Abstract
In the present study, we aim to investigate the correlations between polymorphisms in the DEFB1 gene and the susceptibility to chronic respiratory diseases (CRDs). Electronic searches in multiple scientific literature databases (PubMed, EBSCO, Ovid, Springerlink, Wiley, Web of Science, Wanfang database, China National Knowledge Infrastructure database and VIP database) were made to retrieve studies on the associations between DEFB1 gene polymorphisms and CRDs. We used strict inclusion criteria in the present meta-analysis. Data analyses were performed with STATA software (version 12.0; Stata Corp, College Station, TX, USA). Of 76 initially-retrieved articles, 11 were finally incorporated into our meta-analysis, enrolling 1343 patients with CRDs (477 with chronic obstructive pulmonary disease (COPD), 305 with asthma, 286 with cystic fibrosis (CF), 130 with ventilator-associated pneumonia (VAP), 145 with pulmonary tuberculosis, and 1261 healthy controls into our meta-analysis. Our study showed that −44 C/G (rs1800972) and 1654 G/A (rs2738047) in DEFB1 are strongly associated with the increased susceptibility to CRDs. The subgroup analysis on disease types showed that the −44 C/G (rs1800972) in DEFB1 is associated with the susceptibility to COPD, VAP and CF, and the 1654 G/A (rs2738047) associated with the susceptibility to COPD and asthma. Subgroup analyses based on ethnicity indicated that −44 C/G (rs1800972) may confer increased susceptibility to CRDs in Asians but not in Caucasians. Taken together, −44 C/G (rs1800972) and 1654 G/A (rs2738047) are strongly associated with CRD susceptibility, while associations of SNPs −52 G/A (rs1799946) and −20 G/A (rs11362) with CRDs needs further investigation.
Similar content being viewed by others
Introduction
Chronic respiratory diseases (CRDs) are the main cause of premature mortality particularly in the elderly and the very young. Common risk factors for CRDs includes smoking, occupational dust exposure, household exposure to smoke from cooking stove or open fire as well as viral or bacterial infections (Mallia et al. 2012; Spagnolo et al. 2013; Chuchalin et al. 2014). CRD is the umbrella name for various diseases, including chronic obstructive pulmonary disease (COPD), asthma, bronchiectasis, cystic fibrosis (CF), bronchiolitis obliterans, interstitial lung disease, ventilator-associated pneumonia (VAP), pulmonary heart disease (PHD), and pulmonary tuberculosis (TB) (O’Kelly et al. 2011; Forfia et al. 2013; Kurpas et al. 2013; Valles et al. 2013; Greening et al. 2014).
COPD, one of the most common causes of mortality, accounts for 33 deaths per 100,000 people worldwide. Moreover, COPD is a complex syndrome with several pulmonary and extra-pulmonary components that develop over a long period, and its airflow limitation cannot be entirely reversed with current treatments (Alfageme et al. 2010; Han et al. 2010). Another kind of CRD, called VAP, develops with symptoms of pneumonia and occurs in mechanically ventilated patients, and VAP patients are twice as likely to die, with the mortality rate at 25 %, and its developing resistance to therapy resulting in a significant burden of recovery time and intensive care cost (Faisy et al. 2011; Grap et al. 2012; Rogers et al. 2014). CF, the most frequent inherited disease among white population (1 in every 2500 newborns), is induced by mutations in cystic fibrosis transmembrane conductance regulator (CFTR) gene (Spagnolo et al. 2013). As an airway disease, asthma is characterized by airflow limitation, bronchial hyper-responsiveness and chronic inflammation, increased presence of immune cells such as activated eosinophils, lymphocytes and mast cells. Also, asthma patients present clinically with symptoms of recurrent cough, chest tightness, wheezing, dyspnoea and mucus production (Bateman et al. 2008; Huang et al. 2011). TB is a well-known CRD, accounting for 8.6 million new infections each year and 1.3 million deaths in 2012, whose course can be significantly influenced by the status of host immune system and completely reversed with a combined drug therapy lasting up to 2 years (Gler et al. 2012; Png et al. 2012; Steingart et al. 2014). TB, when occurring with other morbidities that suppress immune functions, such as HIV infection, is extremely difficult to treat. CRDs are highly complicated disorders and have social ramifications, as seen by the prejudice against TB patients, causing a heavy burden on the society. Thus, the search for the effective diagnosis and treatment of CRDs remains a high priority in most health care systems across the world.
