Abstract
Introduction
Studies show that the COVID-19 pandemic disproportionately affected people with diabetes and those from disadvantaged backgrounds. During the first 6 months of the UK lockdown, > 6.6 M glycated haemoglobin (HbA1c) tests were missed. We now report variability in the recovery of HbA1c testing, and its association with diabetes control and demographic characteristics.
Methods
In a service evaluation, we examined HbA1c testing across ten UK sites (representing 9.9% of England’s population) from January 2019 to December 2021. We compared monthly requests from April 2020 to those in the equivalent 2019 months. We examined effects of (i) HbA1c level, (ii) between-practice variability, and (iii) practice demographics.
Results
In April 2020, monthly requests dropped to 7.9–18.1% of 2019 volumes. By July 2020, testing had recovered to 61.7–86.9% of 2019 levels. During April–June 2020, we observed a 5.1-fold variation in the reduction of HbA1c testing between general practices (12.4–63.8% of 2019 levels). There was evidence of limited prioritization of testing for patients with HbA1c > 86 mmol/mol during April–June 2020 (4.6% of total tests vs. 2.6% during 2019). Testing in areas with the highest social disadvantage was lower during the first lockdown (April–June 2020; trend test p < 0.001) and two subsequent periods (July–September and October–December 2020; both p < 0.001). By February 2021, testing in the highest deprivation group had a cumulative fall in testing of 34.9% of 2019 levels versus 24.6% in those in the lowest group.
Conclusion
Our findings highlight that the pandemic response had a major impact on diabetes monitoring and screening. Despite limited test prioritization in the > 86 mmol/mol group, this failed to acknowledge that those in the 59–86 mmol/mol group require consistent monitoring to achieve the best outcomes. Our findings provide additional evidence that those from poorer backgrounds were disproportionately disadvantaged. Healthcare services should redress this health inequality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The COVID-19 pandemic disproportionately affected people with diabetes and those from disadvantaged backgrounds |
During the first months of the pandemic, testing for glycated haemoglobin (HbA1c) fell markedly as the response to the pandemic disrupted healthcare services globally |
During key pandemic phases, we examined (i) whether testing in those with poorest control was prioritized during the lockdowns, (ii) the variability between general practices in testing patterns, and (iii) links to practice demographic characteristics, including social deprivation status |
What was learned from the study? |
We showed that (i) there was limited prioritization of HbA1c testing in those with a HbA1c of > 86 mmol/mol, (ii) there was a fivefold variation in testing between general practices during the early part of the pandemic, and (iii) testing in areas of highest social disadvantage recovered more slowly than in those with the least deprivation |
What were the study outcomes/conclusions? |
There is significant variability in response to and recovery from the UK lockdowns, particularly with respect to diabetes control and social disadvantage |
Addressing health inequality represents a major challenge, particularly during resource-poor scenarios |
Introduction
Over the past two and a half years, the global response to the SARS-CoV-2 virus has disrupted healthcare systems across the world [1, 2]. Services for the diagnosis and management of people with diabetes were similarly disrupted [3,4,5]. Accordingly, routine blood testing, a cornerstone of diabetes diagnosis and management, was significantly affected, partly because of the perceived risk phlebotomy posed in facilitating transmission of the virus, but also because of public concerns about attending for tests [6, 7].
As reported by ourselves [8] and others [9], the frequency of testing, for both diagnosis of diabetes and its monitoring, was greatly reduced in the spring and summer of 2020, with significant implications for the health of people with diabetes and also in relation to screening for diabetes. Specifically, we described that during the first 6 months of the UK COVID-19-associated lockdown, > 6.6 million HbA1c tests were missed or delayed, including 1.41 million missed or delayed in people with diabetes (0.51 million in those with sub-optimal control).
The implications of these missed tests for people with diabetes are considerable. We previously showed a link between HbA1c testing frequency and diabetes control expressed as both change in HbA1c [10] and likelihood of achieving target [11]. More recently, we reported that regularity of HbA1c testing, independent of testing frequency, is associated with a more favourable glycaemic outcome at all levels of previous HbA1c up to 86 mmol/mol [12]. Thus, disruption of testing has a potential major impact on future glycaemic control for many individuals, as well as on the identification of people with incident diabetes.
A key question is: to what extent did HbA1c testing volume recover in the latter part of 2020 and through 2021, particularly following the periods of most intense restrictions (referred to as ‘lockdowns’)? Here, we look at the degree of recovery of HbA1c testing across ten UK sites following the two main UK lockdown periods. In particular, we examined (i) whether testing in those with poorest control was prioritized during the lockdowns, (ii) the variability between general practices in testing patterns, and (iii) links to practice demographic characteristics, including social deprivation status.
