID-19 included respiratory, cardiovascular, psychosocial, neurological, dermatological, digestive, endocrinological symptoms and other symptoms. Studies reporting serological, immunological results or CT scores only were excluded. (5) Sample size > 100.
Data extraction and quality assessment
Data Extraction and Quality Assessment were conducted by two independent reviewers (TY & XL). Any disagreement was solved by a senior author (EHYL). Extracted data included the first author, year of publication, sample size, disease severity, average follow-up period, the average age of participants, and clinical symptoms defined before.
Study quality was evaluated by using the Newcastle–Ottawa Scale (NOS) [18]. Studies with 7–9 stars were perceived as high quality and studies with < 4 stars were perceived as poor quality. We assessed quality in selection strategies (representativeness of the exposed cohort, ascertainment of exposure, etc.), comparability, and outcome (outcome assessment, follow-up rate, etc.).
Statistical analysis
For those sequelae reported in two or more studies, the pooled prevalence and 95% CI were estimated in a meta-analysis using a random-effects model (the variance component was estimated using the DerSimonian–Laird estimator) and inverse variance methods following logit transformation [19]. For those sequelae reported only in a single study, the prevalence was estimated by directly dividing the number of cases who shown symptoms by the total sample size, and the 95% CI was estimated by using the Clopper-Pearson interval. Boxplots, median and interquartile ranges (IQR) were present for sequelae reported by ten or more studies.
The chi-square-based Cochran’s Q test and Higgins (I2) statistics were used to assess the heterogeneity of studies included in the meta-analysis. The significance level of Cochran’s Q test was 0.05. Studies were regarded as having low, moderate and high heterogeneity with I2 = < 30%, 30–60% and > 60%, respectively. Subgroup analysis was conducted for those meta-analyses which included 15 or more studies, by different follow-up duration, regions, ICU admission and age. Meta-regression was used to test whether the difference of estimates between subgroups is significant. The pooled follow-up duration was weighted by sample size of each study. All statistical analyses were conducted in R version 4.0.3 (R Development Core Team).
Results
Study characteristics
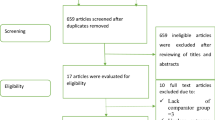
A total of 11,620 studies were identified from PubMed and Web of Science, and one study was identified from other systematic reviews (Fig. 1). After removing 1301 duplicates, 10,320 articles were screened against title and abstract, and 10,062 articles not meeting the eligibility criteria were excluded. Finally, a total of 72 articles were included in the meta-analysis by screening the full texts of 256 articles: 19 articles did not have clinical symptoms as outcomes; 35 articles had a less than 3-month follow-up time; 40 articles included less than 100 participants; 70 articles did not only include hospitalized patients; 4 articles did not report follow-up time; 3 articles did not report prevalence in sequelae; 13 duplicate publications were further identified.
All included articles were published between 2020 and 2022. Of the 72 studies included in our analysis, 15 studies were from China, 11 each from Italy and Spain, 5 from England, 4 from France, 3 each from America and Mexico, 2 each from India, Germany, Switzerland and Belgium, 1 each from Iran, Australia, Egypt, Brazil, Peru, Turkey, Pakistan, Singapore, Austria, Kingdom of Saudi Arabia, Denmark and Netherlands (Table 1). All studies were observational studies: 62 non-controlled cohort studies, 5 controlled cohort studies, 4 cross-sectional studies and 1 case–control study. Data from the control groups (non COVID-19 cases) were not included in our analysis. One article conducted two independent telephone and outpatient follow-ups [35]. The two surveys reported different sequelae, and hence were regarded as two independent studies and included in the meta-analysis, while data on cough was included from the telephone follow-up only. Four articles which included one same cohort were included in the meta-analysis as four independent studies as they reported different symptoms [21,22,23,24]. The average follow-up time ranged from 90 days to 13.2 months and the size of follow-up cohorts ranged from 101 to 47,780. Only patients hospitalized for COVID-19 were included (Fig. 2).
The quality of studies was assessed by NOS and no articles were rated as poor quality (Appendix 2). Only five studies (6.9%) were rated high quality. The majority of studies were non-controlled cohort studies and did not meet the standard of comparability.
Meta-analysis of prevalence of sequelae related to COVID-19
A total of 167 sequelae related to COVID-19 were identified in the systematic review, including respiratory/lung function, cardiovascular, psychosocial, neurological, dermatological, digestive system, endocrinological system and other sequelae. 92 sequelae were reported by two or more studies and their pooled prevalence was presented (Table 2). These sequelae were reported during 90 days to 13.2 months of follow-up.
Respiratory/lung function sequelae
The most common sequelae in the respiratory system were shortness of breath (14 studies) with a prevalence of 25.6% (95% CI 15.1–39.8%, range 3.7–59.7%) and post-activity polypnea (3 study) with the prevalence of 29.8% (95% CI 20.5–41.3%, range 21.4–42.3%), followed by dyspnea (35 studies), pain on breathing (2 studies), chest distress (8 studies), cough (40 studies), with prevalence of 15.5% (95% CI 11.3–20.9%, range 0.8–58.4%), 13.9% (95% CI 11.9–16.2%, range 13.1–14.3), 10.8% (95% CI 6.8–16.8%, range 3.2–29.6%) and 9.8% (95% CI 7.8–12.4%, range 0.0–35.2%), respectively.
Cardiovascular sequelae
The most common sequela was resting heart rate increase (1 study) with prevalence of 11.2% (95% CI 8.8–14.1%). 18 studies reported palpitations with pooled estimate of 6.6% (95% CI 4.4–9.8%, range 0.5–23.2%).
Psychosocial sequelae
Somatization (2 studies) was the most common psychosocial sequela with a prevalence of 37.5% (95% CI 30.2–45.3%, range 34.0–41.8%). More than ten studies measured somnipathy, anxiety, PTSD and depression with a pooled prevalence of 20.1% (14.6–26.9%, range 1.2–64.8%), 18.0% (95% CI 13.8–23.1%, range 0.6–47.8%), 14.6% (95% CI 11.3–18.7%, range 1.2–32.0%) and 12.7% (95% CI 9.3–17.2%, range 0.6–37.5%), respectively.
Neurological sequelae
More than ten studies reported that recovered patients had fatigue, concentration problem, hypomnesia arthralgia, myalgia, headache, dizziness, ageusia, anosmia and movement disturbances, among which fatigue had the highest prevalence of 27.5% (95% CI 22.4–33.3%, range 1.5–84.9%). Meanwhile, one study each reported that the prevalence of bradykinesia and cognitive complaint were up to 49.9% and 49.7%.
Dermatological sequelae
10 and 11 articles reported sweating (6.4% 95% CI 3.5–11.7%, range 0.0–28.5%) and exanthema (4.6% 95% CI 2.7–7.7%, range 0.2–16.0%), respectively. However, a study reported that the prevalence of changing pattern of sweating was 28.5% (95% CI 20.9–37.0%).
Sequelae related to the digestive system
Poor appetite, abdominal pain and diarrhea were reported by more than ten studies, respectively, with a pooled prevalence of 5.7% (95% CI 3.5–9.0%, range 0.0–26.9%), 3.5% (95% CI 1.6–7.3%, range 0.0–17.7%) and 2.9% (95% CI 1.8–4.9%, range 0.0–17.7%), respectively. In addition, two studies reported that 15.3% (95% CI 2.1–59.8%, range 5.8–34.6%) of patients had stomach bloated after meals.
Sequelae-related endocrinological system
The prevalence of dermatological sequelae was generally low. The most common sequela related to the endocrinological system was alopecia, with a pooled prevalence of 11.2% (95% CI 6.9–17.6%, range 0.0–47.0%) from 17 articles.
Other sequelae
Among the remaining sequelae, intolerance to temperature, urinary frequency, musculoskeletal pain and erectile dysfunction were common, with prevalences of 30.8% (95%CI 23.0–39.5%), 23.1% (95% CI 16.1–31.3%), 17.3% (95% CI 11.1–25.8%, range 4.2–50.8%) and 17.2% (95% CI 12.2–23.6%, range 13.8–23.4%), respectively.
Heterogeneity analysis and sensitivity analysis
Most of the sequelae prevalence had high heterogeneity across studies (I2 > 60%, PH < 0.05). Six meta-analyses showed low heterogeneity (pain on breathing: I2 = 0.00%, PH = 0.628, wheezing: I2 = 0.00%, PH = 0.613, orthopnea: I2 = 0.00%, PH = 0.984, problems with usual activity: I2 = 0.00%, PH = 0.766, myoclonus: I2 = 0.00%, PH = 0.584, anorexia: I2 = 0.00%, PH = 0.632), one showed moderate heterogeneity (anger-hostility: I2 = 44.3%, PH = 0.180).
Subgroup analysis
Temporal trend of symptoms
We present prevalence of symptoms at different follow-up time (3–4, 5–8 and > 9 months). Overall, the prevalence of all symptoms showed higher prevalences at 5–8 months’ follow-up (Appendix 3 and Fig. 3). The prevalence of most symptoms decreased at > 9 months, except fatigue, dyspnea, depression, arthralgia, anosmia, ageusia and dizziness. The prevalence of PTSD and chest pain decreased from 3–4 to > 9 months with significant difference, and alopecia decreased significantly from 3–4 to 5–8 months. Heterogeneity in most symptoms was still high after stratification by follow-up duration (I2 > 60.0%, PH < 0.05). Only fever at > 9 months’ follow-up had a low heterogeneity (I2 = 22.0%, PH = 0.279).
Symptoms by geographic regions
We further analyzed the prevalence of symptoms by geographic regions. Overall, the pooled prevalence of symptoms in Asia was lower than that in Europe and other regions (Appendix 4 and Fig. 4). Additionally, the heterogeneity in symptoms was still high (I2 > 60.0%, PH < 0.05), except fever in regions out of Asia and Europe (I2 = 0.0%, PH = 0.628). Europe reported higher prevalences than Asia in fatigue, dyspnea, anxiety, anosmia, ageusia and headache with significant difference.