Human beta-defensins (HBD) are small peptides that play a crucial role in the innate immune responses, acting at the initial steps of immune defense against microbial infections. Thus, defensins possess antimicrobial abilities against fungi, bacteria and viruses and the defensin genes locate in a gene cluster mapped to human chromosome 8p22–23 (Taylor et al. 2008; Segat et al. 2010). The HDB1 is one of defensins, directly responsible for antimicrobial actions, and also plays a significant role in inflammation owing to its chemotactic activity for T cells and immature dendritic cells (Zaga-Clavellina et al. 2012). The gene encoding HBD1, DEFB1, spans approximately 8 kb, and expresses in various tissues, and its expression varies among individuals as a result of single nucleotide polymorphisms (SNPs) in the gene regulatory region (Ozturk et al. 2010; Prado-Montes de Oca 2010; Sandrin-Garcia et al. 2012). Previous studies have revealed that SNPs in 5′ untranslated region (UTR) of DEFB1 are associated with the CRDs, such as COPD and CF (Tesse et al. 2008; Andresen et al. 2011; Crovella et al. 2011; Lopez Campos et al. 2014). However, one study conducted in Italian patients with CF showed that there is no association between SNPs of DEFB1 and CDRs, and their polymorphisms may not be a modifier of CF disease and will not influence clinical outcomes (Segat et al. 2010). To better interpret controversial results from published studies, we performed this meta-analysis to further investigate the correlations between polymorphisms in DEFB1 gene and susceptibility to CRDs in human population.
Materials and methods
Data sources and search strategy
PubMed, EBSCO, Ovid, Wiley, Web of Science, Wanfang database, China National Knowledge Infrastructure (CNKI) and VIP database were searched for studies published from their start date to November 2014, using following search terms: (“chronic respiratory disease” or “asthma” or “chronic bronchitis “or “chronic obstructive pulmonary disease” or “pulmonary heart disease” or “pulmonary fibrosis” or “cystic fibrosis” or “pneumonia” or “pulmonary tuberculosis”) and (“defensin beta 1” or “DEFB1 protein” or “human DEFB1” or “hBD-1”) and “genetic polymorphism”.
Selection criteria
Studies were included based on following inclusion criteria: (1) studies were on the correlations between polymorphisms of DEFB1 and CRDs; (2) the study design was case–control study; (3) subjects in the study contained both patients with CRDs and healthy controls. The exclusion criteria were: (1) publications not in Chinese and English were excluded; (2) conference abstracts without sufficient data were excluded; (3) non-human studies were excluded. After the exclusion of duplicate or irrelevant articles, the full-text publications of the remaining ones were assessed according to the selection criteria, and their reference lists or bibliographies searched for other relevant articles.
Data extraction
Two authors independently extracted the data from eligible articles. Disagreements on inclusion were solved by discussion until a consensus was reached. Two authors reviewed entire articles that suited the inclusion criteria. The following information was extracted from each study: name of the first authors, year of publication, publication language, disease studied, study design, number of cases, ethnicity, gender, age, detection method, SNPs, and genotype frequencies. If the same patient population was documented in several studies, the most complete or latest study was selected for review to avoid duplication.
