Abstract
The aim of this narrative review is to present data on the role of continuous glucose monitoring (CGM) in the management of peripheral diabetic neuropathy (DPN) among individuals with type 1 and type 2 diabetes mellitus. Adequate glycaemic control is crucial to prevent the development or progression of DPN. CGM systems are valuable tools for improving glycaemic control and reducing glycaemic variability (GV). Chronic hyperglycaemia is known to be a risk factor for the development of diabetic microvascular complications, including DPN. In addition, there is now evidence that GV, evaluated by mean amplitude of glycaemic excursions, may be a novel factor in the pathogenesis of diabetic complications. Increased GV appears to be an independent risk factor for DPN and correlates with painful neuropathy. Similarly, time-in-range correlates positively with peripheral nerve function and negatively with sudomotor dysfunction. However, relevant studies are rather limited in scope, and the vast majority are cross-sectional and use different methodologies for the assessment of DPN. Therefore, the causal relationship between CGM-derived data and the development of DPN cannot be firmly established at the present time. It also remains to be elucidated whether CGM measures can be considered the new therapeutic targets for DPN management.
Similar content being viewed by others
Continuous glucose monitoring systems (CGM) provide valuable information on the levels of and variations in glucose, enabling a more personalised approach to diabetes management. |
Glycaemic variability (GV) may be a novel factor in the pathogenesis of diabetic complications. |
GV appears to be an independent risk factor for diabetic peripheral neuropathy (DPN) and correlates with painful neuropathy. |
Conversely, time-in-range correlates positively with peripheral nerve function and negatively with sudomotor dysfunction. |
It remains to be confirmed whether data from CGM may help define new therapeutic targets for DPN. |
Introduction
Diabetic peripheral neuropathy (DPN) is a common microvascular complication of diabetes mellitus (DM). Importantly, DPN is also the major risk factor for the development of diabetic foot ulcers, possibly leading to lower-extremity amputations [1]. Stringent glycaemic control remains the most important aspect of diabetic neuropathy management [2, 3].
The use of continuous glucose monitoring (CGM) devices has been associated with an improvement of glycaemic control. CGM is increasingly used due to its many advantages, namely accuracy and easiness of use, as well as the ability to assess daily variations in glucose [4]. Thus, the use of CGM devices may improve therapeutic decisions in comparison with conventional self-monitoring blood glucose (SMBG) systems [4].
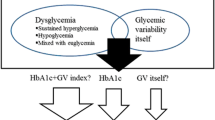
Glycated haemoglobin A1c (HbA1c) remains the reference marker for assessing glycaemic control and predicting the risk of future diabetes complications. Nonetheless, HbA1c has several limitations in this context. First, it provides the average glucose level over the previous 2–3 months but offers no information on glycaemic variability (GV) or hypoglycaemic events on a daily basis. Second, HbA1c can be affected by multiple factors, as age, race, anaemia, haemoglobinopathies, iron deficiency, chronic kidney disease and pregnancy, resulting in discrepancies between the measured HbA1c and true glycaemic control. For these reasons, HbA1c is not a valuable tool for a personalised diabetes management [5, 6].
On the contrary, CGM systems with CGM metrics provide more information on daily glycaemic status and glucose variations [7]. GV describes the intra-day glycaemic excursions, including episodes of hyperglycaemia and hypoglycaemia. CGM systems can more accurately detect GV than SMBG systems, and GV can be evaluated from CGM data using complex formulas [7]. Although chronic hyperglycaemia is known to enhance the risk for diabetes complications, both postprandial spikes of glucose and hypoglycaemias have also been reported to be associated with cardiovascular events in diabetes [7, 8]. A potential association between GV and autonomic neuropathy has also been reported [8]. More importantly, there is increasing evidence for a role of GV in the development of diabetic microvascular complications [9]. Also, GV has been proposed to be a predictor of diabetic complications independently of HbA1c in persons with type 2 DM (T2DM) [10].
Time-in-range (TIR) is defined as the percentage of time at glucose levels ranging from 70 to 180 mg/dL (3.9–10.0 mmol/L). This metric is considered to be an emerging surrogate marker of glycaemic control and to correlate with HbA1c [11]. Although HbA1c remains the key surrogate marker for the development of long-term diabetes complications, TIR has been also associated with microvascular complications (diabetic retinopathy and microalbuminuria) [11].
The role of CGM systems on preventing or improving DPN has not been extensively investigated. In the present narrative review, we summarise emerging data on the relationship of TIR and GV (evaluated by CGM systems) with DPN.