Symptoms by age
We estimated the prevalence of symptoms by age (< 60 years old and ≥ 60 years old). Overall, the pooled prevalence of symptoms in < 60 years old was higher than that in ≥ 60 years old (Appendix 5 and Fig. 5), except dyspnea, PTSD, anosmia, myalgia, cough, ageusia and headache. The heterogeneity in symptoms was still high (I2 > 60.0%, PH < 0.05). Patients < 60 years old reported higher prevalences than those ≥ 60 years old in palpitation and sore throat with significant difference.
Symptoms by ICU admission
We showed the prevalence of symptoms by ICU admission (< 20% and ≥ 20%). Overall, the pooled prevalence of symptoms in < 20% ICU admission was lower than that in 20% ICU admission (Appendix 6 and Appendix 7), except depression and alopecia. The heterogeneity in symptoms was still high (I2 > 60.0%, PH < 0.05). Studies with < 20% ICU admission reported lower prevalences than studied ≥ 20% ICU admission in dizziness and fever.
Discussion
This systematic review and meta-analysis identified 167 sequelae related to COVID-19 from 88,769 patients at least 90 days follow-up after hospital discharge. These included respiratory/lung function, cardiovascular, psychosocial, neurological, dermatological, digestive system and endocrinological system sequelae. We identified symptoms such as fatigue, somnipathy, dyspnea, anxiety, depression, PTSD and arthralgia which persisted for 1 year in the discharged COVID-19 patients. The prevalence of some neurological symptoms (fatigue, arthralgia, anosmia, ageusia and dizziness) did not show decreasing trends up to 1 year of follow-up, while most of the other symptoms resolved over time.
Respiratory/lung function sequelae
Shortness of breath (25.6%) and post-activity polypnea (29.8%) were the 2 most common sequelae in the respiratory system. Furthermore, some patients who recovered from COVID-19 would develop symptoms, including dyspnea (15.5%), pain on breathing (13.9%), chest distress (10.8%), cough (9.8%), etc. These symptoms can be explained by the influence of COVID-19 on the lungs. The current evidence indicates that the organ most affected by COVID-19 is the lung, which may cause a variety of pathophysiological events, including capillary damage and bleeding, hyaline membrane formation, pulmonary consolidation, diffuse alveolar epithelium destruction, and alveolar septal fibrous proliferation [92, 93]. COVID-19 can extensively damage the alveolar epithelial cell and the endothelial cell with secondary fibroproliferation, which may cause lung fibrosis or pulmonary hypertension by chronic vascular and alveolar remodeling [94, 95].
Clinically, the pathological changes can significantly affect activities of daily living, by reduction of walking distance in the 6-min walking test [32]. A systematic review and meta-analysis have found that 39%, 15% and 7% of COVID-19 patients had altered diffusion capacity, restrictive pattern, and obstructive pattern, respectively, in lungs [96]. Radiological and pathological report showed pulmonary fibrosis, parenchymal bands, irregular interfaces, reticular opacities and traction bronchiectasis with or without honeycomb lung [97,98,99,100]. Additionally, varying degrees of alveolar structure destruction and pulmonary interstitial fibrosis were observed in the autopsy of patients with COVID-19 [101].
The underlying pathophysiology of post-COVID sequelae is multifaceted and subject to debate. It can be classified into lung-dependent direct tissue injury, and lung-independent pathological inflammation such as viral persistence, immune dysregulation, and autoimmunity [102, 103]. Radiologically, post-COVID decline in pulmonary function is closely associated with pulmonary fibrosis and ground glass opacification [35, 104,105,106]. An investigation of autopsy samples demonstrated viral persistence, resulting in multiple organ injury and various clinical presentations [107]. The role of inflammatory biomarkers in its pathogenesis is discordant since some studies have observed a persistently elevated biomarkers [103, 108, 109], while some researchers also show there is no direct correlations between them [110].
The evidence showed that the lungs have the potential to heal after severe injury, which is consistent with the downtrend of the prevalence in cough, chest pain and sore throat [111]. However, we also observed that dyspnea persisted in 13.1% of the discharged COVID-19 patients for over a year, which suggested that lung injury may affect patients for a longer duration. Evidence from SARS and MERS reported that some patients still have lung damage even 15 years later [112]. Therefore, a specialized rehabilitation program is important. One study has shown that a 6-week rehabilitation program can significantly improves pulmonary functions, quality of life and anxiety in COVID-19 survivors [113]. Early rehabilitation is beneficial to functional recovery and functional independence of patients [114, 115]. Therefore, several professional bodies advocated the need of early detection and rehabilitations. The British Thoracic Society recommended regular follow-up of high-risk patients 4 months after infection; and the Swiss COVID group and Swiss Society for Pulmonology recommended detailed pulmonary assessments and rehabilitations, if resources are available [116, 117].
Cardiovascular sequelae
Resting heart rate increase were the most common sequelae in the cardiovascular system with the prevalence of 11.2%, which may be related to heart damage caused by COVID-19. A study of recovered COVID-19 patients reported that almost 78% of patients had heart involvement and 60% of them had persistent inflammation of the heart muscle unrelated to a pre-existing condition [118]. Cardiovascular sequelae may recover as we found that the prevalence of palpitation decreased slightly over time. It is important to note that even with a significant recovery of heart function, there may still be a risk of coronary artery disease, atrial fibrillation, or ventricular arrhythmias due to myocardial injury [119].
Patients with cardiovascular sequelae require close monitoring because the post-discharge mortality rate is high, with near half of the patients dying 3 months after discharge [120]. These patients should be referred for clinical reviews and reassessment 1–2 months after discharge [121, 122]. Postural Orthostatic Tachycardia Syndrome (POTS) has been reported in COVID-19 survivors [123]. They may be presented as easy fatigue, postural tachycardia, dizziness and exercise intolerance [124]. The proposed mechanism has been an alteration of autonomic nervous system regulated by angiotensin converting enzyme 2 (ACE2) protein found on neurons [125].
Psychosocial sequelae
The sequelae related to mental health were of common occurrence in COVID-19, such as somatization (37.5%), phobic-anxiety (24.2%), somnipathy (20.1%), anxiety (18.0%), PTSD (14.6%) and depression (12.7%). Meanwhile, the experience with SARS and MERS also showed that the prevalence of depression, anxiety and post-traumatic stress disorder remained high even after 39 months, which indicates that the mental health of patients is of great concern after they recovered from COVID-19 [126]. We observed that the prevalence of somnipathy, anxiety and depression was still high after a year (15.1%, 12.9% and 12.6%, respectively). Reason of psychosocial sequelae is proposed to be inflammatory marker-mediated neuroinflammatory damages since cytokines IL-4 and IL-6 are persistently elevated in patients reported with neurological or psychological symptoms [127]. Other inflammatory markers reported include amyloid-beta, neurofilament light, neurogranin, total tau and p-T181-Tau [128]. Nearly half of survivors without prior psychiatric conditions live with depression after 3 months of recovery from severe COVID-19 associated respiratory failure [129].
Neurological sequelae
A great number of neurological sequelae have been found in this systematic review and meta-analysis. Among these sequelae, bradykinesia (49.9%), cognitive complaint (49.7%), inability to focus vision (33.1%), problems with balance (28.3%), fatigue (27.5%), abnormal reflex status (26.2%), sensory alterations (25.9%), brain fog (25.0%), arthritis (24.6%), unrefreshing sleep (21.9%), cognitive impairment (21.2%), neck pain (21.1%), voice alteration (20.8%) and light sensitivity (20.0%) had a relatively high prevalence. They may be related to viral infection, physiological impairment (e.g., hypoxia), cerebrovascular disease, immunoreaction, side effects of medication, etc. [126] Reason of neurological dysfunction can be explained macroscopically and microscopically. Macroscopically, hypoxic nerve damage leads to mitochondrial swellings in various brain sites, such as cerebral white matters, brainstem, parahippal gyrus, thalamus and sites with high metabolic requirements [130,131,132,133]. Neurons do not readily regenerate; thus, these clinical presentations may be long-lasting, leading to Long COVID-19 syndrome [134]. Microscopically, persistently elevated cytokines were observed in patients with neurological presentations. Multifocal neurological damages in patients with Long COVID-19 Syndrome may be a result from indirect T-cell and microglia damage in the brain, similar to stroke and neuroinflammatory diseases [135]. Additionally, lung sequelae are also believed to be a major cause of fatigue [136].
However, the downtrend was not observed in neurological sequelae, and the prevalence was still high in fatigue (26.2%) and arthralgia (11.5%) after a year.
Dermatological sequelae
Ten and 11 articles reported that COVID-19 recovered patients would have sweating and exanthema with a low prevalence of 6.4% and 4.6%, respectively. González-Hermosillo et al. reported that 28.5% of patients would change pattern of sweating at 6-month follow-up after discharge [43]. These dermatological sequelae may be caused by the drug used to treat COVID-19, maybe because of the long-term effect of COVID-19, or maybe because of some random effects (wrong measurement, the patient happened to have this sequela, etc.). Further studies are needed to determine whether COVID-19 can cause dermatological sequelae.
Sequelae related to the digestive system
14 studies reported poor appetite, with a pooled prevalence of 5.7%. This may be related to the anosmia and the ageusia caused by COVID-19, and elevated levels of inflammatory cytokines are also a common cause of anorexia [137]. Stomach bloated after meals and hyplyphagia occurred frequently (15.3% and 9.5%). Additionally, a small number of patients also had abdominal pain, diarrhea, vomiting, and other sequelae, which are also developed during the acute phase of COVID-19. This may be because the SARS-CoV-2 replicates in the gastrointestinal tract and then infects and destroys absorbent intestinal cells. Or the gastrointestinal system is directly damaged by the COVID-19 induced inflammation [138]. Meanwhile, we observed that the prevalence of diarrhea decreased with the increase of follow-up time.