Methods
Using information from Laboratory Information and Management Systems, we extracted data on all HbA1c requests received between 1 January 2019 and 31 December 2021 by ten UK Clinical Biochemistry Departments: University Hospitals of North Midlands NHS Trust (UHNM); St Helens and Knowsley Teaching Hospitals NHS Trust (STHK); Northern Care Alliance NHS Foundation Trust—Salford Royal Hospital (NCA-S); Northern Care Alliance NHS Foundation Trust—Oldham Hospital (NCA-O); Cambridge University Hospitals NHS Foundation Trust (CUH); Warrington & Halton Hospitals NHS Trust (WHH); Mid-Cheshire NHS Foundation Trust (MCFT); Wirral University Teaching Hospital NHS Foundation Trust (WUTH); Countess of Chester Hospital NHS Foundation Trust (COCH); and Liverpool Clinical Laboratories (LCL) (5,576,685 tests in 2,815,765 patients). The sample included people with both type 1 diabetes (T1DM) and type 2 diabetes (T2DM), as well as those where HbA1c was used as a screening or diagnostic test.
These sites serve an estimated population of 6,095,068. Assuming the population of England to be 61,573,400 (at December 2021; [13]), this equates to 9.9% of the English population.
As this work represented an evaluation of the respective clinical biochemistry services, ethical committee approval was not required. Permission to access and use the information from the Laboratory Information and Management Systems was obtained from the relevant laboratory leads at each of the sites. All extracted data were fully anonymized before processing and analysis.
Practice-Level Data
Practice-level data (practice list size, age profile, Index of Multiple Deprivation [IMD] score, diabetes prevalence) were obtained from NHS Digital [14]. Age was assessed as the proportion of patients aged over 65 years. IMD score for each general practice was derived according to a report, The English Indices of Deprivation 2019 [15], based on the score allocated to the general practice postcode area. All variables were categorized by decile cutoffs into ten ranked groups of the distribution (henceforth referred to as ‘groups’) for the practices covered by the ten sites.
HbA1c Test Trends Over Time
For each site, we examined the change in test volume over the study period, expressed as a percentage of the mean monthly volume for 2019. This was investigated in the context of the different levels of restrictions in place in England over the course of the study period (vide infra) and the impact of the UK shortage of blood collection tubes, including the EDTA-containing tubes used for HbA1c analysis (September–October 2021) [16].
Using these data, we also explored whether people with higher HbA1c values were prioritized during key points within the pandemic. To this end, we categorized patients into those whose HbA1c prior to the pandemic start was ≤ 58 mmol/mol, 59–86 mmol/mol or > 86 mmol/mol, and examined the ratios of the volumes of tests in these categories to total test numbers over time.
Categorization of Pandemic-Associated Restrictions
The impacts of the lockdowns and the recovery of UK HbA1c testing following these periods were assessed by evaluating testing levels during key periods:
-
Lock 1: first full UK lockdown (April–June 2020)
-
Rec 1: phased easing of restrictions (‘recovery’) following Lock 1 (July–September 2020)
-
Tiers: partial reintroduction of restrictions interspersed with partial lockdowns and the use of the ‘tier’ system of region-specific restrictions (October–December 2020)
-
Lock 2: second full UK lockdown (January–February 2021)
-
Rec 2: phased easing of restrictions following Lock 2 (March–June 2021)
-
R Lift: most restrictions lifted (July–August 2021 and November–December 2021).
We separately also considered the impact of the blood tube shortage (BTS; September–October 2021).
Covid or blood tube shortage impact was assessed as the deviation of testing volumes compared with those observed during the equivalent period in 2019. Similarly, the two periods of pandemic recovery were assessed as the extent to which testing returned to its pre-pandemic (2019-equivalent) volumes.
Statistical Analysis
Analysis of the link between HbA1c test recovery and deprivation score was performed by (i) calculating the recovery score [(test volume during recovery period)/(test volume during the equivalent period in 2019)] and (ii) examining the trend in mean recovery score across the deprivation score groups using the Jonckheere–Terpstra nonparametric test for trends [17]; in view of the number of comparisons performed, statistical significance was set at p ≤ 0.01 (two-tailed) in order to control the type 1 error rate. A nonparametric test was used in view of the marked positive skew in some variables. Practices with < 100 tests in either the recovery periods or equivalent periods during 2019 were excluded from the analysis, as practices with very small testing volumes may reflect changes in service configuration and unduly affect the recovery scores. All statistical analyses were performed using Stata (version 17; College Station, Texas).
Results
Study Sample
The ten sites comprised a range of laboratory sizes (ranging from those in small district general hospitals to those in large university teaching hospitals). These laboratories served 745 general practices (11.5% of the practices in England), covering 433,069 people with diabetes (9.9% of the UK diabetes population). The diabetes prevalence across the ten sites (7.11%) was similar to that across England (7.14%). The 745 practices were spread across the IMD groups; however, while groups 1–9 each contained 7.1–12.1% of the practices, 23.1% of the practices were in areas in the tenth IMD group (highest social deprivation areas).
HbA1c Test Volume Trends Over Time
Figure 1(i) shows the monthly trends in HbA1c testing volumes between January 2019 and December 2021 across the ten sites as a percentage of the mean 2019 monthly volumes for each site. This illustrates that monthly patterns of testing were similar across the sites during 2019 and early 2020, followed by an 81.9–92.1% fall in April 2020 across all sites. By July 2020, the sites had recovered to 61.7–86.9% of the 2019 levels, though there was noticeably more variation between sites from this point onwards.