Methods
Search Strategy
For this narrative review, we searched relevant published articles in PubMed up to January 2022 using combinations of the key words “continuous glucose monitoring” and “diabetic peripheral neuropathy”. The electronic search yielded 68 articles (including 12 reviews). Those articles addressing an association or lack of association of CGM with DPN were included in this review, and ten articles were excluded. Searches were not restricted by study design, but only articles published in the English language were included.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Categories of CGM Systems
CGM systems can be divided in real-time CGM (rtCGM) and intermittently scanned CGM (isCGM) systems (also called “flash” CGM). CGMs use a sensor to measure interstitial fluid glucose and, therefore, finger-sticks are not needed, thus allowing the individual to avoid pain derived from blood glucose measurements [7, 12].
An important difference between the two CGM systems is the way data are transmitted to the user. RtCGM systems can automatically transmit data to the user’s receiver and/or smartphone [12], while isCGM systems require the patient to “swipe” the receiver close to the sensor to obtain glucose data. Most importantly, users of isCGM systems must scan at least every 8 h with the device, as only the most recent data of the last 8 h will be retained and available for evaluation.
Both CGM systems provide information on glucose levels during sleep. Similarly, both rtCGM and isCGM devices are able to provide a “high” or “low” alarm when glucose levels are above or below the target range, respectively, thus protecting patients from dangerous episodes of hyper- or hypoglycaemia. Some systems can also share data with clinicians or family/caregivers [12] and thus enable improved glycaemic control among children or people who need help in the adjustment of insulin dose. Moreover, certain CGMs can also be combined with an insulin pump, allowing automatic adjustment or interruption of insulin delivery should significant changes in glucose occur [13].
Commonly Used CGM Metrics
Among all standardised CGM metrics [4], the most commonly used are:
-
Average glucose: average glucose level is highly correlated with HbA1c and measures of hyperglycaemia, but this metric provides no information on GV.
-
GV: GV describes the intra-day glycaemic excursions, including episodes of hyperglycaemia and hypoglycaemia. It is an index that can be affected by diet, lifestyle, comorbidities, as well as by diabetes treatment and insulin injection technique [14].
-
Mean amplitude of glycaemic excursion (MAGE): MAGE is a simple index of GV. It is the mean of blood glucose values exceeding one standard deviation (SD) from the 24-h mean blood glucose and has been proposed as the “gold standard” for assessing the short-term within-day GV [15].
-
Glucose management indicator (GMI): This index calculates an approximate HbA1c based on the average glucose level measured by CGM and enables glucose management and individual goals when the laboratory HbA1c and the estimated HbA1c do not closely match. GMI provides the current state of a person’s glucose management [16].
-
TIR: TIR is the most commonly used CGM metric. It is the duration of time that a patient’s glucose level is in the target range, usually between 70 and 180 mg/dL (3.9–10.0 mmol/L). The use of CGM systems has been associated with increased TIR and reduced incidence of severe episodes of hypoglycaemia [16].
-
Time-below-range (TBR): This metric is the duration of time that a patient’s glucose level is < 70 mg/dL (3.9 mmol/L) or < 54 mg/dL (< 3 mmol/L]. It is a valuable parameter for optimising glucose management [12]. An ideal CGM target is a high TIR with a minimal TBR.
-
Time-above-Range (TAR): This metric is the duration of time that a patient’s glucose level is > 180 mg/dL (> 10 mmol/L) or > 250 mg/dL (> 13.9 mmol/L). It is also an important parameter for optimising glucose management [12].
CGM and DPN
CGM and DPN in T2DM
The relationship between GV and DPN was evaluated in a study conducted among 90 well-controlled subjects with T2DM (HbA1c < 7.0%). Of these subjects, 45 had DPN and were recruited from an inpatient department of the Second Affiliated Hospital of Nantong University (China) and 45 had no DPN and were recruited from outpatient as controls [7]. The two groups were matched for age and T2DM duration. The diagnosis of DPN was based on the criteria recommended by The Toronto Diabetic Neuropathy Expert Group, including the presence of a symptom/symptoms (decreased sensation, positive neuropathic sensory symptoms predominantly in the toes, feet or legs) or a sign/signs of neuropathy (symmetric decrease of distal sensation or unequivocally decreased or absent ankle reflexes) and presence of abnormality of nerve conduction (NC) test results [7]. Glucose was monitored with a CGM system (MiniMed system; Medtronic, Northridge, CA, USA) for 72 h [7]. GV was estimated with multiple parameters, such as glucose SD (SDgluc), mean of daily differences (MODD) and MAGE. Blood pressure, body mass index (BMI) and laboratory parameters were measured, included insulin sensitivity index (ISI; Matsuda index), total cholesterol, triglycerides, high-density lipoprotein cholesterol and low-density lipoprotein cholesterol [7]. Subjects with DPN had higher SDgluc, MODD and MAGE (p < 0.05). Multivariate logistic regression analysis revealed a significant correlation of DPN with MAGE (odds ratio [OR] 2.05, 95% confidence interval [CI] 1.36–3.09, p = 0.001) and BMI (OR 0.85, CI 0.73–0.99, p = 0.033) [7].
