Abstract
The aim of this study was to compare the clinic outcomes between new single-port laparoscopic appendectomy (NSLA) and conventional three-port laparoscopic appendectomy (CTLA) for patients with acute appendicitis. Patients who were diagnosed with acute appendicitis and underwent appendectomy were retrospectively collected from a single clinical center from September 2021 to June 2023. Baseline characteristics, surgical information, and postoperative information were compared between the NSLA group and the CTLA group. Univariate and multivariate logistic regression analyses were used to find out the predictors of overall complications. A total of 296 patients were enrolled from a single clinical medical center. There were 146 (49.3%) males and 150 (50.7%) females. There were 54 (18.2%) patients in the NSLA group and 242 (81.8%) patients in the CTLA group. After data analysis, we found the patients in the NSLA group had a shorter postoperative hospital stay (P < 0.01) than the CTLA group. The other outcomes including intraoperative blood loss (P = 0.167), operation time (P = 0.282), nature of the appendix (P = 0.971), and overall complications (P = 0.543) were not statistically different. After univariate and multivariate logistic regression analysis, we found that age (P = 0.018, OR = 1.039, 95% CI = 1.007–1.072), neutrophil percentage (P = 0.018, OR = 1.070, 95% CI = 1.011–1.132), and fever (P = 0.019, OR = 6.112, 95% CI = 1.340–27.886) were the predictors of overall complications. However, the surgical procedure (NSLA versus CTLA) was not a predictor of overall complications (P = 0.376, OR = 1.964, 95% CI = 0.440–8.768). Compared with CTLA, there was no significant increase in postoperative overall complications with NSLA, making it a safe and feasible new surgical procedure. More studies are needed to evaluate the long-term results.



Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Ferris M, Quan S, Kaplan BS, Molodecky N, Ball CG, Chernoff GW et al (2017) The global incidence of appendicitis: a systematic review of population-based studies. Ann Surg 266(2):237–241. https://doi.org/10.1097/SLA.0000000000002188
Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A et al (2020) Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 15(1):27. https://doi.org/10.1186/s13017-020-00306-3
Wu J, Li M, Liu Q, Xu X, Lu X, Ma G et al (2021) Current practice of acute appendicitis diagnosis and management in China (PANDA-C): a national cross-sectional survey. Surg Infect 22(9):973–982. https://doi.org/10.1089/sur.2021.061
O’Leary DP, Walsh SM, Bolger J, Baban C, Humphreys H, O’Grady S et al (2021) A randomized clinical trial evaluating the efficacy and quality of life of antibiotic-only treatment of acute uncomplicated appendicitis: results of the COMMA trial. Ann Surg 274(2):240–247. https://doi.org/10.1097/SLA.0000000000004785
Semm K (1983) Endoscopic appendectomy. Endoscopy 15(2):59–64. https://doi.org/10.1055/s-2007-1021466
Towfigh S, Chen F, Mason R, Katkhouda N, Chan L, Berne T (2006) Laparoscopic appendectomy significantly reduces length of stay for perforated appendicitis. Surg Endosc 20(3):495–499. https://doi.org/10.1007/s00464-005-0249-8
Golub R, Siddiqui F, Pohl D (1998) Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg 186(5):545–553. https://doi.org/10.1016/s1072-7515(98)00080-5
Giday SA, Kantsevoy SV, Kalloo AN (2006) Principle and history of natural orifice translumenal endoscopic surgery (NOTES). Minim Invasive Ther Allied Technol 15(6):373–377. https://doi.org/10.1080/13645700601038010
Buess GF (2008) Natural orifice transluminal endoscopic surgery (NOTES). Minim Invasive Ther Allied Technol 17(6):329–330. https://doi.org/10.1080/13645700802528082
Arezzo A, Repici A, Kirschniak A, Schurr MO, Ho CN, Morino M (2008) New developments for endoscopic hollow organ closure in prospective of NOTES. Minim Invasive Ther Allied Technol 17(6):355–360. https://doi.org/10.1080/13645700802538628
Chow A, Purkayastha S, Aziz O, Paraskeva P (2010) Single-incision laparoscopic surgery for cholecystectomy: an evolving technique. Surg Endosc 24(3):709–714. https://doi.org/10.1007/s00464-009-0655-4
Poon JT, Cheung CW, Fan JK, Lo OS, Law WL (2012) Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc 26(10):2729–2734. https://doi.org/10.1007/s00464-012-2262-z
Jeong BC, Park YH, Han DH, Kim HH (2009) Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study. J Endourol 23(12):1957–1960. https://doi.org/10.1089/end.2009.0404
Page AJ, Pollock JD, Perez S, Davis SS, Lin E, Sweeney JF (2010) Laparoscopic versus open appendectomy: an analysis of outcomes in 17,199 patients using ACS/NSQIP. J Gastrointest Surg 14(12):1955–1962. https://doi.org/10.1007/s11605-010-1300-1