Although the observed prevalence of hepatic insufficiency was low (0.2%), liver injury has been observed in various studies of COVID-19 survivors [139, 140]. Majority of the survivors showed gradual normalization of liver function enzymes within 2 months after discharge [141]. However, patients with chronic liver conditions (such as liver cirrhosis) are associated with a fourfold increase of mortality risk after COVID-19 infections, compared with those without [142]. Thus, COVID-19 survivors with chronic liver conditions should be prioritized for rehabilitations follow-up.
Sequelae-related endocrinological system
Alopecia was the most common sequela related to the endocrinological system with a pooled prevalence of 11.2%. However, it is apparently lower than another systematic review which reported a pooled prevalence of 25% [143]. It may be because the follow-up time of this systematic review is shorter than mine, the symptom of alopecia may have been alleviated. The alopecia developed after COVID-19 can be referred to as telogen effluvium, defined as a diffuse hair loss after significant systemic stressors or infection, which is due to premature follicular transitions from the active growth phase (anagen) to the resting phase (telogen) [144]. Generally, it will last about 3 months. Therefore, we observed that the prevalence of alopecia decreased by 20.9% from 3 – 4 months to 5 –8 months.
Another Long-COVID related endocrinopathy is diabetes mellitus (DM). Proposed pathogenic mechanism is SARS-CoV-2 binding to ACE2 receptors of pancreatic beta-islet cells, triggering autoimmune response and type I DM [145, 146]. Thus, hyperglycemia without DM and new-onset DM are associated with poor prognosis COVID-19 after excluding risk factors such as obesity and corticosteroid administration [147].
Other sequelae
Weight loss (10.6%) and malnutrition are common in patients who recover from COVID-19. Another study that evaluated the COIVD-19 patients after clinical remission, also found that more than 50% of them were at risk of malnutrition and approximately 30% of them lost more than 5% of weight compared with baseline [148]. This may be because acute systemic inflammation can severely affect several metabolic and hypothalamic pathways, leading to decreased anorexia and food intake as well as increased resting energy expenditure and muscle catabolism [149]. Additionally, erectile dysfunction (18.6%) was found as a sequela of COVID-19, which may be because of psychological distress, endothelial dysfunction, subclinical hypogonadism, or impaired pulmonary hemodynamics [149]. Moreover, the urinary symptoms (urinary frequency, difficulty emptying bladder, problems passing urine) may be because of viral cystitis caused by SARS-COV-2, and further research is needed [150]. The musculoskeletal pain is also a common post-COVID symptom. The muscular nociception is neurologically and immunologically mediated in Long COVID-19 Syndrome. Its pathogenesis is related to muscle injury secondary to hyperinflammatory state [71, 151, 152], leading to to ACE-2 mediated injury with elevated inflammatory & nociceptive immune markers, e.g. IL2, IL7, IL10, IL-6, TNFα. These are amendable by pharmacological and non-pharmacological interventions by pain-modulation pathways to facilitate future rehabilitations. High prevalence of intolerance to temperature (30.8%) reported by González-Hermosillo et al. cannot be explained yet, and needs more further researches.
Our subgroup analysis showed that the prevalence of most COVID-19 sequelae decreased after > 9 months of follow-up, except that fatigue, somnipathy, dyspnea, depression, arthralgia, anosmia and ageusia remained stable for a longer time. However, the prevalence of most sequelae increased at 5 – 8 months. A similar pattern in a meta-analysis by Alkodaymi et al., prevalences of symptoms at 6 – 9 months were higher than others and did not decrease noticeably afterwards for some symptoms such as fatigue, dyspnea and sleep disorder [11]. Other explanation could be studies reporting sequelae at 5–8 months had a higher proportion of ICU admission, and were mostly from regions out of Asia, while studies of 3–4 months and ≥ 9 months were all from Asia. Furthermore, Asia showed lower prevalence than regions out of Asia, except for anxiety and depression. As a majority of Asian studies (15/22) were from China, the lower prevalence may be explained by admission of milder patients in China, whereas most mild patients were treated at home in other regions. A study from Wuhan, China reported that the condition of 93% of patients in the general ward was not serious, compared to 77% in East London, UK [153, 154]. It may also be explained by younger age and lower pre-existing medical comorbidities among Chinese patients [155]. Additionally, some symptoms in patients aged < 60 years had significantly higher prevalence than that in patients aged ≥ 60 years, such as anxiety, palpitation and sore throat (Appendix 5 and Fig. 5), while other studies found that COVID-19 patients of different age groups may exhibit different sets of clinical symptoms [156]. Finally, the pooled prevalence of symptoms tends to be higher among studies with more severe patients (i.e. higher % of ICU admission). Other factors such as treatment, rehabilitation, race and blood type may also affect symptom persistence [157, 158].
The heterogeneity of most meta-analyses was high and from our subgroup analyses it could not be explained by follow-up time, regions, age or ICU admission. Possible source of heterogeneity may include differences in the determination of symptoms (questionnaire or self-report or diagnosis by doctors), the proportion of sex, drug use, etc. We did not perform meta-regression analysis to further identify the source of heterogeneity due to the limited number of studies for each symptom.
One strength of this study is that this systematic review and meta-analysis studied all potential long-term sequelae (> 3 months) in hospital discharged COVID-19 patients. The review presented a wide spectrum of health burdens among hospital recovered COVID-19 patients and informed management strategies of COVID-19 discharged patients. Currently, different long COVID-19 clinical assessment tools have been proposed, such as Newcastle post-COVID syndrome Follow Up Screening Questionnaire and COVID-19 Yorkshire Rehabilitation Scale [159, 160]. This study provided clues for standardization of rehabilitation baseline assessment based on symptom prevalence and severity. The focus on hospitalized patients would be of clinical significance and provided most relevant information for hospital-based rehabilitation strategies and services. The meta-analysis by Maglietta et al. described symptoms > 3 months for hospitalized COVID-19 patients, but did not further analyze the prevalence over time [14]. The meta-analysis by Alkodaymi et al. presented symptom prevalence over time, but did not stratify by hospitalized and non-hospitalized COVID-19 patients [11].
There are also some limitations. First, there was large heterogeneity in the prevalence estimates and hence the pooled prevalence should be interpreted with caution. There could be differences in the assessment or reporting of symptoms which contributed to the heterogeneity between studies. Second, some sequelae had a small sample size so that the pooled estimate may not be generalized. Third, clinical symptoms may have various diagnostic standards and symptoms such as cough and chest pain were mainly self-reported [20, 25, 29,30,31, 36, 38, 40,41,42,43, 46, 47, 51,52,53,54,55,56,57,58, 60, 62, 74, 80, 81, 86, 88, 89, 91], as healthcare resources were already stretched coping with the evolving pandemic. Finally, the excess burden of each sequela compared to the general population was not quantified which were available from a limited number of controlled cohort studies only.
This systematic review and meta-analysis indicated that post-COVID symptoms are common in hospital discharged patients. A noticeable proportion of discharged COVID-19 patients still reported fatigue and somnipathy after 1 year of follow-up. Therefore, it is imperative to develop and implement effective preventive and rehabilitative measures for hospitalized COVID-19 patients and COVID-19 survivors after discharge, such as inhibiting viral replication, blocking the inflammatory response and early preventive treatment. Furthermore, post-discharge monitoring is essential to monitor the progress of these sequelae and take treatment measures timely. A recent study suggested community rehabilitative approach in COVID-19 survivors stratified by different clinical severity [161]. In view of the enormous populations, patients with mild severity should be monitored with digital interventions, while moderate and severe patients should have regular follow-up and rehabilitation sessions. Additionally, the mental health of COVID-19 recovered patients is deeply influenced because of social isolation, the psychological impact of new and potentially fatal diseases, fear of infecting others and stigma [126]. Therefore, continuous psychological evaluation after hospital discharge is necessary. Individuals who have depression, anxiety, or PTSD may need psychological intervention from an occupational therapist, social worker, or rehabilitation psychologist [162]. Moreover, because recovered COVID-19 patients often experience weight loss and malnutrition, diagnosis, prevention and treatment of malnutrition should be considered in the previously hospitalized COVID-19 patient management strategy to improve short- and long-term outcomes, as suggested by the European Society of Enteral and Parenteral Nutrition (ESPEN) [163]. Meanwhile, there are still limited therapeutic options for COVID-19 infections and long COVID-19, preventive measures such as vaccinations, masks, personal hygiene and social distancing should be stressed [164, 165].
Conclusion
Post-COVID symptoms affected some of the hospital discharged patients persistently for around 1 year, such as fatigue (26.2%), somnipathy (15.1%), anxiety (12.9%), dyspnea (13.1%), arthralgia (11.5%), depression (12.6%), alopecia (10.5%), etc. A multidisciplinary approach is required to develop preventive measures, rehabilitation techniques and clinical management strategies to reduce the impact of COVID-19 sequelae on patients’ lives.
References
World Health Organization. WHO coronavirus (COVID-19) Dashboard [internet]. [2022-04-01]. https://covid19.who.int/.
Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–93. https://doi.org/10.1001/jama.2020.12839.
Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, Shen J, Zhu LR, Chen Y, Iacucci M, Ng SC. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:667–78. https://doi.org/10.1016/S2468-1253(20)30126-6.
Iqbal FM, Lam K, Sounderajah V, Clarke JM, Ashrafian H, Darzi A. Characteristics and predictors of acute and chronic post-COVID syndrome: a systematic review and meta-analysis. EClinicalMedicine. 2021;1: 100899. https://doi.org/10.1016/j.eclinm.2021.100899.
Sanchez-Ramirez DC, Normand K, Zhaoyun Y, Torres-Castro R. Long-term impact of COVID-19: a systematic review of the literature and meta-analysis. Biomedicines. 2021;9:900. https://doi.org/10.3390/biomedicines9080900.