Similarly, another study of 982 subjects with T2DM (197 with DPN) from the inpatient department of the Affiliated Hospital of Nantong University and Second Affiliated Hospital of Nantong University (China) examined the association of GV and other conventional risk factors with DPN [17]. DPN was diagnosed based on both neuropathic symptoms/signs and abnormal NC test results. Using a CGM system (Gold system; Medtronic), multiple GV parameters were calculated, including MACE, MODD, SD and 24-h mean glucose (24-h MG). Those T2DM subjects with DPN exhibited higher MAGE, MODD, SD, and 24-h MG (p < 0.001) [10]. Regression analysis showed that MAGE, T2DM duration, Homeostasis model assessment for insulin resistance (HOMA-IR) and HbA1c were independent risk factors for DPN (OR 4.57, 95% CI 3.48–6.01; OR 1.10, 95% CI 1.03–1.17; OR 1.24, 95% CI 1.09–1.41; OR 1.33, 95% CI 1.15–1.53, respectively). Moreover, 4.60 mmol/L was the optimal MAGE cutoff for DPN identification (sensitivity 64.47%, specificity 75.54%) [17].
The Continuous Glucose Monitoring to Assess Glycemia in Chronic Kidney Disease (CANDY) study enrolled 105 subjects with T2DM who were treated with insulin or sulfonylurea (81 with moderate-to-severe chronic kidney disease [CKD] and estimated glomerular filtration rate [eGFR] < 60 mL/min/1.73 m2) and 24 controls from the same centre (eGFR ≥ 60 mL/min/1.73 m2). Glucose was monitored using a CGM system for two 6-days periods [18]. Participants were enrolled from nephrology clinics, the Diabetes Care Centre and referring clinics associated with the University of Washington, Seattle (USA). TIR (glucose 70–180 mg/dL) and GMI were assessed. DPN was diagnosed by the Michigan Neuropathy Screening Instrument (MNSI) questionnaire. DPN was seen in 63% of participants with CKD and in 46% of controls. Lower TIR and higher GMI were associated with a higher risk of DPN symptoms (OR 1.25, 95% CI 1.02–1.52) per 10% lower TIR; OR 1.79, 95% CI 1.05–3.04 per 1% higher GMI). Interestingly, no significant association between laboratory HbA1c values and DPN symptoms was observed [18]. The majority of participants in this study had CKD. As one explanation of these results, the authors commented that as CKD is a factor affecting HbA1c (HbA1c tends to be lower in individuals with end-stage-kidney disease), HbA1c in the enrolled patients with CKD was a less precise parameter for estimating glucose management compared with CGM metrics (TIR and GMI). Other potential explanations for their findings could include the limitations acknowledged by the authors: the cross-sectional observational design of the study, the relatively small sample size, the diagnosis of DPN by subjective symptoms (MNSI questionnaire), as well as the CGM-data being obtained from two 6-day-periods [18]. In view of the association between lower TIR and DPN symptoms, the need for adequate glycaemic control to prevent DPN was implied [18].
In agreement with these findings, the authors of another study reported for the first time a link between TIR and peripheral nerve function among 740 patients with T2DM patients [19]. TIR was assessed by CGM (Medtronic). Participants were divided into tertiles according to TIR values (low TIR: ≤ 53%; medium TIR: 54–76%; high TIR: ≥ 77%), and composite Z-scores of nerve conduction velocity (NCV), latency and amplitude were calculated [12]. Higher TIR values were associated with elevated composite Z-scores of NCV and amplitude and lower composite Z-scores of latency (all p < 0.05) [19]. In addition, the risk of TIR tertiles and worsening NCV was independent of HbA1c (medium TIR: OR 0.48, p = 0.001; high TIR: OR 0.41, p < 0.001) [19]. Specifically, the authors used linear regression analysis to explore whether HbA1c or TIR was more strongly associated with peripheral nerve function. HbA1c was more closely related to the composite Z-score of the nerve function parameters, but TIR had an additional role [19]. Moreover, the risk of reduced NCV decreased with higher TIR after controlling for HbA1c and other parameters. Finally, according to ROC analysis, adding TIR to the models increased the predictive performance of the logistic models to decreased NCV and to amplitude, suggesting that TIR might assess peripheral nerve function independent of HbA1c [19]. Of note, the study was conducted among hospitalised patients and, therefore, the results must be carefully interpreted when extrapolating to the general/outpatient population [19].