There was a second drop around January 2021, coinciding with the second lockdown, and a third dip in October 2021 linked to the national shortage of the required blood specimen tubes. While testing recovered in the intervening periods, it did not achieve the expected normal levels, which were predicted to be around 108% in 2020 and 117% in 2021, based on the general trend in increasing HbA1c testing (8% p.a.) during the previous decade.
Prioritization of Testing
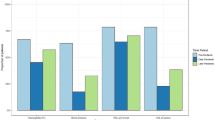
To assess whether people with high HbA1c values were prioritized during lockdowns, we examined test volumes in three categories: ≤ 58 mmol/mol, 59–86 mmol/mol or > 86 mmol/mol. Figure 1(ii) shows test volumes over time in each of these groups. This showed that there was some evidence that testing in those with HbA1c values > 86 mmol/mol recovered more quickly after the first lockdown than that in the other two groups.
When expressed as a proportion of total tests, there appeared to be some degree of prioritization of testing those with HbA1c values of > 86 mmol/mol during the first UK lockdown (Lock 1: April–June 2020) and, to a lesser degree, during the second full lockdown (Lock 2: January–February 2021) (Fig. 2).
Change in HbA1c test volumes over time as a ratio of total tests: (i) tests with HbA1c ≤ 58 mmol/mol, (ii) tests with HbA1c 59–86 mmol/mol, (iii) tests with HbA1c > 86 mmol/mol, expressed as a percentage of the mean monthly test ratio for 2019. Note that the vertical axis in chart (i) has a non-zero origin
We also noted that there was significant variability between sites in the prioritization in relation to HbA1c, with some sites showing little evidence of prioritization (UHNM) while others showed more marked changes in practice (LCL, WUTH, NCA-S, WHH) (data not shown).
Variability in the Initial Impact of the Pandemic by General Practice
To assess the degree of variability in initial impact of the pandemic between general practices, we examined the mean monthly test volumes for the period April–June 2020 compared to the same period in 2019 for each general practice. Figure 3 shows the ski-slope plot of test ratios in testing by general practice and demonstrates that there was a 5.1-fold variation in reduction in HbA1c testing between the second and 98th percentiles across the 734 practices with at least 100 tests during April–June 2019 (from 12.4% to 63.8% of 2019 levels).
Factors Associated with Variability in Recovery of HbA1c Testing
We examined readily-available practice-level data on diabetes prevalence, list size and patients’ ages, each categorized into ten groups based on deciles, as described in the “Methods” section, to explore the factors linked to the variability in recovery of HbA1c testing. Table 1 shows the results of the Jonckheere–Terpstra non-parametric trend test, while supplemental Fig. S1 shows line diagrams to illustrate the direction and pattern of the associations. Practice list size did not show a significant association with test volume during any of the pandemic periods. Percentage aged over 65 demonstrated a significant association during Rec 1 and Lock 2 (an inverse relationship in the latter). We also observed an inverse association between HbA1c test volumes and diabetes prevalence during Tiers, and during the two consecutive periods: Rec 2 and R Lift.
The most notable associations with HbA1c test volumes were observed with IMD; increasing deprivation score was significantly associated with lower testing volumes during each of the three initial periods (Lock 1, Rec 1 and Tiers), demonstrating a statistically significant association of slower test recovery with greater average social disadvantage at a general practice level. This was also evident during the Rec 2 and R Lift periods, though there was some evidence of a recovery in those in the highest social disadvantage group (deprivation score group 10) in the Rec 2 period (Fig. S1).
We did not identify any significant associations between HbA1c test volumes and any of the practice parameters during the blood tube shortage (BTS period).
HbA1c Test Volume Trends Over Time by Deprivation Score
To further examine the link between HbA1c testing and deprivation score, we examined month-by-month test volumes by IMD group in those practices with at least 100 tests during each of the 3 years of data collection. As before, these were expressed as a percentage of the mean monthly volume for each group for the period January–December 2019.
Figure 4 shows that, overall, those areas with the lowest deprivation (particularly those in IMD groups 1–3) recovered more quickly during the period April 2020–December 2020. Across the whole pandemic period (April 2020–December 2021), those in areas with IMD groups 5–10 appeared to recover the slowest (Table S1).
We also examined the cumulative impact of reduction in HbA1c testing by IMD group by examining the cumulative deficit in HbA1c testing compared with 2019 levels. Figure 5 shows that, by February 2021, testing fell by 24.6% in those practices in areas with the lowest deprivation (IMD group 1) compared to 34.9% in areas with the highest deprivation (IMD group 10): an additional 10.3% cumulative loss of testing. Other groups demonstrated an intermediate cumulative impact. Data from the remainder of 2021 showed that there was no evidence of a ‘catch up’ in any of the groups, except perhaps a small recovery in group 10 in July–August 2021.