Statistical analysis
All analyses were performed on STATA (version 12.0; Stata Corp, College Station, TX, USA) software. The relative risk (RR) with 95 % confidence intervals (95 % CI) was utilized to evaluate the correlations between DEFB1 polymorphisms and CRDs, and the pooled RRs were estimated using the Z test. The present meta-analysis was conducted applying a random-effects model or a fixed-effects model to calculate the pooled RRs based on heterogeneity among studies, which was assessed with Cochran’s Q-statistic test (DerSimonian and Laird 1986) and I 2 statistic (DerSimonian 1996; Higgins et al. 2003). A fixed-effects model was applied to calculate parameters when heterogeneity was not an issue (I 2 < 50 %). When substantial heterogeneity (I 2 ≥ 50 %) existed, a random-effects model was utilized to pool data, and subgroup analyses were conducted to determine potential sources of heterogeneity. Publication bias was evaluated applying a method documented by Egger et al. (Egger et al. 1997). Moreover, we investigated causes for statistical heterogeneity through applying meta-regression, subgroup analysis and sensitivity analysis (Egger et al. 1997). All tests were two-sided, and P < 0.05 was recognized to be statistical significance.
Results
Study selection
Studies included in this meta-analysis were published between 2002 and 2014. A total number of 76 articles was retrieved initially through electronic database search and manual search, and 30 studies were retained after elimination of duplicates (n = 17), letters and reviews (n = 2), non-human studies (n = 3) as well as studies unrelated to the research topics (n = 28). In the final step of selection, 15 out of the remaining 26 studies were eliminated for insufficient information (Matsushita et al. 2002; Hu et al. 2004; Leung et al. 2006; Zhou et al. 2007a; Tesse et al. 2008; Li et al. 2008; Sun et al. 2010; Segat et al. 2010; Huang et al. 2012; Wu et al. 2012; Lopez Campos et al. 2014) Finally, based on our selection, we identified 11 case–control studies, which enrolled 1343 CRD patients with and 1261 healthy controls who were eligible for our meta-analysis. As shown in Fig. 1, there are 62 SNPs in DEFB1. In current meta-analysis, we only assessed 4 most common SNPs, −44 C/G (rs1800972), 1654 G/A (rs2738047), −52 G/A (rs1799946) and −20 G/A (rs11362). Three studies of this meta-analysis contained European and North American populations (one from Mexico, and two from Italy) and 8 studies involved Asian populations (seven from China, and one from Japan). Polymerase chain reaction-restriction fragment length polymorphism (PCR–RFLP) was used in six studies, TaqMan in two studies, direct sequencing in two studies, and polymerase chain reaction-single strand conformation polymorphism (PCR–SSCP)/direct sequencing/PCR–RFLP in one to detect SNPs. The sample sizes in these studies ranged from 92 to 461 subjects. The genotypic distributions were consistent with HWE (P > 0.05) for most SNPs, except for 1654 G/A (rs2738047) in the study of Leung TF (P = 0.001), −44 C/G (rs1800972) in Sun LR (P = 0.005), and −44 C/G (rs1800972) in Lopez Campos’ study (P = 0.003). The characteristics of recruited studies were showed in Table 1.
The correlations of −44 C/G (rs1800972) and 1654 G/A (rs2738047) polymorphisms in DEFB1 with the susceptibility to CRDs
The correlations of −44 C/G (rs1800972) with CRDs were reported in 9 studies, and the heterogeneity test suggested that there was significant heterogeneity among them (allele model: I 2 = 73.7 %, P h < 0.001; dominant model: I 2 = 74.9 %, P h < 0.001). No heterogeneity was observed among 3 studies that documented the correlations between 1654 G/A (rs2738047) with CRDs, thus a fixed-effects model was utilized (allele model: I 2 = 0.0 %, P h = 0.742; dominant model: I 2 = 0.0 %, P h = 0.881). The results of our meta-analysis indicated that −44 C/G (rs1800972) and 1654 G/A (rs2738047) polymorphisms were strongly associated with the susceptibility to CRDs, with statistical significance detected in both the allele and dominant models of genotype frequency difference between case group and control group (the allele model and dominant model of −44 C/G (rs1800972): RR = 0.82, 95 % CI = 0.71–0.95, P = 0.010; RR = 0.81, 95 % CI = 0.71–0.94, P = 0.004, respectively) (the allele model and dominant model of 1654 G/A (rs2738047): RR = 0.82, 95 % CI = 0.71–0.95, P = 0.010) (as shown in Fig. 2; Table 2).