Guo et al. [20] investigated the relationship between TIR and sudomotor function among 466 in-patients at the Endocrinology Department of Jinling Hospital, Nanjing with T2DM. Sudomotor function was assessed using Sudoscan technology (SUDOSCAN Inc., San Diego, CA, USA). TIR was evaluated after 3 days of CGM (Meiqi Corp., Shenzhen, Guangdong, China) [20]. Overall, 135 participants exhibited sudomotor dysfunction (28.9%) and low TIR. A TIR value within the middle and the highest tertiles was associated with a lower prevalence of sudomotor dysfunction (20.51% and 21.94% vs. 44.52%, p < 0.001) [13]. Moreover, after adjustment for confounding factors, TIR appeared to be inversely and independently associated with the presence of sudomotor dysfunction (OR 0.979, 95% CI 0.971–0.987, p < 0.001) [20].
Interestingly, the association between subclinical diabetic polyneuropathy and GV has also been studied [21]. Among 509 subjects with T2DM (147 with DPN) admitted to the Endocrinology Department of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital (Shanghai, China), a significant association was revealed between SDgluc and abnormal nerve function (OR 1.198, 95% CI 1.027–1.397). Moreover, the composite Z-score of NCV and response amplitude decreased witn increasing SDgluc (p < 0.05) [21]. Even after adjustment for potential confounders (age, sex, BMI, HbA1c and diabetes duration), high SDgluc was independently associated with slower NCV (b = − 0.124, p = 0.021) [21].
Finally, in an study of 281 outpatients with T2DM, as part of a multi-centre prospective cohort study (Hyogo Diabetes Hypoglycemia Cognition Complications [HDHCC] study, Japan), glucose was monitored with FreeStyle Libre Pro (Abbott Japan, Tokyo, Japan) during a 10-day period [22]. DPN was diagnosed by a combination of symptoms, signs, vibration perception threshold and NC parameters [22]. Multiple regression analyses revealed that DPN was associated with TIR deterioration (standard partial regression coefficient β = − 0.106, p = 0.033) [22].
In conclusion, studies performed to date in subjects with T2DM have shown an association of GV with DPN and painful neuropathy. Of note, GV has been also associated with subclinical DPN. These findings are in accordance with data derived from other studies which showed that worsening glycaemic control and GV are associated with the development and progression of complications in diabetes [23, 24].
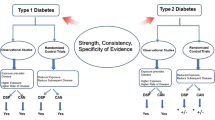
CGM and DPN in Type 1 Diabetes Mellitus
Oyibo et al. [25] have examined the relationship between blood glucose excursions and painful diabetic neuropathy among 20 patients with type 1 DM (T1DM) and DPN randomly selected (10 with painful DPN and 10 with pain-free DPN). A CGM system (MiniMed system; Medtronic) was used for 3 days and MAGEs subsequently evaluated. Both groups, with and without pain, were similar in terms of age, T1DM duration, duration of neuropathy and CGM performance [25]. Mean glucose levels (p = 0.02) and M-values (as a measure of GV) (p = 0.02) were higher among T1DM subjects with painful neuropathy and, similarly, glucose excursions were more frequent among those subjects with painful DPN (p < 0.01); however, MAGE was similar between the two groups [25]. The authors suggested that reduced GV could contribute to the treatment of painful diabetic neuropathy, but we should bear in mind that this was a small study and the results need confirmation [25].
Kwai et al. [26] investigated the role of GV on peripheral nerve function among 17 patients with T1DM using a CGM system (Enlite sensor; Medtronic) and nerve excitability techniques. Patients were recruited consecutively from the Prince of Wales Hospital in Sydney (Australia). MAGE was calculated to quantify GV [26]. There were significant correlations of MAGE with excitability markers of altered motor and sensory axonal function (superexcitability: r = 0.54; S2 accommodation: r = − 0.76; minimum current/voltage (I/V) slope (expressed as rate of change per unit): r = 0.71; strength duration time constant: r = 0.66; latency: r = 0.65) (p < 0.05). Interestingly, there was no association between acute glucose levels and markers of axonal function [26].