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Chen Y, Guo S, Liu Y, Yuan J, Fan Z (2022) Single-port laparoscopic appendectomy using a needle-type grasping forceps compared with conventional three-port laparoscopic appendectomy for patients with acute uncomplicated appendicitis: a single-center retrospective study. J Int Med Res 50(8):3000605221119647. https://doi.org/10.1177/03000605221119647
Podda M, Gerardi C, Cillara N, Fearnhead N, Gomes CA, Birindelli A et al (2019) Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg 270(6):1028–1040. https://doi.org/10.1097/SLA.0000000000003225
Minneci PC, Hade EM, Metzger GA, Saito JM, Mak GZ, Deans KJ, Midwest Pediatric Surgery Consortium (2021) Association of initial treatment with antibiotics vs surgery with treatment success and disability in subgroups of children with uncomplicated appendicitis. JAMA 325(24):2502–2504. https://doi.org/10.1001/jama.2021.6710
Moris D, Paulson EK, Pappas TN (2021) Diagnosis and management of acute appendicitis in adults: a review. JAMA 326(22):2299–2311. https://doi.org/10.1001/jama.2021.20502
Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M et al (2018) Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA 320(12):1259–1265. https://doi.org/10.1001/jama.2018.13201. (Erratum in: JAMA. 2018;320(16):1711)
Talan DA, Di Saverio S (2021) Treatment of acute uncomplicated appendicitis. N Engl J Med 385(12):1116–1123. https://doi.org/10.1056/NEJMcp2107675
Köhler F, Hendricks A, Kastner C, Müller S, Boerner K, Wagner JC et al (2021) Laparoscopic appendectomy versus antibiotic treatment for acute appendicitis-a systematic review. Int J Colorectal Dis 36(10):2283–2286. https://doi.org/10.1007/s00384-021-03927-5
Khan MN, Fayyad T, Cecil TD, Moran BJ (2007) Laparoscopic versus open appendectomy: the risk of postoperative infectious complications. JSLS 11(3):363–367
Vettoretto N, Agresta F (2011) A brief review of laparoscopic appendectomy: the issues and the evidence. Tech Coloproctol 15(1):1–6. https://doi.org/10.1007/s10151-010-0656-2
Qiu J, Yuan H, Chen S, He Z, Wu H (2014) Single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy: evidence from randomized controlled trials and nonrandomized comparative studies. Surg Laparosc Endosc Percutan Tech 24(1):12–21. https://doi.org/10.1097/SLE.0b013e3182937da4
Lee WS, Choi ST, Lee JN, Kim KK, Park YH, Lee WK et al (2013) Single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy: a prospective randomized controlled study. Ann Surg 257(2):214–218. https://doi.org/10.1097/SLA.0b013e318273bde4
Teoh AY, Chiu PW, Wong TC, Wong SK, Lai PB, Ng EK (2011) A case-controlled comparison of single-site access versus conventional three-port laparoscopic appendectomy. Surg Endosc 25(5):1415–1419. https://doi.org/10.1007/s00464-010-1406-2
Esparaz JR, Jeziorczak PM, Mowrer AR, Chakraborty SR, Nierstedt RT, Zumpf KB et al (2019) Adopting single-incision laparoscopic appendectomy in children: is it safe during the learning curve? J Laparoendosc Adv Surg Tech A 29(10):1306–1310. https://doi.org/10.1089/lap.2019.0112
Assali S, Eapen S, Carman T, Horattas S, Daigle CR, Paranjape C (2018) Single-port laparoscopic appendectomy: beyond the learning curve: a retrospective comparison with multi-port laparoscopic appendectomy. Surg Laparosc Endosc Percutan Tech 28(5):291–294. https://doi.org/10.1097/SLE.0000000000000546
Kang BM, Choi SI, Kim BS, Lee SH (2018) Single-port laparoscopic surgery in uncomplicated acute appendicitis: a randomized controlled trial. Surg Endosc 32(7):3131–3137. https://doi.org/10.1007/s00464-018-6028-0
Kim Y, Lee W (2016) The learning curve of single-port laparoscopic appendectomy performed by emergent operation. World J Emerg Surg 5(11):39. https://doi.org/10.1186/s13017-016-0096-z
Isik A, Demiryilmaz I, Yilmaz I et al (2016) Effectiveness of manual knotting at laparoscopic appendectomy. Gazi Med J 27:19–20
Acknowledgements
The authors are grateful to all the colleagues who helped in the preparation of this article.
Author information
Authors and Affiliations
Contributions
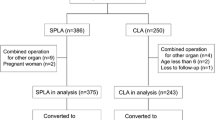
Data extraction, FL and Z-WL; quality assessments, DP, WZ, and C-YW; data analysis, X-RL, Z-WL, and QL; writing the main manuscript text, FL; writing—review and editing, X-RL, Z-WL, X-YL, X-PS, L-SL, YT, and QL. DP prepared Figs. 1, 2, 3. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and informed consent
The study was approved by the ethics committee of our institution (The First Affiliated Hospital of Chongqing Medical University, K2023-339). This study was conducted in accordance with the World Medical Association Declaration of Helsinki as well.
Consent for publication
Not applicable.
Research involving human participants and/or animals
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, F., Lv, Q., Wang, CY. et al. Single-port laparoscopic appendectomy using new surgical procedure versus conventional three-port laparoscopic appendectomy. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01775-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01775-w