Michelen M, Manoharan L, Elkheir N, Cheng V, Dagens A, Hastie C, O’Hara M, Suett J, Dahmash D, Bugaeva P, Rigby I. Characterising long COVID: a living systematic review. BMJ Glob Health. 2021;6: e005427. https://doi.org/10.1136/bmjgh-2021-005427.
Ceban F, Ling S, Lui LM, Lee Y, Gill H, Teopiz KM, Rodrigues NB, Subramaniapillai M, Di Vincenzo JD, Cao B, Lin K. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immunity. 2021. https://doi.org/10.1016/j.bbi.2021.12.020.
Premraj L, Kannapadi NV, Briggs J, Seal SM, Battaglini D, Fanning J, Suen J, Robba C, Fraser J, Cho SM. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci. 2022;15: 120162. https://doi.org/10.1016/j.jns.2022.120162.
Fernández-de-las-Peñas C, Navarro-Santana M, Gómez-Mayordomo V, Cuadrado ML, García-Azorín D, Arendt-Nielsen L, Plaza-Manzano G. Headache as an acute and post-COVID-19 symptom in COVID-19 survivors: a meta-analysis of the current literature. Eur J Neurol. 2021;28:3820–5. https://doi.org/10.1111/ene.15040.
Fernández-de-Las-Peñas C, Navarro-Santana M, Plaza-Manzano G, Palacios-Ceña D, Arendt-Nielsen L. Time course prevalence of post-COVID pain symptoms of musculoskeletal origin in patients who had survived to SARS-CoV-2 infection: a systematic review and meta-analysis. Pain. 2021. https://doi.org/10.1097/j.pain.0000000000002496.
Alkodaymi MS, Omrani OA, Fawzy NA, Abou Shaar B, Almamlouk R, Riaz M, Obeidat M, Obeidat Y, Gerberi D, Taha RM, Kashour Z. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. 2022. https://doi.org/10.1016/j.cmi.2022.01.014.
Behnood SA, Shafran R, Bennett SD, Zhang AX, O’Mahoney LL, Stephenson TJ, Ladhani SN, DeStavola BL, Viner RM, Swann OV. Persistent symptoms following SARS-CoV-2 infection among children and young people: a meta-analysis of controlled and uncontrolled studies. J Infect. 2021. https://doi.org/10.1016/j.jinf.2021.11.011.
Han Q, Zheng B, Daines L, Sheikh A. Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens. 2022;11:269. https://doi.org/10.3390/pathogens11020269.
Maglietta G, Diodati F, Puntoni M, Lazzarelli S, Marcomini B, Patrizi L, Caminiti C. Prognostic factors for post-COVID-19 syndrome: a systematic review and meta-analysis. J Clin Med. 2022;11:1541. https://doi.org/10.3390/jcm11061541.
Rao S, Benzouak T, Gunpat S, Burns RJ, Tahir TA, Jolles S, Kisely S. Fatigue symptoms associated with COVID-19 in convalescent or recovered COVID-19 patients; a systematic review and meta-analysis. Ann Behav Med. 2022;56:219–34. https://doi.org/10.1093/abm/kaab081.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34. https://doi.org/10.1016/j.jclinepi.2009.06.006.
World Health Organization. A clinical case definition of post COVID-19 condition by a Delphi consensus. 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www3.med.unipmn.it/dispense_ebm/2009-2010/Corso%20Perfezionamento%20EBM_Faggiano/NOS_oxford.pdf.
Wang N. How to conduct a meta-analysis of proportions in R: a comprehensive tutorial. John Jay College of Criminal Justice, New York, 0-62. 2018. https://doi.org/10.13140/RG.2.2.27199.00161
Xiong Q, Xu M, Li J, Liu Y, Zhang J, Xu Y, Dong W. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clin Microbiol Infect. 2021;27:89–95. https://doi.org/10.1016/j.cmi.2020.09.023.
Fernández-de-Las-Peñas C, Guijarro C, Plaza-Canteli S, Hernández-Barrera V, Torres-Macho J. Prevalence of post-COVID-19 cough one year after SARS-CoV-2 infection: a multicenter study. Lung. 2021;199:249–53. https://doi.org/10.1007/s00408-021-00450-w.
Fernández-de-Las-Peñas C, Pellicer-Valero OJ, Navarro-Pardo E, Palacios-Ceña D, Florencio LL, Guijarro C, Martín-Guerrero JD. Symptoms experienced at the acute phase of SARS-CoV-2 infection as risk factor of long-term post-COVID symptoms: the LONG-COVID-EXP-CM multicenter study. Int J Infect Dis. 2022. https://doi.org/10.1016/j.ijid.2022.01.007.
Fernández-de-La-Speñas C, de-la-Llave-Rincón AI, Ortega-Santiago R, Ambite-Quesada S, Gómez-Mayordomo V, Cuadrado ML, Arias-Navalón JA, Hernández-Barrera V, Martín-Guerrero JD, Pellicer-Valero OJ, Arendt-Nielsen L. Prevalence and risk factors of musculoskeletal pain symptoms as long-term post-COVID sequelae in hospitalized COVID-19 survivors: a multicenter study. Pain. 2021;1:5–89. https://doi.org/10.1097/j.pain.0000000000002564.
Fernández-de-Las-Peñas C, Martín-Guerrero JD, Cancela-Cilleruelo I, Moro-López-Menchero P, Rodríguez-Jiménez J, Pellicer-Valero OJ. Trajectory curves of post-COVID anxiety/depressive symptoms and sleep quality in previously hospitalized COVID-19 survivors: the LONG-COVID-EXP-CM multicenter study. Psychol Med. 2022;10:1–2. https://doi.org/10.1017/S003329172200006X.
Bellan M, Baricich A, Patrucco F, Zeppegno P, Gramaglia C, Balbo PE, Carriero A, Amico CS, Avanzi GC, Barini M, Battaglia M. Long-term sequelae are highly prevalent one year after hospitalization for severe COVID-19. Sci Rep. 2021;11:1. https://doi.org/10.1038/s41598-021-01215-4.
Romero-Duarte Á, Rivera-Izquierdo M, de Alba IG, Pérez-Contreras M, Fernández-Martínez NF, Ruiz-Montero R, Serrano-Ortiz Á, González-Serna RO, Salcedo-Leal I, Jiménez-Mejías E, Cárdenas-Cruz A. Sequelae, persistent symptomatology and outcomes after COVID-19 hospitalization: the ANCOHVID multicentre 6-month follow-up study. BMC Med. 2021;19:1–3. https://doi.org/10.1186/s12916-021-02003-7.
Simani L, Ramezani M, Darazam IA, Sagharichi M, Aalipour MA, Ghorbani F, Pakdaman H. Prevalence and correlates of chronic fatigue syndrome and post-traumatic stress disorder after the outbreak of the COVID-19. J Neurovirol. 2021;27:154–9. https://doi.org/10.1007/s13365-021-00949-1.
Mei Q, Wang F, Yang Y, Hu G, Guo S, Zhang Q, Bryant A, Zhang L, Kurts C, Wei L, Yuan X. Health issues and immunological assessment related to Wuhan’s COVID-19 survivors: a multicenter follow-up study. Front Med. 2021;7:487. https://doi.org/10.3389/fmed.2021.617689.
Qu G, Zhen Q, Wang W, Fan S, Wu Q, Zhang C, Li B, Liu G, Yu Y, Li Y, Yong L. Health-related quality of life of COVID-19 patients after discharge: a multicenter follow-up study. J Clin Nurs. 2021;30:1742–50. https://doi.org/10.1111/jocn.15733.
Shang YF, Liu T, Yu JN, Xu XR, Zahid KR, Wei YC, Wang XH, Zhou FL. Half-year follow-up of patients recovering from severe COVID-19: analysis of symptoms and their risk factors. J Intern Med. 2021. https://doi.org/10.1111/joim.13284.
Suárez-Robles M, del Rosario Iguaran-Bermúdez M, García-Klepizg JL, Lorenzo-Villalba N, Méndez-Bailón M. Ninety days post-hospitalization evaluation of residual COVID-19 symptoms through a phone call check list. Pan Afr Med J. 2020;37:1–89. https://doi.org/10.11604/pamj.2020.37.289.27110.
Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, Luo J. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–32. https://doi.org/10.1016/S0140-6736(20)32656-8.
Tarsitani L, Vassalini P, Koukopoulos A, Borrazzo C, Alessi F, Di Nicolantonio C, Serra R, Alessandri F, Ceccarelli G, Mastroianni CM, d’Ettorre G. Post-traumatic stress disorder among COVID-19 survivors at 3-month follow-up after hospital discharge. J Gen Intern Med. 2021;36:1702–7. https://doi.org/10.1007/s11606-021-06731-7.
Froidure A, Mahsouli A, Liistro G, De Greef J, Belkhir L, Gérard L, Bertrand A, Koenig S, Pothen L, Yildiz H, Mwenge B. Integrative respiratory follow-up of severe COVID-19 reveals common functional and lung imaging sequelae. Respir Med. 2021;1: 106383. https://doi.org/10.1016/j.rmed.2021.106383.
Morin L, Savale L, Pham T, Colle R, Figueiredo S, Harrois A, Gasnier M, Lecoq AL, Meyrignac O, Noel N, Baudry E. Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA. 2021;325:1525–34. https://doi.org/10.1001/jama.2021.3331.
Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, Banerjee A. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 2021. https://doi.org/10.1136/bmj.n693.
Sykes DL, Holdsworth L, Jawad N, Gunasekera P, Morice AH, Crooks MG. Post-COVID-19 symptom burden: what is long-COVID and how should we manage it? Lung. 2021;199:113–9. https://doi.org/10.1007/s00408-021-00423-z.
Arnold DT, Hamilton FW, Milne A, Morley AJ, Viner J, Attwood M, Noel A, Gunning S, Hatrick J, Hamilton S, Elvers KT. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax. 2021;76:399–401. https://doi.org/10.1136/thoraxjnl-2020-216086.