The authors of another study included 159 subjects with T1DM and examined whether optimised glycaemic control (measured by improved HbA1c) could improve vibration perception thresholds (VPTs) [27]. The latter were measured at six frequencies (range: 4–125 Hz) at the heads of the first and fifth metatarsal bones using a VibroSense Meter (VibroSense Dynamics, Malmö, Sweden). Patients were being treated at the Department of Endocrinology, Skåne University Hospital, Malmö (Sweden) and were examined twice between 2015 and 2018. Among those participants whose HbA1c improved by > 1 mmol/mol (95 subjects), the mean Z-score, reflecting the combined effect of all VPTs, also improved and was lower at the follow-up compared with that at the baseline (0.2 [− 0.3 to 1.2] vs. − 0.1 [− 0.7 to 0.8], p = 0.00002) [27]. In contrast, no difference in VPTs was observed among participants whose HbA1c was unchanged or deteriorated. The 4-Hz frequency was identified as the more sensitive frequency to detect improvements [27]. Unfortunately, GV was not measured in this study [27].
In a large U.S. population study that included 5936 participants with T1DM (T1D Exchange Clinic Registry), DPN was diagnosed by the Michigan Neuropathy Screening Instrument Questionnaire [28]. A CGM system was used by 33% of the participants. The authors found no difference between the subjects with and without DPN [28].
More recently, Feng et al. [29] examined the association between TIR (including nocturnal TIR) and sudomotor dysfunction in 95 subjects with T1DM (74.41% male) hospitalised in the Endocrinology Department of the Jinling Hospital, the First School of Clinical Medicine, Southern Medical University (China) to improve glucose control. TIR was measured using a 72-h blind CGM system (Meiqi Corp.). Sudomotor dysfunction was assessed using Sudoscan technology (Impeto Medical, Paris, France). Patients with sudomotor dysfunction exhibited lower TIR and nocturnal TIR, as well as higher TAR and nocturnal TAR in comparison with those free from sudomotor dysfunction [29]. Multiple regression analysis showed an inverse association of both TIR and nocturnal TIR with the risk of sudomotor dysfunction after adjustment for confounding factors [29].
CGM and DPN in Studies Including Subjects with Both T1DM and T2DM
Akaza et al. [30] examined the relationship between GV (estimated MAGE) and DPN in 40 outpatients of Shuuwa General Hospital (Saitama, Japan) with T1DM and T2DM (23 males and 17 females; age range: 34–79 years). Glucose levels were monitored with CGM, and DPN was diagnosed by NC study. In the multivariate linear regression analysis, MAGE was independently associated with a higher risk of medial plantar neuropathy (β = − 0.49, p = 0.007) [30].
Yan et al. looked at the association between TIR and the prevalence and degree of painful diabetic neuropathy among 364 patients with this condition [31]. Individuals were recruited at the Department of Endocrinology and Metabolism of Henan Provincial People’s Hospital (Zhengzhou, China). Based on a pain score, subjects were categorised into three groups: those who were pain-free and those with mild pain and moderate/severe pain, respectively. TIR was found to be associated with painful diabetic neuropathy, and was significantly lower among subjects with mild or moderate/severe pain than in those who reported no pain (p < 0.05) [31]. Moreover, the prevalence of pain decreased with increasing TIR (p < 0.05). Logistic regression analysis showed that lower TIR levels were significantly associated with an increasing risk of painful neuropathy (p < 0.05) [31].
In summary, GV has been associated not only with DPN but also with painful neuropathy. The pathogenesis of DPN involves several mechanisms. Of these, oxidative stress (induced by hyperglycaemia and acute glucose fluctuations) is receiving considerable attention [32]. Moreover, data support the possibility that GV could activate oxidative stress in a more intensive way than chronic hyperglycaemia [17, 33].
CGM and Diabetic Foot
Very limited data are available on TIR and clinical outcomes among patients with diabetic foot and diabetic foot ulcers (DFUs). The association of TIR with amputation and all-cause mortality was assessed retrospectively among 303 hospitalised patients with DFUs. The amputation rate and all-cause mortality was found to decline with increasing TIR [34]. Logistic regression analysis showed an inverse association of TIR with both amputation (p = 0.034) and all-cause mortality (p = 0.013) after controlling for multiple confounders [34].