We then conducted subgroup analyses on disease types and observed that the −44 C/G (rs1800972) was associated with the susceptibility to COPD, VAP and CF respectively (the allele model and dominant model of COPD: RR = 0.63, 95 % CI = 0.47–0.84, P = 0.001; RR = 0.65, 95 % CI = 0.50–0.85, P = 0.002, respectively) (the allele model of VAP: RR = 1.97, 95 % CI = 1.14–3.40, P = 0.015) (the dominant model CF: RR = 0.77, 95 % CI = 0.59–1.00, P = 0.048). The 1654 G/A (rs2738047) was also associated with the susceptibility to COPD and asthma (the allele model and dominant model of COPD: RR = 2.85, 95 % CI = 1.50–5.43, P = 0.001; RR = 2.82, 95 % CI = 1.47–5.43, P = 0.002, respectively) (the allele model and dominant model of asthma: RR = 4.35, 95 % CI = 1.84–10.28, P = 0.001; RR = 3.78, 95 % CI = 1.48–9.68, P = 0.006) (Fig. 3). Further subgroup analyses by ethnicity indicated that the −44 C/G (rs1800972) conferred increased susceptibility to CRDs in Asians but not in Caucasians (the allele model and dominant model of Asians: RR = 0.76, 95 % CI = 0.62–0.94, P = 0.009; RR = 0.75, 95 % CI = 0.62–0.91, P = 0.004) (the allele model and dominant model of Caucasians: RR = 0.91, 95 % CI = 0.73–1.14, P = 0.410; RR = 0.91, 95 % CI = 0.75–1.11, P = 0.363) (Fig. 4).
Forest plots on the associations of polymorphisms with the susceptibility of COPD, asthma, CF, VAP AND TB at −44 C/G (rs1800972), 1654 G/A (rs2738047), −52 G/A (rs1799946) and −20 G/A (rs11362) of DEFB1. Note DEFB1 beta-defensin gene, COPD chronic obstructive pulmonary disease, CF cystic fibrosis, VAP ventilator-associated pneumonia, TB pulmonary tuberculosis
The correlations of −52 G/A (rs1799946) and −20 G/A (rs11362) polymorphisms in DEFB1 with the susceptibility to CRDs
The correlations of −52 G/A (rs1799946) in DEFB1 with the susceptibility to CRDs were documented by 6 studies, and our results showed a significant heterogeneity among studies (the allele model and dominant model: I 2 = 51.8 %, P h = 0.065; I 2 = 61.8 %, P h = 0.023, respectively). There were also six studies reporting the relationship between −20 G/A (rs11362) in DEFB1 and the susceptibility to CRDs, with significant heterogeneity in allele model (I 2 = 74.9 %, P h < 0.001), and thus a random-effects model was applied. While no heterogeneity was found in the dominant model (I 2 = 0.0 %, P h = 0.586), a fixed-effects model was used. In our current meta-analysis, we uncovered that −52 G/A (rs1799946) and −20 G/A (rs11362) had no significant correlation with the susceptibility to CRDs, and the significant difference of genotype frequencies between case group and control group could not be seen under the allele model and dominant model (the allele model and dominant model of −52 G/A (rs1799946): RR = 0.96, 95 % CI = 0.85–1.09, P = 0.552; RR = 0.94, 95 % CI = 0.84–1.06, P = 0.334) (the allele model and dominant model of −20 G/A (rs11362): RR = 1.02, 95 % CI = 0.89–1.18, P = 0.738; RR = 0.98, 95 % CI = 0.90–1.06, P = 0.606) (Fig. 2; Table 2). However, we did find a significant association between −20 G/A (rs11362) in DEFB1 and the asthma susceptibility (the allele model: RR = 1.35, 95 % CI = 1.05–1.75, P = 0.019) (Fig. 3).