Garrigues E, Janvier P, Kherabi Y, Le Bot A, Hamon A, Gouze H, Doucet L, Berkani S, Oliosi E, Mallart E, Corre F. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020;81:e4-6. https://doi.org/10.1016/j.jinf.2020.08.029.
Caruso D, Guido G, Zerunian M, Polidori T, Lucertini E, Pucciarelli F, Polici M, Rucci C, Bracci B, Nicolai M, Cremona A. Postacute sequelae of COVID-19 pneumonia: 6-month chest CT follow-up. Radiology. 2021;27: 210834. https://doi.org/10.1148/radiol.2021210834.
Castro V, Rosand J, Giacino J, McCoy T, Perlis RH. Case-control study of neuropsychiatric symptoms following COVID-19 hospitalization in 2 academic health systems. medRxiv. 2021. https://doi.org/10.1101/2021.07.09.21252353.
Darcis G, Bouquegneau A, Maes N, Thys M, Henket M, Labye F, Rousseau AF, Canivet P, Desir C, Calmes D, Schils R. Long-term clinical follow-up of patients suffering from moderate-to-severe COVID-19 infection: a monocentric prospective observational cohort study. Int J Infect Dis. 2021;1:209–16. https://doi.org/10.1016/j.ijid.2021.07.016.
González-Hermosillo JA, Martínez-López JP, Carrillo-Lampón SA, Ruiz-Ojeda D, Herrera-Ramírez S, Amezcua-Guerra LM, Martínez-Alvarado MD. Post-acute COVID-19 symptoms, a potential link with myalgic encephalomyelitis/chronic fatigue syndrome: a 6-month survey in a Mexican cohort. Brain Sci. 2021;11:760. https://doi.org/10.3390/brainsci11060760.
Gramaglia C, Gambaro E, Bellan M, Balbo PE, Baricich A, Sainaghi PP, Pirisi M, Baldon G, Battistini S, Binda V, Feggi A. Mid-term psychiatric outcomes of patients recovered from COVID-19 from an Italian cohort of hospitalized patients. Front Psychiatry. 2021. https://doi.org/10.3389/fpsyt.2021.667385.
Bozzetti S, Ferrari S, Zanzoni S, Alberti D, Braggio M, Carta S, Piraino F, Gabbiani D, Girelli D, Nocini R, Monaco S. Neurological symptoms and axonal damage in COVID-19 survivors: are there sequelae? Immunol Res. 2021;7:1–5. https://doi.org/10.1007/s12026-021-09220-5.
Maestre-Muñiz MM, Arias Á, Mata-Vázquez E, Martín-Toledano M, López-Larramona G, Ruiz-Chicote AM, Nieto-Sandoval B, Lucendo AJ. Long-term outcomes of patients with coronavirus disease 2019 at one year after hospital discharge. J Clin Med. 2021;10:2945. https://doi.org/10.3390/jcm10132945.
Vincent A, Beck K, Becker C, Zumbrunn S, Ramin-Wright M, Urben T, Quinto A, Schaefert R, Meinlschmidt G, Gaab J, Reinhardt T. Psychological burden in patients with COVID-19 and their relatives 90 days after hospitalization: a prospective observational cohort study. J Psychosom Res. 2021;1: 110526. https://doi.org/10.1016/j.jpsychores.2021.110526.
Sun LL, Wang J, Wang YS, Hu PF, Zhao ZQ, Chen W, Ning BF, Yin C, Hao YS, Wang Q, Wang C. Symptomatic features and prognosis of 932 hospitalized patients with coronavirus disease 2019 in Wuhan. J Dig Dis. 2021;22:271–81. https://doi.org/10.1111/1751-2980.12983.
Vlake JH, Wesselius S, van Genderen ME, van Bommel J, Boxma-de Klerk B, Wils EJ. Psychological distress and health-related quality of life in patients after hospitalization during the COVID-19 pandemic: a single-center, observational study. PLoS ONE. 2021;16: e0255774. https://doi.org/10.1371/journal.pone.0255774.
Huang L, Yao Q, Gu X, Wang Q, Ren L, Wang Y, Hu P, Guo L, Liu M, Xu J, Zhang X. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. The Lancet. 2021;398:747–58. https://doi.org/10.1016/S0140-6736(21)01755-4.
Li X, Shen C, Wang L, Majumder S, Zhang D, Deen MJ, Li Y, Qing L, Zhang Y, Chen C, Zou R. Pulmonary fibrosis and its related factors in discharged patients with new corona virus pneumonia: a cohort study. Respir Res. 2021;22:1. https://doi.org/10.1186/s12931-021-01798-6.
Sibila O, Albacar N, Perea L, Faner R, Torralba Y, Hernandez-Gonzalez F, Moisés J, Sanchez-Ruano N, Sequeira-Aymar E, Badia JR, Agusti A. Lung function sequelae in COVID-19 patients 3 months after hospital discharge. Arch Bronconeumol. 2021. https://doi.org/10.1016/j.arbres.2021.01.036.
Liu T, Wu D, Yan W, Wang X, Zhang X, Ma K, Chen H, Zeng Z, Qin Y, Wang H, Xing M. Twelve-month systemic consequences of COVID-19 in patients discharged from hospital: a prospective cohort study in Wuhan, China. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab703.
Lombardo MD, Foppiani A, Peretti GM, Mangiavini L, Battezzati A, Bertoli S, Martinelli Boneschi F, Zuccotti GV. Long term COVID-19 complications in inpatients and outpatients: a one-year follow up cohort study. SSRN 3814761. 2021. https://ssrn.com/abstract=3814761.
Maestrini V, Birtolo LI, Francone M, Galardo G, Galea N, Severino P, Alessandri F, Colaiacomo MC, Cundari G, Chimenti C, Lavalle C. Cardiac involvement in consecutive unselected hospitalized COVID-19 population: in-hospital evaluation and one-year follow-up. Int J Cardiol. 2021;15:235–42. https://doi.org/10.1016/j.ijcard.2021.06.056.
Sigfrid L, Drake TM, Pauley E, Jesudason EC, Olliaro P, Lim WS, Gillesen A, Berry C, Lowe DJ, McPeake J, Lone N. Long Covid in adults discharged from UK hospitals after Covid-19: a prospective, multicentre cohort study using the ISARIC WHO clinical characterisation protocol. medRxiv. 2021. https://doi.org/10.1101/2021.03.18.21253888.
Ahmed GK, Khedr EM, Hamad DA, Meshref TS, Hashem MM, Aly MM. Long term impact of COVID-19 infection on sleep and mental health: a cross-sectional study. Psychiatry Res. 2021;1: 114243. https://doi.org/10.1016/j.psychres.2021.114243.
Anjana NK, Annie TT, Siba S, Meenu MS, Chintha S, Anish TS. Manifestations and risk factors of post COVID syndrome among COVID-19 patients presented with minimal symptoms—a study from Kerala, India. J Fam Med Prim Care. 2021;10:4023–9. https://doi.org/10.4103/jfmpc.jfmpc_851_21.
Bai F, Tomasoni D, Falcinella C, Barbanotti D, Castoldi R, Mulè G, Augello M, Mondatore D, Allegrini M, Cona A, Tesoro D. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. 2022;28:611-e9. https://doi.org/10.1016/j.cmi.2021.11.002.
Chen X, Li Y, Shao TR, Yang LL, Li SJ, Wang XJ, Li A, Wu YY, Liu XF, Liu CM, Liu YH. Some characteristics of clinical sequelae of COVID-19 survivors from Wuhan, China: a multi-center longitudinal study. Influenza Other Respir Viruses. 2022;16:395–401. https://doi.org/10.1111/irv.12943.
Damiano RF, Caruso MJ, Cincoto AV, de Almeida Rocca CC, de Pádua SA, Bacchi P, Guedes BF, Brunoni AR, Pan PM, Nitrini R, Beach S. Post-COVID-19 psychiatric and cognitive morbidity: preliminary findings from a Brazilian cohort study. Gen Hosp Psychiatry. 2022. https://doi.org/10.1016/j.genhosppsych.2022.01.002.
Philippine EL, Tardivon C, Martin-Blondel G, Isnard M, Le Turnier P, Le Marechal M, Cabié A, Launay O, Tattevin P, Senneville E, Ansart S. Severity of self-reported symptoms and psychological burden 6-months after hospital admission for COVID-19: a prospective cohort study. Int J Infect Dis. 2021;1:247–53. https://doi.org/10.1016/j.ijid.2021.09.011.
Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, Elneima O, Docherty AB, Lone NI, Leavy OC, Daines L. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med. 2021;9:1275–87. https://doi.org/10.1016/S2213-2600(21)00383-0.
Gamberini L, Mazzoli CA, Prediletto I, Sintonen H, Scaramuzzo G, Allegri D, Colombo D, Tonetti T, Zani G, Capozzi C, Dalpiaz G. Health-related quality of life profiles, trajectories, persistent symptoms and pulmonary function one year after ICU discharge in invasively ventilated COVID-19 patients, a prospective follow-up study. Respir Med. 2021;189: 106665. https://doi.org/10.1016/j.rmed.2021.106665.
García-Abellán J, Padilla S, Fernández-González M, García JA, Agulló V, Andreo M, Ruiz S, Galiana A, Gutiérrez F, Masiá M. Antibody response to SARS-CoV-2 is associated with long-term clinical outcome in patients with COVID-19: a longitudinal study. J Clin Immunol. 2021;41:1490–501. https://doi.org/10.1007/s10875-021-01083-7.
Ghosn J, Piroth L, Epaulard O, Le Turnier P, Mentré F, Bachelet D, Laouénan C. Persistent COVID-19 symptoms are highly prevalent 6 months after hospitalization: results from a large prospective cohort. Clin Microbiol Infect. 2021;27:1041-e1. https://doi.org/10.1016/j.cmi.2021.03.012.