Huang et al. studied the association of TIR with postoperative wound healing among patients with DFUs [35]. The results showed that participants with TIR < 50% were more likely to undergo second surgery within 1 month (p = 0.032) and to stay longer in hospital (p = 0.045). In the multivariate analysis, TIR was also an independent risk factor for second surgery (p = 0.034), implying that high TIR should be sought in DFU patients undergoing surgery [35].
Additional prospective data on the role of CGM systems in improving outcomes among DFU patients are needed. Such outcomes might include wound healing, re-ulceration, amputation rates, quality of life, among others.
Discussion
In this review we discuss the associations of glycaemic control based on CGM measures and the prevalence of DPN among subjects with T1DM and T2DM (Table 1). Current evidence points to a potential association between GV or TIR and DPN. However, there are some caveats to this statement. First, the number of studies are limited, the majority of studies that have been performed involved mostly Asian populations and the vast majority of these studies are cross-sectional in design. Second, many participants were in-patients and, therefore, the findings cannot be applied to a general outpatient setting. Third, studies have used varying criteria for the assessment and definition of DPN, as well as various CGM systems. CGM has been used for limited time periods and various parameters (VG or TIR) have been assessed.
It is evident that the pathogenesis of DPN involves several mechanisms, with chronic hyperglycaemia being an established cardinal factor. It is interesting that not only hyperglycaemia per se but also acute glucose fluctuations induce oxidative stress, a relationship that has received considerable attention [25]. Some data support GV activating oxidative stress more than chronic hyperglycaemia [10, 26]. Intermittent high blood glucose exposure, rather than constant exposure to high blood glucose, has been shown to have deleterious effects in experimental studies [9].
The effect of GV on DPN has not been extensively studied. Possible mechanisms that are involved in the role of GV on DPN include the activation of protein kinase C-dependent NADPH oxidase, which leads to oxidative stress and GV-induced apoptosis of Schwann cells. Moreover, GV seems to significantly decrease the expression of superoxide dismutase and increase the levels of tumour necrosis factor alpha, interleukin-6, nuclear factor kappa B (NF-kB) and malondialdehyde. In summary, GV induces oxidative stress and inflammatory response by activating the NF-kB pathway, thereby causing DPN [36].
GV has also been associated with an increased incidence of hypoglycaemia. Hypoglycaemia induces multiple inflammatory and endocrine responses (sympatho-adrenal response), including the release of inflammatory cytokines, the increase in platelet and neutrophil activation and increased adrenaline secretion, leading to endothelial dysfunction and thus decreased vasodilatation. Therefore, GV appears to play an important role in vascular damage [9].
Of note, an association between GV and the severity of autonomic neuropathy in T1DM has already been observed. In addition, reduced beta-cell function is a very important risk factor for GV. A negative association has been reported between C-peptide levels and GV in T1DM [37]. Reducing GV and optimising TIR using CGM systems might be a possible strategy to reduce the occurrence of DPN and other diabetes complications.
In this overall context, CGM systems can automatically measure glucose every 5 min, which is approximately 288 readings a day [13]. For an accurate interpretation of CGM readings, sufficient CGM data must be available. Minimum use of a CGM system is considered to be > 14 days, with the CSM system worn for at least 10 days (70%), to obtain reliable information [12]. Data on 14 days provide a good estimation of glucose metrics for a 3-month period [38]. Thus, longitudinal studies in large populations from various countries in which CGM systems are used for longer time periods are needed to establish a causal relationship among CGM measures and DPN.
Evidence presented in this review suggests that adequate glycaemic control according to CGM measures could be associated with DPN, as well as with subclinical DPN and, more interestingly, with symptoms of pain among patients with DPN. HbA1c is currently still the key surrogate marker for the development of long-term diabetes complications. However, HbA1c has several limitations, rendering CGM systems as an alternative very interesting [39]. Thus, it remains to be established whether, in comparison to HbA1c, stringent glycaemic control defined by lower GV and higher TIR levels could be more efficiently correlated with the development of DPN and whether CGM could provide new therapeutic targets for the prevention of DPN.
Conclusions
Stringent glycaemic control is crucial in order to prevent the development and progression of DPN. Emerging evidence suggests that GV (MAGE) may be a novel factor in the pathogenesis of diabetic complications, and significant associations have been reported between CGM-derived data (TIR and GV) and DPN. However, the number of studies are currently limited. Most of the studies carried out to date are cross-sectional and have used different methodologies for the assessment of DPN, while the duration of CGM use has also been very limited. Therefore, the causal relationship between CGM-derived data and the development of DPN cannot be firmly established at this time. It also remains to be elucidated whether CGM measures could be considered the new therapeutic targets for DPN management.