The sources of heterogeneity and publication bias
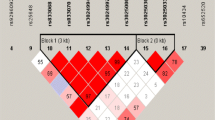
The sensitivity analysis showed that individual studies would not influence the pooled RRs values for correlations between DEFB1 gene polymorphisms and the susceptibility of CRDs (Fig. 4). The regression analysis results indicated that SNPs, diseases, year of publication, country, ethnicity, sample size, were not the main sources of heterogeneity or key factors influencing the overall effectiveness of the results (all P > 0.05) (shown in Fig. 5; Table 3). Contour-enhanced funnel plots were symmetrical, indicating that no obvious publication bias existed (all P > 0.05) (Fig. 6), and Egger’s linear regression tests also further confirmed this viewpoint (Fig. 7; Table 4).
Discussion
In current meta-analysis, we investigated the correlations of four SNPs of DEFB1 with CRDs. Our results showed that −44 C/G (rs1800972) and 1654 G/A (rs2738047) in DEFB1 are strongly associated with the susceptibility to CRDs, and there are significant differences of genotype frequencies between case group and control group in both allele and dominant models; while our analyses on −52 G/A (rs1799946) and −20 G/A (rs11362) of DEFB1 SNPs showed that they are not associated with the susceptibility to CRDs. DEFB1 expression is thought to control microbial flora and have the ability to kill a broad range of pathogens. The inductive role of defensins in bacterial or viral aggregation makes them the vital factor in reducing infectious titers and promoting clearance from the airway (Prado-Montes de Oca 2010; Tecle et al. 2010). Locating in exon 1 and within 5’UTR, −44 C/G can alter a NF-kB1 putative binding site, and thereby influence DEFB1 expression and induce multipleβ-defensins (Kalus et al. 2009; Prado-Montes de Oca et al. 2009). Coincidentally, some researchers suggested that −44 C/G is closely associated with the susceptibility to and fatal outcomes of severe sepsis while −20 G/A and −52 G/A are only associated with fatal outcomes (Chen et al. 2007). Being strongly correlated with chemoattractive activity of HBD-1, 1654 G/A (rs2738047) polymorphisms may reduce immune cell infiltration, promoting susceptibility to airway infection and leading to subsequent CRDs (Zhou et al. 2007a, b). The exact mechanism for the diverse effects of four SNPs on the susceptibility to CRD remains unknown. As suggested, bacteria have a counter mechanism through which bacterial surface components are altered, reducing binding ability of antimicrobial defensins and depressing the expression of HBDs in epithelial cells (Moranta et al. 2010). A possible explanation is that the transcriptional activity of DEFB1 varies in different loci.
We carried out subgroup analyses on disease types, and the results demonstrated that the −44 C/G (rs1800972) in DEFB1 was correlated with the susceptibility of COPD, VAP and CF, and the 1654 G/A (rs2738047) in DEFB1 was associated with the susceptibility of COPD and asthma. A possible reason for this result is that the pathogeneses of COPD, VAP and CF involve multiple risk factors other than bacterial infections. Furthermore, subgroup analyses based on ethnicity suggested that the −44 C/G (rs1800972) in DEFB1 might confer increased susceptibility to CRDs in Asians but not in Caucasians, possibly due to difference in living environments and health behaviors. Wallace reported less frequency of polymorphisms at −44 C/G, −52 G/A, −20 G/A in DEFB1 gene in Caucasians, suggesting the significant differences in the DEFB1 expression due to ethnicity (Wallace et al. 2006). There are limitations in current meta-analysis. For one, the literatures included in our study were mostly from Asians, only three out of eleven were done among Caucasians. For another, we only enrolled the CRDs including COPD, CF, VAP, TB and asthma. Finally, there was also the potential language bias in our meta-analysis in recruiting studies published only in English and Chinese, potentially excluding important studies in other languages that could have significantly influenced our study results.