Hodgson CL, Higgins AM, Bailey MJ, Mather AM, Beach L, Bellomo R, Bissett B, Boden IJ, Bradley S, Burrell A, Cooper DJ. The impact of COVID-19 critical illness on new disability, functional outcomes and return to work at 6 months: a prospective cohort study. Crit Care. 2021;25:1–2. https://doi.org/10.1186/s13054-021-03794-0.
Horwitz LI, Garry K, Prete AM, Sharma S, Mendoza F, Kahan T, Karpel H, Duan E, Hochman KA, Weerahandi H. Six-month outcomes in patients hospitalized with severe COVID-19. J Gen Intern Med. 2021;36:3772–7. https://doi.org/10.1007/s11606-021-07032-9.
Huang L, Xu X, Zhang L, Zheng D, Liu Y, Feng B, Hu J, Lin Q, Xi X, Wang Q, Lin M. Post-traumatic stress disorder symptoms and quality of life of COVID-19 survivors at 6-month follow-up: a cross-sectional observational study. Front Psychiatry. 2021. https://doi.org/10.3389/fpsyt.2021.782478.
Huarcaya-Victoria J, Barreto J, Aire L, Podestá A, Caqui M, Guija-Igreda R, Castillo C, Alarcon-Ruiz CA. Mental health in COVID-2019 survivors from a general hospital in Peru: sociodemographic, clinical, and inflammatory variable associations. Int J Ment Heal Addict. 2021;28:1–22. https://doi.org/10.1007/s11469-021-00659-z.
Karaarslan F, Güneri FD, Kardeş S. Long COVID: rheumatologic/musculoskeletal symptoms in hospitalized COVID-19 survivors at 3 and 6 months. Clin Rheumatol. 2022;41:289–96. https://doi.org/10.1007/s10067-021-05942-x.
Boglione L, Meli G, Poletti F, Rostagno R, Moglia R, Cantone M, Esposito M, Scianguetta C, Domenicale B, Di Pasquale F, Borrè S. Risk factors and incidence of long-COVID syndrome in hospitalized patients: does remdesivir have a protective effect? QJM Int J Med. 2021;114:865–71. https://doi.org/10.1093/qjmed/hcab297.
Chand S, Kapoor S, Naqvi A, Thakkar J, Fazzari MJ, Orsi D, Dieiev V, Lewandowski DC, Dicpinigaitis PV. Long-term follow up of renal and other acute organ failure in survivors of critical illness due to covid-19. J Intensive Care Med. 2021. https://doi.org/10.1177/08850666211062582.
Kumar J, Makheja K, Rahul FN, Kumar S, Kumar M, Chand M, Kammawal Y, Khalid D, Jahangir M, Bachani P. Long-term neurological impact of COVID-19. Cureus. 2021. https://doi.org/10.7759/cureus.18131.
Mei Z, Wu X, Zhang X, Zheng X, Li W, Fan R, Yu H, Zhang S, Gu Y, Wang X, Xia Y. The occurrence and risk factors associated with post-traumatic stress disorder among discharged COVID-19 patients in Tianjin, China. Brain Behav. 2022;5:1–2492. https://doi.org/10.1002/brb3.2492.
Nesan GS, Keerthana D, Yamini R, Jain T, Kumar D, Eashwer A, Maiya GR. 3-Month symptom-based ambidirectional follow-up study among recovered COVID-19 patients from a tertiary care hospital using telehealth in Chennai, India. Inquiry J Health Care Org Provis Financ. 2021. https://doi.org/10.1177/00469580211060165.
Ong SW, Fong SW, Young BE, Chan YH, Lee B, Amrun SN, Chee RS, Yeo NK, Tambyah P, Pada S, Tan SY. Persistent symptoms and association with inflammatory cytokine signatures in recovered coronavirus disease 2019 patients. In: Open forum infectious diseases, vol 8, no 6, p. ofab156. Oxford: Oxford University Press; 2021
Rass V, Beer R, Schiefecker AJ, Kofler M, Lindner A, Mahlknecht P, Heim B, Limmert V, Sahanic S, Pizzini A, Sonnweber T. Neurological outcome and quality of life 3 months after COVID-19: a prospective observational cohort study. Eur J Neurol. 2021;28:3348–59. https://doi.org/10.1111/ene.14803.
Righi E, Mirandola M, Mazzaferri F, Dossi G, Razzaboni E, Zaffagnini A, Ivaldi F, Visentin A, Lambertenghi L, Arena C, Micheletto C. Determinants of persistence of symptoms and impact on physical and mental wellbeing in long COVID: a prospective cohort study. J Infect. 2022. https://doi.org/10.1016/j.jinf.2022.02.003.
Rivera-Izquierdo M, Láinez-Ramos-Bossini AJ, de Alba IG, Ortiz-González-Serna R, Serrano-Ortiz Á, Fernández-Martínez NF, Ruiz-Montero R, Cervilla JA. Long COVID 12 months after discharge: persistent symptoms in patients hospitalised due to COVID-19 and patients hospitalised due to other causes—a multicentre cohort study. BMC Med. 2022;20:1. https://doi.org/10.1186/s12916-022-02292-6.
Sibila O, Perea L, Albacar N, Moisés J, Cruz T, Mendoza N, Solarat B, Lledó G, Espinosa G, Barberà JA, Badia JR. Elevated plasma levels of epithelial and endothelial cell markers in COVID-19 survivors with reduced lung diffusing capacity six months after hospital discharge. Respir Res. 2022;23:1. https://doi.org/10.1186/s12931-022-01955-5.
Staudt A, Jörres RA, Hinterberger T, Lehnen N, Loew T, Budweiser S. Associations of Post-Acute COVID syndrome with physiological and clinical measures 10 months after hospitalization in patients of the first wave. Eur J Intern Med. 2022;1:50–60. https://doi.org/10.1016/j.ejim.2021.10.031.
Tessitore E, Handgraaf S, Poncet A, Achard M, Höfer S, Carballo S, Marti C, Follonier C, Girardin F, Mach F, Carballo D. Symptoms and quality of life at 1-year follow up of patients discharged after an acute COVID-19 episode. Swiss Med Wkly. 2021. https://doi.org/10.4414/smw.2021.w30093.
Tleyjeh IM, Saddik B, Ramakrishnan RK, AlSwaidan N, AlAnazi A, Alhazmi D, Aloufi A, AlSumait F, Berbari EF, Halwani R. Long term predictors of breathlessness, exercise intolerance, chronic fatigue and well-being in hospitalized patients with COVID-19: a cohort study with 4 months median follow-up. J Infect Public Health. 2022;15:21–8. https://doi.org/10.1016/j.jiph.2021.11.016.
Torres-Ruiz J, Lomelín-Gascón J, Lira-Luna J, Pérez-Fragoso A, Tapia-Conyer R, Nuñez-Aguirre M, Alcalá-Carmona B, Absalón-Aguilar A, Maravillas-Montero JL, Mejía-Domínguez NR, Núñez-Álvarez C. FANSY POSTCOV: a composite clinical immunological predictive index for post-COVID-19 syndrome unveils distinctive features in a cohort study of mild to critical patients. Clin Transl Med. 2021;11: e623. https://doi.org/10.1002/ctm2.623.
Vejen M, Hansen EF, Al-Jarah BN, Jensen C, Thaning P, Jeschke KN, Ulrik CS. Hospital admission for COVID-19 pneumonitis–long-term impairment in quality of life and lung function. Eur Clin Respir J. 2022;9:2024735. https://doi.org/10.1080/20018525.2021.2024735.
Wang B, Yang X, Fu L, Hu Y, Luo D, Xiao X, Ju N, Zheng W, Xu H, Fang Y, Chan PS. Post-traumatic stress disorder symptoms in COVID-19 survivors 6 months after hospital discharge: an application of the conservation of resource theory. Front Psychiatry. 2021. https://doi.org/10.3389/fpsyt.2021.773106.
Wong-Chew RM, Rodríguez Cabrera EX, Rodríguez Valdez CA, Lomelin-Gascon J, Morales-Juárez L, de la Cerda ML, Villa-Romero AR, Arce Fernández S, Serratos Fernandez M, Bello HH, Castañeda LM. Symptom cluster analysis of long COVID-19 in patients discharged from the temporary COVID-19 hospital in Mexico City. Ther Adv Infect Dis. 2022;9:20499361211069264. https://doi.org/10.1177/20499361211069264.
Zhang X, Wang F, Shen Y, Zhang X, Cen Y, Wang B, Zhao S, Zhou Y, Hu B, Wang M, Liu Y. Symptoms and health outcomes among survivors of COVID-19 infection 1 year after discharge from hospitals in Wuhan, China. JAMA Netw Open. 2021;4:e2127403. https://doi.org/10.1001/jamanetworkopen.2021.27403.
Zhou F, Tao M, Shang L, Liu Y, Pan G, Jin Y, Wang L, Hu S, Li J, Zhang M, Fu Y. Assessment of sequelae of COVID-19 nearly 1 year after diagnosis. Front Med. 2021. https://doi.org/10.3389/fmed.2021.717194.
Zuschlag D, Grandt D, Custodis F, Braun C, Häuser W. Spontaneously reported persistent symptoms related to coronavirus disease 2019 one year after hospital discharge. Der Schmerz. 2022;25:1–9. https://doi.org/10.1007/s00482-022-00626-0.
Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–34. https://doi.org/10.1016/S1473-3099(20)30086-4.
Mo X, Jian W, Su Z, Chen M, Peng H, Peng P, Lei C, Chen R, Zhong N, Li S. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur Respir J. 2020. https://doi.org/10.1183/13993003.01217-2020.
Venkataraman T, Frieman MB. The role of epidermal growth factor receptor (EGFR) signaling in SARS coronavirus-induced pulmonary fibrosis. Antiviral Res. 2017;1:142–50. https://doi.org/10.1016/j.antiviral.2017.03.022.