References
Bönhof GJ, Herder C, Strom A, Papanas N, Roden M, Ziegler D. Emerging biomarkers, tools, and treatments for diabetic polyneuropathy. Endocr Rev. 2019;40:153–92.
Bondar A, Popa AR, Papanas N, et al. Diabetic neuropathy: a narrative review of risk factors, classification, screening and current pathogenic treatment options (Review). Exp Ther Med. 2021;22:690.
Ziegler D, Papanas N, Schnell O, et al. Current concepts in the management of diabetic polyneuropathy. J Diabetes Investig. 2021;12:464–75.
Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42:1593–603.
Beck RW, Connor CG, Mullen DM, et al. The fallacy of average: how using HbA1c alone to assess glycemic control can be misleading. Diabetes Care. 2017;40:994–9.
Danne T, Nimri R, Battelino T, et al. International consensus on use of continuous glucose monitoring. Diabetes Care. 2017;40:1631–40.
Xu F, Zhao LH, Su JB, et al. The relationship between glycemic variability and diabetic peripheral neuropathy in type 2 diabetes with well-controlled HbA1c. Diabetol Metab Syndr. 2014;6:139.
Kalopita S, Liatis S, Thomakos P, et al. Relationship between autonomic nervous system function and continuous interstitial glucose measurement in patients with type 2 diabetes. J Diabetes Res. 2014;2014:835392.
Suh S, Kim JH. Glycemic variability: how do we measure it and why is it important? Diabetes Metab J. 2015;39:273–82.
Nalysnyk L, Hernandez-Medina M, Krishnarajah G. Glycaemic variability and complications in patients with diabetes mellitus: evidence from a systematic review of the literature. Diabetes Obes Metab. 2010;12:288–98.
Beck RW, Bergenstal RM, Riddlesworth TD, et al. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care. 2019;42:400–5.
Galindo RJ, Aleppo G. Continuous glucose monitoring: the achievement of 100 years of innovation in diabetes technology. Diabetes Res Clin Pract. 2020;170:108502.
Funtanilla VD, Candidate P, Caliendo T, Hilas O. Continuous glucose monitoring: a review of available systems. P T. 2019;44:550–3.
Chehregosha H, Khamseh ME, Malek M, Hosseinpanah F, Ismail-Beigi F. A view beyond hba1c: role of continuous glucose monitoring. Diabetes Ther. 2019;10:853–63.
Zhou Z, Sun B, Huang S, Zhu C, Bian M. Glycemic variability: adverse clinical outcomes and how to improve it? Cardiovasc Diabetol. 2020;19:102.
Bergenstal RM, Beck RW, Close KL, et al. Glucose Management Indicator (GMI): a new term for estimating a1c from continuous glucose monitoring. Diabetes Care. 2018;41:2275–80.
Hu YM, Zhao LH, Zhang XL, et al. Association of glycaemic variability evaluated by continuous glucose monitoring with diabetic peripheral neuropathy in type 2 diabetic patients. Endocrine. 2018;60:292–300.
Mayeda L, Katz R, Ahmad I, et al. Glucose time in range and peripheral neuropathy in type 2 diabetes mellitus and chronic kidney disease. BMJ Open Diabetes Res Care. 2020;8:e000991.
Li F, Zhang Y, Li H, et al. TIR generated by continuous glucose monitoring is associated with peripheral nerve function in type 2 diabetes. Diabetes Res Clin Pract. 2020;166:108289.
Guo QY, Lu B, Guo ZH, et al. Continuous glucose monitoring defined time-in-range is associated with sudomotor dysfunction in type 2 diabetes. World J Diabetes. 2020;11:489–500.
Pan J, Yan X, Li F, Zhang Y, Jiang L, Wang C. Association of glycemic variability assessed by continuous glucose monitoring with subclinical diabetic polyneuropathy in type 2 diabetes patients. J Diabetes Investig. 2021;13:328–35.
Kuroda N, Kusunoki Y, Osugi K, et al. Relationships between time in range, glycemic variability including hypoglycemia and types of diabetes therapy in Japanese patients with type 2 diabetes mellitus: Hyogo Diabetes Hypoglycemia Cognition Complications study. J Diabetes Investig. 2021;12:244–53.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
Jin SM, Kim TH, Oh S, et al. Association between the extent of urinary albumin excretion and glycaemic variability indices measured by continuous glucose monitoring. Diabet Med. 2015;32:274–9.