Overall, the results of our meta-analysis suggested that two sites −44 C/G (rs1800972) and 1654 G/A (rs2738047) in DEFB1 are closely associated with the susceptibility to CRDs, while further studies are needed to determine the relationship between SNPs −52 G/A (rs1799946), −20 G/A (rs11362) in DEFB1 and the susceptibility to CRDs.
References
Alfageme I, Reyes N, Merino M, Reina A, Gallego J, Lima J, Palacios Z (2010) The effect of airflow limitation on the cause of death in patients with COPD. Chronic Respir Dis 7:135–145
Andresen E, Gunther G, Bullwinkel J, Lange C, Heine H (2011) Increased expression of beta-defensin 1 (DEFB1) in chronic obstructive pulmonary disease. PLoS One 6:e21898
Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, Gibson P, Ohta K, O’Byrne P, Pedersen SE et al (2008) Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J 31:143–178
Chen QX, Lv C, Huang LX, Cheng BL, Xie GH, Wu SJ, Fang XM (2007) Genomic variations within DEFB1 are associated with the susceptibility to and the fatal outcome of severe sepsis in Chinese Han population. Genes Immun 8:439–443
Chuchalin AG, Khaltaev N, Antonov NS, Galkin DV, Manakov LG, Antonini P, Murphy M, Solodovnikov AG, Bousquet J, Pereira MH et al (2014) Chronic respiratory diseases and risk factors in 12 regions of the Russian Federation. Int J Chronic Obstr Pulm Dis 9:963–974
Crovella S, Segat L, Amato A, Athanasakis E, Bezzerri V, Braggion C, Casciaro R, Castaldo G, Colombo C, Covone AE et al (2011) A polymorphism in the 5′ UTR of the DEFB1 gene is associated with the lung phenotype in F508del homozygous Italian cystic fibrosis patients. Clin Chem Lab Med 49:49–54
DerSimonian R (1996) Meta-analysis in the design and monitoring of clinical trials. Stat Med 15:1237–1248 (discussion 1249–1252)
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Faisy C, Candela Llerena M, Savalle M, Mainardi JL, Fagon JY (2011) Early ICU energy deficit is a risk factor for Staphylococcus aureus ventilator-associated pneumonia. Chest 140:1254–1260
Forfia PR, Vaidya A, Wiegers SE (2013) Pulmonary heart disease: the heart-lung interaction and its impact on patient phenotypes. Pulm Circ 3:5–19
Gler MT, Skripconoka V, Sanchez-Garavito E, Xiao H, Cabrera-Rivero JL, Vargas-Vasquez DE, Gao M, Awad M, Park SK, Shim TS et al (2012) Delamanid for multidrug-resistant pulmonary tuberculosis. N Engl J Med 366:2151–2160
Grap MJ, Munro CL, Unoki T, Hamilton VA, Ward KR (2012) Ventilator-associated pneumonia: the potential critical role of emergency medicine in prevention. J Emerg Med 42:353–362
Greening NJ, Williams JE, Hussain SF, Harvey-Dunstan TC, Bankart MJ, Chaplin EJ, Vincent EE, Chimera R, Morgan MD, Singh SJ et al (2014) An early rehabilitation intervention to enhance recovery during hospital admission for an exacerbation of chronic respiratory disease: randomised controlled trial. BMJ 349:g4315
Han MK, Agusti A, Calverley PM, Celli BR, Criner G, Curtis JL, Fabbri LM, Goldin JG, Jones PW, Macnee W et al (2010) Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med 182:598–604
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Hu RC, Xu YJ, Zhang ZX, Ni W, Chen SX (2004) Correlation of HDEFB1 polymorphism and susceptibility to chronic obstructive pulmonary disease in Chinese Han population. Chin Med J (Engl) 117:1637–1641