Cumulative percentage change in HbA1c test volumes for IMD groups 1 to 10 relative to their respective mean monthly figures for 2019. Values for IMD groups 1 and 10 at February 2021 and December 2021 are labelled. IMD group 1 represents the category with the lowest social disadvantage. IMD groups 1 and 10 are shown by thicker lines
Discussion
Our findings reinforce the fact that the UK response to the COVID-19 pandemic continued to have a major impact on diabetes management at least until December 2021 in our centres, with some yet to return to pre-pandemic levels of monitoring. This ongoing impact appeared to be most significant in areas of greatest social disadvantage, thereby adding to the increasing body of evidence showing that those from poorer backgrounds continue to be disproportionately disadvantaged in the context of SARS-CoV-2. Given the importance of regular testing in people with diabetes [12], there is an onus on healthcare services to address this inequality.
HbA1c Test Volume Trends Over Time
We showed that, across all ten centres, monthly HbA1c requests dropped by 81.9–92.1% in April 2020 compared with the mean monthly 2019 request numbers. This replicates our previous findings [8], those from the US (a reduction of 66% in HbA1c testing during the first 8 weeks of the pandemic) [18], Israel (a reduction in HbA1c of ~ 55% during April 2020 [19] and Spain (a reduction of 52% during March–June 2020 in people with a HbA1c of < 48 mmol/mol) [20]. It is also consistent with other UK findings by Carr et al. [9], which showed a similar magnitude of reduction in HbA1c testing in April 2020. Similarly, they showed that testing rates return to around 80–85% of pre-pandemic levels during the period up to December 2020 (similar to the 73.8–87.6% from our data by December 2020), while Palanca et al. [20] showed that testing in Spain returned to normal levels during July–September 2020. Our longer data collection period allowed us to detect a second dip in testing during the UK’s second lockdown at the beginning of 2021, though the impact on testing at this point was less severe, suggesting that some adaptation to facilitate ongoing testing was occurring. This is in keeping with data from Spain showing that testing fell less dramatically during their second partial lockdown (October–December 2020; 85% of 2019 levels) [20].
From our data, during the post-lockdown 1 period (July 2020–December 2021), the degree of recovery to pre-pandemic levels showed greater variability between centres in relation to volume of HbA1c testing than was the case at the start of the COVID-19 pandemic. This variability was also reflected in the fivefold between-practice variation in reduction in HbA1c testing during the first lockdown (April–June 2020). These findings are consistent with variation between practices in laboratory testing that we and others have previously observed both in HbA1c testing and in other areas where regular testing is required [21,22,23]. A scoping review by Elwenspoek et al. highlighted that unwarranted variation in test ordering among general practices may lead to patient harm and increased health care costs [24]. During the pandemic, consistent monitoring would appear particularly important for people with sub-optimally controlled diabetes, as they had poorer outcomes in the event of SARS-CoV-2 infection [25].
Blood Collection Tube Shortage
We observed a dip in testing during September–October 2021, which coincided with the UK-specific effect of the global shortage of the potassium-EDTA blood collection tubes. We noted wide variability between sites in the impact of this shortage. This may have reflected the different manufacturers supplying tubes to particular laboratories, as some suppliers were disproportionately affected. The shortage led to NHS England (and other equivalent bodies in the UK devolved nations) issuing recommendations on how to reduce tube usage [26]. This included an emphasis on utilizing minimum retest intervals for tests including HbA1c and, in the case of diabetes routine reviews, to ‘Consider postponing the blood test elements of the review if the patient’s history suggests they are low risk of harm in the next three months’ [27].
Prioritization of Testing
Our data suggest some prioritization of testing in people with HbA1c values of > 86 mmol/mol during the first UK lockdown (at the expense of those with values of < 59 mmol/mol), but less so during subsequent restrictions, including the second major lockdown during winter 2020–2021. The degree and timing of prioritization during lockdown 1 appeared to vary between sites, suggesting that prioritization protocols, if used, were variably implemented.
Given the worldwide disruption of healthcare services during the pandemic, including those for diabetes [3,4,5,6,7], prioritization of services during the initial stages of the pandemic became a necessary adaptation. Seidu et al. conducted a survey of 975 healthcare professionals in primary care and noted that most (63.9%) had altered their approach to choosing which people to recall for a diabetes annual review [28]. Of these, 82.4% said that they implemented some form of clinical risk prioritization. Of those who did not implementation prioritization protocols, around two-thirds said they were able to provide a full service, while 15% said that they did not have the capacity to implement a prioritization protocol. During the early stages of the pandemic, the Primary Care Diabetes Society and the Association of British Clinical Diabetologists published a guide for the prioritization of diabetes services during the pandemic using a traffic light (red/amber/green) system [29, 30]. They classified those with a HbA1c level of > 86 mmol/mol or those with no HbA1c for > 24 months as red and therefore warranted being seen within 3 months. Those with HbA1c values of 59–86 mmol/mol or no result for 18–24 months were classified as amber and recommended to be seen within 6 months. They recognized the importance of HbA1c and suggested that initial prioritization by HbA1c was a good starting point.