Frija-Masson J, Debray MP, Gilbert M, Lescure FX, Travert F, Borie R, Khalil A, Crestani B, d’Ortho MP, Bancal C. Functional characteristics of patients with SARS-CoV-2 pneumonia at 30 days post-infection. Eur Respir J. 2020. https://doi.org/10.1183/13993003.01754-2020.
Torres-Castro R, Vasconcello-Castillo L, Alsina-Restoy X, Solis-Navarro L, Burgos F, Puppo H, Vilaró J. Respiratory function in patients post-infection by COVID-19: a systematic review and meta-analysis. Pulmonology. 2020. https://doi.org/10.1016/j.pulmoe.2020.10.013.
McGroder CF, Zhang D, Choudhury MA, Salvatore MM, D’Souza BM, Hoffman EA, Wei Y, Baldwin MR, Garcia CK. Pulmonary fibrosis 4 months after COVID-19 is associated with severity of illness and blood leucocyte telomere length. Thorax. 2021. https://doi.org/10.1136/thoraxjnl-2021-217031.
Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, Shi H, Zhou M. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020;296:E55-64. https://doi.org/10.1148/radiol.2020200843.
Barisione E, Grillo F, Ball L, Bianchi R, Grosso M, Morbini P, Pelosi P, Patroniti NA, De Lucia A, Orengo G, Gratarola A. Fibrotic progression and radiologic correlation in matched lung samples from COVID-19 post-mortems. Virchows Arch. 2021;478:471–85. https://doi.org/10.1007/s00428-020-02934-1.
Huang W, Wu Q, Chen Z, Xiong Z, Wang K, Tian J, Zhang S. The potential indicators for pulmonary fibrosis in survivors of severe COVID-19. J Infect. 2021;82:e5-7. https://doi.org/10.1016/j.jinf.2020.09.027.
Yao XH, Li TY, He ZC, Ping YF, Liu HW, Yu SC, Mou HM, Wang LH, Zhang HR, Fu WJ, Luo T. A pathological report of three COVID-19 cases by minimally invasive autopsies. Zhonghua bing li xue za zhi Chin J Pathol. 2020;49:E009. https://doi.org/10.3760/cma.j.cn112151-20200312-00193.
Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis. 2021;53:737–54. https://doi.org/10.1080/23744235.2021.1924397.
Phetsouphanh C, Darley DR, Wilson DB, Howe A, Munier C, Patel SK, Juno JA, Burrell LM, Kent SJ, Dore GJ, Kelleher AD. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol. 2022;13:1–7. https://doi.org/10.1038/s41590-021-01113-x.
Zhao YM, Shang YM, Song WB, Li QQ, Xie H, Xu QF, Jia JL, Li LM, Mao HL, Zhou XM, Luo H. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine. 2020;1: 100463. https://doi.org/10.1016/j.eclinm.2020.100463.
González J, Benítez ID, Carmona P, Santisteve S, Monge A, Moncusí-Moix A, Gort-Paniello C, Pinilla L, Carratalá A, Zuil M, Ferrer R. Pulmonary function and radiologic features in survivors of critical COVID-19: a 3-month prospective cohort. Chest. 2021;160:187–98. https://doi.org/10.1016/j.chest.2021.02.062.
Frija-Masson J, Debray MP, Boussouar S, Khalil A, Bancal C, Motiejunaite J, Galarza-Jimenez MA, Benzaquen H, Penaud D, Laveneziana P, Malrin R. Residual ground glass opacities three months after covid-19 pneumonia correlate to alteration of respiratory function: the post Covid M3 study. Respir Med. 2021;1: 106435. https://doi.org/10.1016/j.rmed.2021.106435.
Maccio U, Zinkernagel AS, Schuepbach R, Probst-Mueller E, Frontzek K, Brugger SD, Hofmaenner DA, Moch H, Varga Z. Long-term persisting SARS-CoV-2 RNA and pathological findings: lessons learnt from a series of 35 COVID-19 autopsies. Front Med. 2022. https://doi.org/10.3389/fmed.2022.778489.
Haffke M, Freitag H, Rudolf G, Seifert M, Doehner W, Scherbakov N, Hanitsch L, Wittke K, Bauer S, Konietschke F, Paul F. Endothelial dysfunction and altered endothelial biomarkers in patients with post-COVID-19 syndrome and chronic fatigue syndrome (ME/CFS). J Transl Med. 2022;20:1–1. https://doi.org/10.1186/s12967-022-03346-2.
Vianello A, Guarnieri G, Braccioni F, Lococo S, Molena B, Cecchetto A, Giraudo C, De Marchi LB, Caminati M, Senna G. The pathogenesis, epidemiology and biomarkers of susceptibility of pulmonary fibrosis in COVID-19 survivors. Clin Chem Lab Med (CCLM). 2022;60:307–16. https://doi.org/10.1515/cclm-2021-1021.
Fernández-de-Las-Peñas C, Ryan-Murua P, Rodríguez-Jiménez J, Palacios-Ceña M, Arendt-Nielsen L, Torres-Macho J. Serological biomarkers at hospital admission are not related to long-term post-COVID fatigue and dyspnea in COVID-19 survivors. Respiration. 2022;5:1–8. https://doi.org/10.1159/000524042.
Cheung OY, Chan JW, Ng CK, Koo CK. The spectrum of pathological changes in severe acute respiratory syndrome (SARS). Histopathology. 2004;45:119–24. https://doi.org/10.1111/j.1365-2559.2004.01926.x.
Helding L, Carroll TL, Nix J, Johns MM, LeBorgne WD, Meyer D. COVID-19 after effects: concerns for singers. J Voice. 2020. https://doi.org/10.1016/j.jvoice.2020.07.032.
Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract. 2020;1: 101166. https://doi.org/10.1016/j.ctcp.2020.101166.
Ali RM, Ghonimy MB. Post-COVID-19 pneumonia lung fibrosis: a worrisome sequelae in surviving patients. Egypt J Radiol Nucl Med. 2021;52:1–8. https://doi.org/10.1186/s43055-021-00484-3.
Stam H, Stucki G, Bickenbach J. Covid-19 and post intensive care syndrome: a call for action. J Rehabil Med. 2020. https://doi.org/10.2340/16501977-2677.
Funke-Chambour M, Bridevaux PO, Clarenbach CF, Soccal PM, Nicod LP, von Garnier C. Swiss recommendations for the follow-up and treatment of pulmonary long COVID. Respiration. 2021;100:826–41. https://doi.org/10.1159/000517255.
British Thoracic Society. Guidance on respiratory follow up of patients with a clinical radiological diagnosis of COVID-19 pneumonia. British Thoracic Society. 2020. https://www.brit-thoracic.org.uk.
Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1265–73. https://doi.org/10.1001/jamacardio.2020.3557.
Mitrani RD, Dabas N, Goldberger JJ. COVID-19 cardiac injury: implications for long-term surveillance and outcomes in survivors. Heart Rhythm. 2020;17:1984–90. https://doi.org/10.1016/j.hrthm.2020.06.026.
Gąsior M, Jaroszewicz J, Wita K, Cieśla D, Hudzik B. High post-discharge mortality in hospitalized COVID-19 patients with cardiovascular comorbidities. Pol Arch Intern Med. 2021. https://doi.org/10.20452/pamw.16026.
Lavery AM, Preston LE, Ko JY, Chevinsky JR, DeSisto CL, Pennington AF, Kompaniyets L, Datta SD, Click ES, Golden T, Goodman AB. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission—United States, March–August 2020. Morbid Mortal Wkly Rep. 2020;69:1695. https://doi.org/10.15585/mmwr.mm6945e2.
Chopra V, Flanders SA, O’Malley M, Malani AN, Prescott HC. Sixty-day outcomes among patients hospitalized with COVID-19. Ann Intern Med. 2021;174:576–8. https://doi.org/10.7326/M20-5661.
O’Sullivan JS, Lyne A, Vaughan CJ. COVID-19-induced postural orthostatic tachycardia syndrome treated with ivabradine. BMJ Case Rep CP. 2021;14: e243585. https://doi.org/10.1136/bcr-2021-243585.
Blitshteyn S, Whitelaw S. Postural orthostatic tachycardia syndrome (POTS) and other autonomic disorders after COVID-19 infection: a case series of 20 patients. Immunol Res. 2021;69:205–11. https://doi.org/10.1007/s12026-021-09191-7.
Goldstein DS. The possible association between COVID-19 and postural tachycardia syndrome. Heart Rhythm. 2021. https://doi.org/10.1016/j.hrthm.2020.12.007.
Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, Zandi MS, Lewis G, David AS. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611–27. https://doi.org/10.1016/S2215-0366(20)30203-0.
Sun B, Tang N, Peluso MJ, Iyer NS, Torres L, Donatelli JL, Munter SE, Nixon CC, Rutishauser RL, Rodriguez-Barraquer I, Greenhouse B. Characterization and biomarker analyses of post-COVID-19 complications and neurological manifestations. Cells. 2021;10:386. https://doi.org/10.3390/cells10020386.
Olanipekun T, Abe T, Effoe V, Westney G, Snyder R. Incidence and severity of depression among recovered African Americans with COVID-19-associated respiratory failure. J Racial Ethn Health Disparities. 2021;6:1–6. https://doi.org/10.1007/s40615-021-01034-3.
Cai X, Hu X, Ekumi IO, Wang J, An Y, Li Z, Yuan B. Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am J Geriatr Psychiatry. 2020;28:1030–9. https://doi.org/10.1016/j.jagp.2020.07.003.
Miners S, Kehoe PG, Love S. Cognitive impact of COVID-19: looking beyond the short term. Alzheimers Res Ther. 2020;12:1–6. https://doi.org/10.1186/s13195-020-00744-w.
Coolen T, Lolli V, Sadeghi N, Rovai A, Trotta N, Taccone FS, Creteur J, Henrard S, Goffard JC, Dewitte O, Naeije G. Early postmortem brain MRI findings in COVID-19 non-survivors. Neurology. 2020;95:e2016–27. https://doi.org/10.1212/WNL.0000000000010116.