Huang YJ, Nelson CE, Brodie EL, Desantis TZ, Baek MS, Liu J, Woyke T, Allgaier M, Bristow J, Wiener-Kronish JP et al (2011) Airway microbiota and bronchial hyperresponsiveness in patients with suboptimally controlled asthma. J Allergy Clin Immunol 127(372–381):e371–e373
Huang LX, Wang GX, Tao F, Sun J (2012) Correlation of single nucleotide polymorphisms in human B-Defensin-1 gene with incidence and prognosis of ventilator-associsted pneumonia. Chin J Nosocomiol 22:2994–2997
Kalus AA, Fredericks LP, Hacker BM, Dommisch H, Presland RB, Kimball JR, Dale BA (2009) Association of a genetic polymorphism (−44 C/G SNP) in the human DEFB1 gene with expression and inducibility of multiple beta-defensins in gingival keratinocytes. BMC Oral Health 9:21
Kurpas D, Mroczek B, Knap-Czechowska H, Bielska D, Nitsch-Osuch A, Kassolik K, Andrzejewski W, Gryko A, Steciwko A (2013) Quality of life and acceptance of illness among patients with chronic respiratory diseases. Respir Physiol Neurobiol 187:114–117
Leung TF, Li CY, Liu EK, Tang NL, Chan IH, Yung E, Wong GW, Lam CW (2006) Asthma and atopy are associated with DEFB1 polymorphisms in Chinese children. Genes Immun 7:59–64
Li Y, Du Y, Jiang P, Zhai FZ (2008) Relationship of genetic polymorphisms of heme oxygenase-1, tumor necrosis factor-α, human β-defensin -1 with chronic obstructive pulmonary disease. Chin J Geriatr Med 27:333–336
Lopez Campos GN, Velarde Felix JS, Sandoval Ramirez L, Cazares Salazar S, Corona Nakamura AL, Amaya Tapia G, Montes Prado, de Oca E (2014) Polymorphism in cathelicidin gene (CAMP) that alters Hypoxia-inducible factor (HIF-1alpha:ARNT) binding is not associated with tuberculosis. Int J Immunogenet 41:54–62
Mallia P, Footitt J, Sotero R, Jepson A, Contoli M, Trujillo-Torralbo MB, Kebadze T, Aniscenko J, Oleszkiewicz G, Gray K et al (2012) Rhinovirus infection induces degradation of antimicrobial peptides and secondary bacterial infection in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 186:1117–1124
Matsushita I, Hasegawa K, Nakata K, Yasuda K, Tokunaga K, Keicho N (2002) Genetic variants of human beta-defensin-1 and chronic obstructive pulmonary disease. Biochem Biophys Res Commun 291:17–22
Moranta D, Regueiro V, March C, Llobet E, Margareto J, Larrarte E, Garmendia J, Bengoechea JA (2010) Klebsiella pneumoniae capsule polysaccharide impedes the expression of beta-defensins by airway epithelial cells. Infect Immun 78:1135–1146
O’Kelly S, Smith SM, Lane S, Teljeur C, O’Dowd T (2011) Chronic respiratory disease and multimorbidity: prevalence and impact in a general practice setting. Respir Med 105:236–242
Ozturk A, Famili P, Vieira AR (2010) The antimicrobial peptide DEFB1 is associated with caries. J Dent Res 89:631–636
Png E, Alisjahbana B, Sahiratmadja E, Marzuki S, Nelwan R, Balabanova Y, Nikolayevskyy V, Drobniewski F, Nejentsev S, Adnan I et al (2012) A genome wide association study of pulmonary tuberculosis susceptibility in Indonesians. BMC Med Genet 13:5
Prado-Montes de Oca E (2010) Human beta-defensin 1: a restless warrior against allergies, infections and cancer. Int J Biochem Cell Biol 42:800–804
Prado-Montes de Oca E, Velarde-Felix JS, Rios-Tostado JJ, Picos-Cardenas VJ, Figuera LE (2009) SNP 668C (−44) alters a NF-kappaB1 putative binding site in non-coding strand of human beta-defensin 1 (DEFB1) and is associated with lepromatous leprosy. Infect Genet Evol 9:617–625
Rogers AD, Deal C, Argent AC, Hudson DA, Rode H (2014) Ventilator associated pneumonia in major paediatric burns. Burns 40:1141–1148