This prioritization strategy, along with the blood tube shortage recommendations, may be appropriate in some cases, and we would agree that those with a HbA1c in the > 86 mmol/mol category require closer monitoring. However, perhaps counter-intuitively, we have shown that it is the 59–86 mmol/mol group that is most likely to benefit from more consistent HbA1c testing in terms of subsequent lowering of HbA1c [12].
HbA1c Testing and Practice Characteristics
Our data demonstrated that HbA1c testing during the pandemic was linked to practice-level characteristics; particularly the proportion aged over 65 years, diabetes prevalence and social disadvantage. The association with age over 65 years during the Rec 1 period may reflect a surge in attendance for tests following the first UK lockdown (during which testing was most severely affected), perhaps reflecting the importance of testing in the older, generally more vulnerable age groups in which diabetes control would be particularly important, given the link between diabetes and poorer covid-associated clinical outcomes [25, 31]. There was also an association between age and HbA1c testing during the second lockdown (Lock 2), though in this case it appeared that those practices with a lower proportion aged over 65 years performed more testing than other groups. This may indicate that there was a greater reluctance to attend for testing in the older age groups during this period when case numbers were higher. Palanca et al. observed that HbA1c testing decreased more markedly in the > 65-year-old age group during their initial lockdown, but not during subsequent periods [20].
Compared with the pattern seen with age, the significant associations between HbA1c testing and diabetes prevalence across the pandemic phases appeared to be more consistent and cover a number of consecutive periods. We observed similar inverse associations across a number of the pandemic phases where restrictions were less severe (Tiers, Rec 2 and R Lift), with recovery being slower in areas with higher diabetes prevalence. This may reflect concerns about covid-associated risks for diabetes patients [25, 31], and perhaps a focus on those at highest risk in these areas, in line with guidance on prioritization from professional bodies [29, 30].
HbA1c Testing and Social Disadvantage
We have shown that general practices serving areas with the highest levels of deprivation appeared to recover from the initial pandemic-linked reduction in HbA1c testing more slowly than those with the lowest levels of deprivation. While there appeared to be evidence of a limited recovery of testing in the second half of 2021 for those in the highest deprivation group, over the duration of the study period, test volumes in the least deprived areas recovered better than those in IMD groups 5–9. Our data on cumulative deficit in HbA1c testing showed that, by December 2021, there was no evidence of additional testing to make up for those tests lost during the preceding 21 months. If our data are reflected nationally, many thousands of patients missed important and sometimes essential diabetes tests, with inevitable consequences for health outcomes [8, 10,11,12].
It is now well established that those people in society who are at greatest social disadvantage are more likely to succumb to the adverse effects of a COVID-19 infection in relation to complications, hospital admission and mortality [32, 33], with ethnic differences accounted for at least in part by differences in socio-demographic situation. Furthermore, it has been known for decades that people in the higher social deprivation groups, with or without diabetes, have a higher standardized mortality rate [34, 35] and poorer clinical outcomes [36,37,38]. If replicated across the UK, our findings that those in the highest social deprivation groups were disproportionality affected by the failure of HbA1c monitoring during the pandemic would highlight the urgent need for improvements in health inequalities across the UK. Furthermore, the design of future research studies needs to address the importance of social determinants of health in people with diabetes [39].
Implications
While we have not looked at health outcomes here, it is well established that less regular frequent testing of HbA1c is associated with a rise in HbA1c over time [10, 11], and that a higher HbA1c is associated with greater microvascular and macrovascular complication rates and a higher mortality date in both T1DM [40] and T2DM [41]. Thus, any change in the frequency of HbA1c testing may result in more (in both number and severity) adverse health outcomes in our centres in subsequent years. In this context, the findings of Valabhji et al., which support the view that the reduction in diabetes care service provision was linked to increased rates of non-COVID-related mortality in people with diabetes [42], illustrate the vital importance of continuing engagement between healthcare services and people with diabetes, which not only raises their pre-COVID-19-associated risk but increases the probability of poor outcomes in the event of SARS-CoV-2 infection [25, 31]. This is particularly true for those experiencing social disadvantage.
The fact that, even by the period May–December 2021, HbA1c monitoring had not recovered to pre-pandemic levels has not, as far as we are aware, been reported elsewhere. The reasons for this are complex and likely include factors such as (i) delays in returning to the annual review timetable [28], (ii) suspension of the Quality Outcome Framework (QOF) [43] payment scheme (which incentivizes general practices to bring diabetes patients in annually for routine tests), and (iii) reticence on the part of individuals with diabetes to attend their general practices for routine investigations.
Strengths and Limitations
We were able to access all HbA1c test data from ten large biochemistry laboratories covering a total population base of 6.1 million people (9.9% of the population of England). This large cohort comprised a range of geographical and demographic areas and was broadly representative of the UK as a whole in terms of diabetes prevalence and spread of IMD score. Furthermore, the use of laboratory data allowed the assessment of longitudinal HbA1c testing from both primary and secondary care.