Oyibo SO, Prasad YD, Jackson NJ, Jude EB, Boulton AJ. The relationship between blood glucose excursions and painful diabetic peripheral neuropathy: a pilot study. Diabet Med. 2002;19:870–3.
Kwai NC, Arnold R, Poynten AM, Krishnan AV. Association between glycemic variability and peripheral nerve dysfunction in type 1 diabetes. Muscle Nerve. 2016;54:967–9.
Dahlin LB, Elgzyri T, Löndahl M, Ekman L, Lindholm E. Improved metabolic control using glucose monitoring systems leads to improvement in vibration perception thresholds in type 1 diabetes patients. Acta Diabetol. 2020;57:433–8.
Mizokami-Stout KR, Li Z, Foster NC, et al. The contemporary prevalence of diabetic neuropathy in type 1 diabetes: findings from the T1D exchange. Diabetes Care. 2020;43:806–12.
Feng ZQ, Guo QY, Wang W, et al. Time in range, especially overnight time in range, is associated with sudomotor dysfunction in patients with type 1 diabetes. Diabetol Metab Syndr. 2021;13:119.
Akaza M, Akaza I, Kanouchi T, Sasano T, Sumi Y, Yokota T. Nerve conduction study of the association between glycemic variability and diabetes neuropathy. Diabetol Metab Syndr. 2018;10:69.
Yang J, Yang X, Zhao D, Wang X, Wei W, Yuan H. Association of time in range, as assessed by continuous glucose monitoring, with painful diabetic polyneuropathy. J Diabetes Investig. 2021;12:828–36.
Jin HY, Lee KA, Park TS. The impact of glycemic variability on diabetic peripheral neuropathy. Endocrine. 2016;53:643–8.
Monnier L, Mas E, Ginet C, et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295:1681–7.
Xie P, Deng B, Zhang X, et al. Time in range in relation to amputation and all-cause mortality in hospitalised patients with diabetic foot ulcers. Diabetes Metab Res Rev. 2022;38: e3498.
Huang ZX, Zhang HH, Huang Y, et al. Association of time in range with postoperative wound healing in patients with diabetic foot ulcers. Int Wound J. 2021. https://doi.org/10.1111/iwj.13725.
Zhang X, Yang X, Sun B, Zhu C. Perspectives of glycemic variability in diabetic neuropathy: a comprehensive review. Commun Biol. 2021;4:1366.
Nyiraty S, Pesei F, Orosz A, et al. Cardiovascular autonomic neuropathy and glucose variability in patients with type 1 diabetes: is there an association? Front Endocrinol (Lausanne). 2018;9:174.
Riddlesworth TD, Beck RW, Gal RL, et al. Optimal sampling duration for continuous glucose monitoring to determine long-term glycemic control. Diabetes Technol Ther. 2018;20:314–6.
Bellido V, Pinés-Corrales PJ, Villar-Taibo R, Ampudia-Blasco FJ. Time-in-range for monitoring glucose control: Is it time for a change? Diabetes Res Clin Pract. 2021;177:108917.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Both authors contributed to the article in a substantive and meaningful manner. Evanthia Gouveri and Nikolaos Papanas were involved in article conception and design; Evanthia Gouveri searched and interpreted literature and wrote the first draft; Nikolaos Papanas finalised the draft. Both authors have read and agreed to the published version of the manuscript.
Disclosures
Evanthia Gouveri has attended conferences sponsored by Berlin-Chemie, Sanofi, AstraZeneca, Novo Nordisk, Lilly and Boehringer Ingelheim. Nikolaos Papanas has been an advisory board member of Astra-Zeneca, Boehringer Ingelheim, MSD, Novo Nordisk, Pfizer, Takeda and TrigoCare International; has participated in sponsored studies by Astra-Zeneca, Eli-Lilly, GSK, MSD, Novo Nordisk, Novartis and Sanofi-Aventis; has received honoraria as a speaker for Astra-Zeneca, Boehringer Ingelheim, Eli-Lilly, Elpen, MSD, Mylan, Novo Nordisk, Pfizer, Sanofi-Aventis and Vianex; and has attended conferences sponsored by TrigoCare International, Eli-Lilly, Galenica, Novo Nordisk, Pfizer and Sanofi-Aventis.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gouveri, E., Papanas, N. The Emerging Role of Continuous Glucose Monitoring in the Management of Diabetic Peripheral Neuropathy: A Narrative Review. Diabetes Ther 13, 931–952 (2022). https://doi.org/10.1007/s13300-022-01257-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01257-5