Sandrin-Garcia P, Brandao LA, Guimaraes RL, Pancoto JA, Donadi EA, Lima-Filho JL, Segat L, Crovella S (2012) Functional single-nucleotide polymorphisms in the DEFB1 gene are associated with systemic lupus erythematosus in Southern Brazilians. Lupus 21:625–631
Segat L, Morgutti M, Athanasakis E, Trevisiol C, Amaddeo A, Poli F, Crovella S (2010) Analysis of DEFB1 regulatory SNPs in cystic fibrosis patients from North-Eastern Italy. Int J Immunogenet 37:169–175
Spagnolo P, Fabbri LM, Bush A (2013) Long-term macrolide treatment for chronic respiratory disease. Eur Respir J 42:239–251
Steingart KR, Schiller I, Horne DJ, Pai M, Boehme CC, Dendukuri N (2014) Xpert(R) MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev 1:CD009593
Sun LR, Zhang M, Li DM, Liu Z, Li SX, Gao Y, Zhang JL (2010) Study on the relationship between human beta -1 gene polymorphism and chronic obstructive pulmonary disease. J Med Res 161:81–84
Taylor K, Barran PE, Dorin JR (2008) Structure-activity relationships in beta-defensin peptides. Biopolymers 90:1–7
Tecle T, Tripathi S, Hartshorn KL (2010) Review: defensins and cathelicidins in lung immunity. Innate Immun 16:151–159
Tesse R, Cardinale F, Santostasi T, Polizzi A, Manca A, Mappa L, Iacoviello G, De Robertis F, Logrillo VP, Armenio L (2008) Association of beta-defensin-1 gene polymorphisms with Pseudomonas aeruginosa airway colonization in cystic fibrosis. Genes Immun 9:57–60
Valles J, Peredo R, Burgueno MJ, Rodrigues de Freitas AP, Millan S, Espasa M, Martin-Loeches I, Ferrer R, Suarez D, Artigas A (2013) Efficacy of single-dose antibiotic against early-onset pneumonia in comatose patients who are ventilated. Chest 143:1219–1225
Wallace AM, He JQ, Burkett KM, Ruan J, Connett JE, Anthonisen NR, Pare PD, Sandford AJ (2006) Contribution of alpha- and beta-defensins to lung function decline and infection in smokers: an association study. Respir Res 7:76
Wu XM, Gong LY, Lin J, Wang HH (2012) Association between human beta defensin-1 single nucleotide polymorphisms and susceptibility to pulmonary tuberculosis. Chin J Prev Med 46:912–915
Zaga-Clavellina V, Martha RV, Flores-Espinosa P (2012) In vitro secretion profile of pro-inflammatory cytokines IL-1beta, TNF-alpha, IL-6, and of human beta-defensins (HBD)-1, HBD-2, and HBD-3 from human chorioamniotic membranes after selective stimulation with Gardnerella vaginalis. Am J Reprod Immunol 67:34–43
Zhou M, Huang SG, Wan HY, Li M, Rong XJ, Li B (2007a) Genetic polymorphism in human β-defensin-1 and chronic obstructive pulmonary disease in Han Population in South of China. J Shanghai Second Med Univ 19:19–22
Zhou M, Huang SG, Wan HY et al (2007b) Genetic polymorphism in human β-defensin-1 and chronic obstructive pulmonary disease in Han Population in South of China. Med Bull Shanghai Jiaotong Univ 19:19–22
Acknowledgments
We would like to show our thankfulness to the reviewers for their useful comments in this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing interests exist.
Rights and permissions
About this article
Cite this article
Ran, X., Chen, J., Chen, L. et al. Beta-defensin gene (DEFB1) polymorphisms are associated with the susceptibility to chronic respiratory diseases. Genes Genom 38, 645–658 (2016). https://doi.org/10.1007/s13258-016-0388-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13258-016-0388-4