We acknowledge that the use of laboratory data has its disadvantages. For example, we were not able to extract clinical data, such as type of diabetes or medications used.
We also recognize that HbA1c alone is not the only marker of glucose dysregulation—blood glucose measurement is also important in this regard, and routine laboratory databases do not include home glucose monitoring data. Hence, our figures may underestimate the magnitude of the impact of the pandemic on diabetes detection and perhaps overestimate the impact on monitoring in our centres. However, HbA1c is the better measure of long-term diabetes control, and testing rates have been shown to be linked to clinical outcomes [10,11,12].
We used a measure of deprivation at general practice level as data at a more granular level (e.g. based on patient postcode) was not available. We accept that IMD based on general practice is a relatively crude measure of social disadvantage. However, given the limited spread of social disadvantage in many general practice lists, we felt that it was a reasonable measure to apply.
Conclusion
The limited prioritization of testing of those with poorer diabetes control during the first UK lockdown indicates that there is a need for improved targeting of support during resource-poor scenarios. This needs to be nationally driven to reduce the observed practice-level variability and enhance the robustness of the system.
Our findings also reinforce that the COVID-19 pandemic continues to have a major impact on diabetes management, with some centres having yet to return to pre-pandemic levels by the end of 2021. This continuing impact of pandemic measures on HbA1c testing appears most significant in areas of greatest social deprivation, thereby adding to the increasing body of evidence showing that those from poorer backgrounds continue to be disproportionately disadvantaged in the context of SARS-CoV-2 and its consequences. There is therefore a responsibility on healthcare services to implement urgent measures to redress this imbalance.
Although this service evaluation focuses just on the participating centres, we hope that it has highlighted the continuing impact of the COVID-19 pandemic on the day-to-day management of those people with diabetes, particularly those in a more socially disadvantaged situation, and that this information may be of relevance to other clinical centres in the UK. This will have consequences for their future health that need to be taken account of by health service planners and by government in the coming months and years.
References
Rawaf S, Allen LN, Stigler FL, Kringos D, Quezada Yamamoto H, van Weel C. Global forum on universal health coverage and primary health care. Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. 2020;26(1):129–33.
Krist AH, DeVoe JE, Cheng A, Ehrlich T, Jones SM. Redesigning primary care to address the COVID-19 pandemic in the midst of the pandemic. Ann Fam Med. 2020;18:349–54.
Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14(5):965–7.
Williams R, Jenkins DA, Ashcroft DM, Brown B, Campbell S, Carr MJ, Cheraghi-Sohi S, Kapur N, Thomas O, Webb RT, Peek N. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. Lancet Public Health. 2020;5(10):e543–50.
Rachamin Y, Senn O, Streit S, Dubois J, Deml MJ, Jungo KT. Impact of the COVID-19 pandemic on the intensity of health services use in general practice: a retrospective cohort study. Int J Public Health. 2021;66: 635508.
Levene LS, Seidu S, Greenhalgh T, Khunti K. Pandemic threatens primary care for long term conditions. BMJ. 2020;371: m3793.
Ludwig L, Scheyer N, Remen T, Guerci B. The impact of COVID-19 lockdown on metabolic control and access to healthcare in people with diabetes: the CONFI-DIAB cross-sectional study. Diabetes Ther. 2021;12(8):2207–21.
Holland D, Heald AH, Stedman M, Hanna F, Wu P, Duff C, Green L, Robinson S, Halsall I, Gaskell N, Pemberton J, Bloor C, Fryer AA. Assessment of the effect of the COVID-19 pandemic on UK HbA1c testing: implications for diabetes management and diagnosis. J Clin Pathol. 2021;13: 207776.
Carr MJ, Wright AK, Leelarathna L, Thabit H, Milne N, Kanumilli N, Ashcroft DM, Rutter MK. Impact of COVID-19 restrictions on diabetes health checks and prescribing for people with type 2 diabetes: a UK-wide cohort study involving 618 161 people in primary care. BMJ Qual Saf. 2021;12: 013613.
Driskell OJ, Holland D, Waldron JL, Ford C, Scargill JJ, Heald A, Tran M, Hanna FW, Jones PW, Pemberton RJ, Fryer AA. Reduced testing frequency for glycated hemoglobin, HbA1c, is associated with deteriorating diabetes control. Diabetes Care. 2014;37(10):2731–7.
Duff CJ, Solis-Trapala I, Driskell OJ, Holland D, Wright H, Waldron JL, Ford C, Scargill JJ, Tran M, Hanna FWF, Pemberton RJ, Heald A, Fryer AA. The frequency of testing for glycated haemoglobin, HbA1c, is linked to the probability of achieving target levels in patients with suboptimally controlled diabetes mellitus. Clin Chem Lab Med. 2018;57(2):296–304.
Fryer AA, Holland D, Stedman M, Duff CJ, Green L, Scargill J, Hanna FWF, Wu P, Pemberton RJ, Bloor C, Heald AH. Variability in test interval is linked to glycated haemoglobin (HbA1c) trajectory over time. J Diabetes Res. 2022;2022(16):7093707.