Stefano GB. Historical insight into infections and disorders associated with neurological and psychiatric sequelae similar to long COVID. Med Sci Monit Int Med J Exp Clin Res. 2021;27:e931447-1.
Sollini M, Morbelli S, Ciccarelli M, Cecconi M, Aghemo A, Morelli P, Chiola S, Gelardi F, Chiti A. Long COVID hallmarks on [18F] FDG-PET/CT: a case-control study. Eur J Nucl Med Mol Imaging. 2021;7:1–1. https://doi.org/10.1007/s00259-021-05294-3.
Radnis C, Qiu S, Jhaveri M, Da Silva I, Szewka A, Koffman L. Radiographic and clinical neurologic manifestations of COVID-19 related hypoxemia. J Neurol Sci. 2020;15: 117119. https://doi.org/10.1016/j.jns.2020.117119.
Lee MH, Perl DP, Nair G, Li W, Maric D, Murray H, Dodd SJ, Koretsky AP, Watts JA, Cheung V, Masliah E. Microvascular injury in the brains of patients with Covid-19. N Engl J Med. 2021;384:481–3. https://doi.org/10.1056/NEJMc2033369.
Metlay JP, Fine MJ, Schulz R, Marrie TJ, Coley CM, Kapoor WN, Singer DE. Measuring symptomatic and functional recovery in patients with community-acquired pneumonia. J Gen Intern Med. 1997;12:423–30. https://doi.org/10.1046/j.1525-1497.1997.00074.x.
Morley JE, Kalantar-Zadeh K, Anker SD. COVID-19: a major cause of cachexia and sarcopenia? J Cachexia Sarcopenia Muscle. 2020;11:863–5. https://doi.org/10.1002/jcsm.12589.
Patel KP, Patel PA, Vunnam RR, Hewlett AT, Jain R, Jing R, Vunnam SR. Gastrointestinal, hepatobiliary, and pancreatic manifestations of COVID-19. J Clin Virol. 2020;1: 104386. https://doi.org/10.1016/j.jcv.2020.104386.
Iacobucci G. Long covid: damage to multiple organs presents in young, low risk patients. BMJ Br Med J. 2020. https://doi.org/10.1136/bmj.m4470.
Zhong P, Xu J, Yang D, Shen Y, Wang L, Feng Y, Du C, Song Y, Wu C, Hu X, Sun Y. COVID-19-associated gastrointestinal and liver injury: clinical features and potential mechanisms. Signal Transduct Target Ther. 2020;5:1–8. https://doi.org/10.1038/s41392-020-00373-7.
An YW, Song S, Li WX, Chen YX, Hu XP, Zhao J, Li ZW, Jiang GY, Wang C, Wang JC, Yuan B. Liver function recovery of COVID-19 patients after discharge, a follow-up study. Int J Med Sci. 2021;18:176. https://doi.org/10.7150/ijms.50691.
Marjot T, Moon AM, Cook JA, Abd-Elsalam S, Aloman C, Armstrong MJ, Pose E, Brenner EJ, Cargill T, Catana MA, Dhanasekaran R. Outcomes following SARS-CoV-2 infection in patients with chronic liver disease: an international registry study. J Hepatol. 2021;74:567–77. https://doi.org/10.1016/j.jhep.2020.09.024.
Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, Villapol S. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021. https://doi.org/10.2139/ssrn.3769978.
Mieczkowska K, Deutsch A, Borok J, Guzman AK, Fruchter R, Patel P, Wind O, McLellan BN, Mann RE, Halverstam CP. Telogen effluvium: a sequela of COVID-19. Int J Dermatol. 2021. https://doi.org/10.1111/ijd.15313.
Chee YJ, Ng SJ, Yeoh E. Diabetic ketoacidosis precipitated by covid-19 in a patient with newly diagnosed diabetes mellitus. Diabetes Res Clin Pract. 2020;164:108166. https://doi.org/10.1016/j.diabres.2020.108166.
Suwanwongse K, Shabarek N. Newly diagnosed diabetes mellitus, DKA, and COVID-19: causality or coincidence? A report of three cases. J Med Virol. 2021;93:1150–3. https://doi.org/10.1002/jmv.26339.
Papachristou S, Stamatiou I, Stoian AP, Papanas N. New-onset diabetes in COVID-19: time to frame its fearful symmetry. Diabetes Ther. 2021;12:461–4. https://doi.org/10.1007/s13300-020-00988-7.
Di Filippo L, De Lorenzo R, D’Amico M, Sofia V, Roveri L, Mele R, Saibene A, Rovere-Querini P, Conte C. COVID-19 is associated with clinically significant weight loss and risk of malnutrition, independent of hospitalisation: a post-hoc analysis of a prospective cohort study. Clin Nutr. 2021;40:2420–6. https://doi.org/10.1016/j.clnu.2020.10.043.
Sansone A, Mollaioli D, Ciocca G, Limoncin E, Colonnello E, Vena W, Jannini EA. Addressing male sexual and reproductive health in the wake of COVID-19 outbreak. J Endocrinol Investig. 2021;44:223–31. https://doi.org/10.1007/s40618-020-01350-1.
Mumm JN, Osterman A, Ruzicka M, Stihl C, Vilsmaier T, Munker D, Khatamzas E, Giessen-Jung C, Stief C, Staehler M, Rodler S. Urinary frequency as a possibly overlooked symptom in COVID-19 patients: does SARS-CoV-2 cause viral cystitis? Eur Urol. 2020;78:624–8. https://doi.org/10.1016/j.eururo.2020.05.013.
Silva CC, Bichara CN, Carneiro FR, Palacios VR, Van den Berg AV, Quaresma JA, Falcão LF. Muscle dysfunction in the long coronavirus disease 2019 syndrome: pathogenesis and clinical approach. Rev Med Virol. 2019. https://doi.org/10.1002/rmv.2355.
Wang L, Yang N, Yang J, Zhao S, Su C. A review: the manifestations, mechanisms, and treatments of musculoskeletal pain in patients with COVID-19. Front Pain Res. 2022. https://doi.org/10.3389/fpain.2022.826160.
Liu J, Zhang S, Wu Z, Shang Y, Dong X, Li G, Zhang L, Chen Y, Ye X, Du H, Liu Y. Clinical outcomes of COVID-19 in Wuhan, China: a large cohort study. Ann Intensive Care. 2020;10:1–21. https://doi.org/10.1186/s13613-020-00706-3.
Cheng D, Calderwood C, Skyllberg E, Ainley A. Clinical characteristics and outcomes of adult patients admitted with COVID-19 in East London: a retrospective cohort analysis. BMJ Open Respir Res. 2021;8: e000813. https://doi.org/10.1136/bmjresp-2020-000813.
Fernández-de-las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Florencio LL, Cuadrado ML, Plaza-Manzano G, Navarro-Santana M. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: a systematic review and meta-analysis. Eur J Intern Med. 2021. https://doi.org/10.1016/j.ejim.2021.06.009.
Canas LS, Sudre CH, Pujol JC, Polidori L, Murray B, Molteni E, Graham MS, Klaser K, Antonelli M, Berry S, Davies R. Early detection of COVID-19 in the UK using self-reported symptoms: a large-scale, prospective, epidemiological surveillance study. Lancet Digit Health. 2021;3:e587–98. https://doi.org/10.1016/S2589-7500(21)00131-X.
Mackey K, Ayers CK, Kondo KK. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. 2021;174:362–73. https://doi.org/10.7326/M20-6306.
Wu BB, Gu DZ, Yu JN, Yang J, Shen WQ. Association between ABO blood groups and COVID-19 infection, severity and demise: a systematic review and meta-analysis. Infect Genet Evol. 2020. https://doi.org/10.1016/j.meegid.2020.104485.
Sivan M, Halpin S, Gee J. Assessing long-term rehabilitation needs in COVID-19 survivors using a telephone screening tool (C19-YRS tool). Adv Clin Neurosci Rehabil. 2020;19:14–7. https://doi.org/10.47795/NELE5960.
National Health Service United Kingdom. Newcastle post-COVID syndrome follow up screening questionnaire. National Health Service United Kingdom. 2021. https://www.rdash.nhs.uk/wp-content/uploads/2021/03/Newcastle-Post-Covid-Screening-Questionnaire.pdf.
Yan Z, Yang M, Lai CL. Long covid-19 syndrome: a comprehensive review of its effect on various organ systems and recommendation on rehabilitation plans. Biomedicines. 2021;9:966. https://doi.org/10.3390/biomedicines9080966.
Sheehy LM. Considerations for postacute rehabilitation for survivors of COVID-19. JMIR Public Health Surveill. 2020;6: e19462. https://doi.org/10.2196/19462.
Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Krznarić Ž, Nitzan D, Pirlich M, Singer P. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Liječnički vjesnik. 2020;142:75–84. https://doi.org/10.26800/LV-142-3-4-13.
Yan ZP, Yang M, Lai CL. COVID-19 vaccines: a review of the safety and efficacy of current clinical trials. Pharmaceuticals. 2021;14:406. https://doi.org/10.3390/ph14050406.
Yan Z, Yang M, Lai CL. COVID-19 vaccinations: a comprehensive review of their safety and efficacy in special populations. Vaccines. 2021;9:1097. https://doi.org/10.3390/vaccines9101097.
Acknowledgements
This work was supported by AIR@InnoHK administered by Innovation and Technology Commission.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval is not required for this systematic review and meta-analysis as only secondary analysis of data already available in scientific databases will be conducted.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, T., Yan, M.Z., Li, X. et al. Sequelae of COVID-19 among previously hospitalized patients up to 1 year after discharge: a systematic review and meta-analysis. Infection 50, 1067–1109 (2022). https://doi.org/10.1007/s15010-022-01862-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-022-01862-3