NHS Digital. Patients registered at a GP practice. September 2022. https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice/september-2022 Accessed 9 November 2022
NHS Digital. Patients registered at a GP practice. https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice. Accessed 9 November 2022
Ministry of Housing, Communities and Local Government. The English indices of deprivation 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/833951/IoD2019_Technical_Report.pdf
Rimmer A. What has caused the NHS blood tube shortage, and how is it affecting doctors and patients? BMJ. 2021;374: n2174.
Jonckheere AR. A distribution-free k-sample test against ordered alternatives. Biometrika. 1954;41(1/2):133–45.
Fragala MS, Kaufman HW, Meigs JB, Niles JK, McPhaul MJ. Consequences of the COVID-19 pandemic: reduced hemoglobin A1c diabetes monitoring. Popul Health Manag. 2021;24(1):8–9.
Rose AJ, Ein Mor E, Krieger M, Ben-Yehuda A, Cohen AD, Matz E, Bar-Ratson E, Bareket R, Paltiel O, Calderon-Margalit R. Israeli COVID lockdowns mildly reduced overall use of preventive health services, but exacerbated some disparities. Int J Qual Health Care. 2022;34(3):71.
Palanca A, Quinones-Torrelo C, Girbés J, Real JT, Ampudia-Blasco FJ. Impact of COVID-19 lockdown on diabetes management and follow-up in a broad population in Spain. Eur J Clin Invest. 2022;52(6): e13771.
Driskell OJ, Holland D, Hanna FW, Jones PW, Pemberton RJ, Tran M, Fryer AA. Inappropriate requesting of glycated hemoglobin (Hb A1c) is widespread: assessment of prevalence, impact of national guidance, and practice-to-practice variability. Clin Chem. 2012;58(5):906–15.
Scargill JJ, Livingston M, Holland D, Duff CJ, Fryer AA, Heald AH. Monitoring thyroid function in patients on levothyroxine. Assessment of conformity to national guidance and variability in practice. Exp Clin Endocrinol Diabetes. 2017;125(9):625–33.
Busby J, Schroeder K, Woltersdorf W, Sterne JA, Ben-Shlomo Y, Hay A, Hollingworth W. Temporal growth and geographic variation in the use of laboratory tests by NHS general practices: using routine data to identify research priorities. Br J Gen Pract. 2013;63(609):e256–66.
Elwenspoek MMC, Scott LJ, Alsop K, Patel R, Watson JC, Mann E, Whiting P. What methods are being used to create an evidence base on the use of laboratory tests to monitor long-term conditions in primary care? A scoping review. Fam Pract. 2020;37(6):845–53.
Gregory JM, Slaughter JC, Duffus SH, et al. COVID-19 severity is tripled in the diabetes community: a prospective analysis of the pandemic’s impact in type 1 and type 2 diabetes. Diabetes Care. 2021;44(2):526–32.
NHS England. Optimising blood testing in primary and secondary care. September 2021. https://www.england.nhs.uk/publication/optimising-blood-testing-in-primary-and-secondary-care/. Accessed 9 November 2022
Royal College of Pathologists. Supply disruption of BD vacutainer blood specimen collection tubes. October 2021. https://www.rcpath.org/profession/on-the-agenda/supply-disruption-of-bd-vacutainer-blood-specimen-collection-tubes.html. Accessed 9 November 2022
Seidu S, Hambling C, Holmes P, Fernando K, Campbell NS, Davies S, Khunti K. The impact of the COVID pandemic on primary care diabetes services in the UK: a cross-sectional national survey of views of health professionals delivering diabetes care. Prim Care Diabetes. 2022;16(2):257–63.
Primary Care Diabetes Society. Prioritising primary care diabetes services during and post COVID-19 pandemic. September 2020. https://www.pcdsociety.org/news/details/prioritising-primary-care-diabetes-services-during-and-post-covid19-pandemic. Accessed 9 November 2022
Association of British Clinical Diabetologists. A quick guidance to risk stratification and recovery of diabetes services in the post-Covid-19 era. June 2020. https://abcd.care/sites/abcd.care/files/site_uploads/Resources/COVID-19/ABCD-Recovery-Guidance-2020-06-23.pdf. Accessed 9 November 2022
Holman N, Knighton P, Kar P, O’Keefe J, Curley M, Weaver A, Barron E, Bakhai C, Khunti K, Wareham NJ, Sattar N, Young B, Valabhji J. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823–33.
Heald AH, Jenkins DA, Williams R, Sperrin M, Fachim H, Mudaliar RN, Syed A, Naseem A, Gibson JM, Bowden Davies KA, Peek N, Anderson SG, Peng Y, Ollier W. The risk factors potentially influencing hospital admission in people with diabetes, following SARS-CoV-2 infection: a population-level analysis. Diabetes Ther. 2022;13(5):1007–21.
Hippisley-Cox J, Coupland CA, Mehta N, Keogh RH, Diaz-Ordaz K, Khunti K, Lyons RA, Kee F, Sheikh A, Rahman S, Valabhji J, Harrison EM, Sellen P, Haq N, Semple MG, Johnson PWM, Hayward A, Nguyen-Van-Tam JS. Risk prediction of covid-19 related death and hospital admission in adults after covid-19 vaccination: national prospective cohort study. BMJ. 2021;374: n2244.
Marmot M, Bell R. Fair society, healthy lives. Public Health. 2012;126(Suppl 1):S4–10.
Adler N, Singh-Manoux A, Schwartz J, Stewart J, Matthews K, Marmot MG. Social status and health: a comparison of British civil servants in Whitehall-II with European- and African-Americans in CARDIA. Soc Sci Med. 2008;66(5):1034–45.
Anderson SG, Shoo H, Saluja S, Anderson CD, Khan A, Livingston M, Jude EB, Lunt M, Dunn G, Heald AH. Social deprivation modifies the association between incident foot ulceration and mortality in type 1 and type 2 diabetes: a longitudinal study of a primary-care cohort. Diabetologia. 2018;61(4):959–67.
Wild SH, McKnight JA, McConnachie A, Lindsay RS. Socioeconomic status and diabetes-related hospital admissions: a cross-sectional study of people with diagnosed diabetes. J Epidemiol Community Health. 2010;64(11):1022–4.
Bachmann MO, Eachus J, Hopper CD, Davey Smith G, Propper C, Pearson NJ, Williams S, Tallon D, Frankel S. Socio-economic inequalities in diabetes complications, control, attitudes and health service use: a cross-sectional study. Diabet Med. 2003;20(11):921–9.
Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, Thornton PL, Haire-Joshu D. Social determinants of health and diabetes: a scientific review. Diabetes Care. 2020;44(1):258–79.
Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643–53.
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–12.
Valabhji J, Barron E, Gorton T, Bakhai C, Kar P, Young B, Khunti K, Holman N, Sattar N, Wareham NJ. Associations between reductions in routine care delivery and non-COVID-19-related mortality in people with diabetes in England during the COVID-19 pandemic: a population-based parallel cohort study. Lancet Diabetes Endocrinol. 2022;10(8):561–70.
NHS Digital. Quality and Outcomes Framework (QOF), enhanced services and core contract extraction specifications (business rules). https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-collections/quality-and-outcomes-framework-qof. Accessed 9 November 2022
Acknowledgements
The authors would like to thank Kayoko Yokoyama and David Smith for help with extracting the data for Cambridge University Hospital and for Mid-Cheshire Foundation Trust, respectively. Jonathon Howe is now based in the Blood Sciences Department, Cumberland Infirmary, Carlisle. AAF is the guarantor for this article.
Funding
The Rapid Service Fee was funded from AHH’s PI fund.
Author Contributions
AAF, DH, AHH and MS devised the original concept; CJD, HD, LG, JS, JDH, SR, IH, NG, AD, MS, AD and ML were responsible for the extraction and initial cleaning of the data from laboratory records at each of the ten centres; DH, AAF and JS performed the data manipulation and analysis; AHH, FWFH, PW and AAF provided the clinical interpretation; CJD, HD, LG, JS, JDH, SR, IH, NG, AD, MS, AD and ML provided data quality checking and interpretation of the results from each of their respective centres; AAF, AHH, DH, PW and FWFH wrote the initial draft of the paper, which was then critiqued by all other authors as part of regular team meetings and the manuscript revision process. All authors approved the final version of the manuscript.
Disclosures
David Holland has nothing to disclose. Adrian H. Heald has nothing to disclose. Fahmy F.W. Hanna has nothing to disclose. Mike Stedman has nothing to disclose. Pensée Wu has nothing to disclose. Julius Sim has nothing to disclose. Christopher J. Duff has nothing to disclose. Helen Duce has nothing to disclose. Lewis Green has nothing to disclose. Jonathan Scargill has nothing to disclose. Jonathon D. Howe has nothing to disclose. Sarah Robinson has nothing to disclose. Ian Halsall has nothing to disclose. Neil Gaskell has nothing to disclose. Andrew Davison has nothing to disclose. Mark Simms has nothing to disclose. Angela Denny has nothing to disclose. Martin Langan has nothing to disclose. Anthony A. Fryer has nothing to disclose.
Compliance with Ethics Guidelines
As this work represented an evaluation of the respective clinical biochemistry services, ethical committee approval was not required. Permission to access and use the information from the Laboratory Information and Management Systems was obtained from the relevant laboratory leads at each of the sites. All extracted data were fully anonymized before processing and analysis.
Prior Presentations
Work leading to this publication was presented at the Society for Endocrinology meeting in Harrogate, UK, in Nov. 2022.
Data Availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Holland, D., Heald, A.H., Hanna, F.F.W. et al. The Effect of the COVID-19 Pandemic on HbA1c Testing: Prioritization of High-Risk Cases and Impact of Social Deprivation. Diabetes Ther 14, 691–707 (2023). https://doi.org/10.1007/s13300-023-01380-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01380-x