Abstract
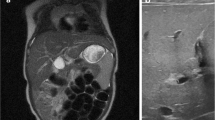
We present the case of a patient with biliary and duodenal atresia who showed false-negative hepatobiliary scintigraphy results. The patient was born at 37 weeks and 2 days of gestation. Her mother had undergone amnioreduction after detection of a double-bubble ultrasound sign in the fetal abdomen. At 2 days of age, total serum bilirubin level was elevated. On hepatobiliary scintigraphy 4 days later, the gallbladder was visualized from 30 min and it showed duodeno-gastric reflux at 240 min. After 24 h, the radiotracer was almost washed out in the hepatic parenchyma, but there was retention in the gastroduodenal junction. Because the biliary to duodenal transit was visible, biliary atresia seemed unlikely. Abdominal ultrasonography at 7 days of age showed a small dysmorphic gallbladder, but triangular cord sign was not definite. Magnetic resonance cholangiography revealed atretic gallbladder. Although cystic and common bile ducts were visible, the proximal common hepatic bile duct was not visible. The next day, serum total bilirubin levels remained elevated (17.1 mg/dl) with direct bilirubin level of 1.2 mg/dl. Kasai portoenterostomy with duodeno-duodenostomy was performed at 10 days of age. Histopathological evaluation showed a fibrous obliteration of the common bile duct, consistent with that of biliary atresia.



Similar content being viewed by others
References
Sokol RJ, Mack C, Narkewicz MR, Karrer FM. Pathogenesis and outcome of biliary atresia: current concepts. J Pediatr Gastroenterol Nutr. 2003;37:4–21.
Wildhaber BE. Biliary atresia: 50 years after the first Kasai. ISRN Surg. 2012;2012:132089.
Hartley JL, Davenport M, Kelly DA. Biliary atresia. Lancet. 2009;374:1704–13.
Wang L, Yang Y, Chen Y, Zhan J. Early differential diagnosis methods of biliary atresia: a meta-analysis. Pediatr Surg Int. 2018;34(4):363–80 1–18.
Kianifar HR, Tehranian S, Shojaei P, Adinehpoor Z, Sadeghi R, Kakhki VRD, et al. Accuracy of hepatobiliary scintigraphy for differentiation of neonatal hepatitis from biliary atresia: systematic review and meta-analysis of the literature. Pediatr Radiol. 2013;43:905–19.
Tulchinsky M, Ciak BW, Delbeke D, et al. SNM practice guideline for hepatobiliary scintigraphy 4.0. J Nucl Med Technol. 2010;38:210–8.
Zhou L, Shan Q, Tian W, Wang Z, Liang J, Xie X. Ultrasound for the diagnosis of biliary atresia: a meta-analysis. AJR Am J Roentgenol. 2016;206:W73–82.
Han SJ, Kim MJ, Han A, Chung KS, Yoon CS, Kim D, et al. Magnetic resonance cholangiography for the diagnosis of biliary atresia. J Pediatr Surg. 2002;37:599–604.
Chavhan GB, Babyn PS, Manson D, Vidarsson L. Pediatric MR cholangiopancreatography: principles, technique, and clinical applications. Radiographics. 2008;28:1951–62.
Kwatra N, Shalaby-Rana E, Narayanan S, Mohan P, Ghelani S, Majd M. Phenobarbital-enhanced hepatobiliary scintigraphy in the diagnosis of biliary atresia: two decades of experience at a tertiary center. Pediatr Radiol. 2013;43:1365–75.
Lee H, Kang J, Kim KM, Jang JY, Jang S-J, Yu E. The clinicopathological parameters for making the differential diagnosis of neonatal cholestasis. Korean J Pathol. 2009;43:43–7.
Van Eyken P, Fanni D, Faa G. Extrahepatic bile duct atresia from the pathologist’s perspective: pathological features and differential diagnosis. J Pediatr Neonatal Individ Med. 2014;3(2):e030247.
Muthukanagarajan SJ, Karnan I, Srinivasan P, Sadagopan P, Manickam S. Diagnostic and prognostic significance of various histopathological features in extrahepatic biliary atresia. J Clin Diagn Res. 2016;10:Ec23–7.
Acknowledgments
The authors would like to thank Enago (www.enago.com) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Hyunji Kim, Sujin Park, Sejin Ha, Jae Seung Kim, Dae Yeon Kim, and Minyoung Oh declare that they have no conflicts of interest.
Ethical Statement
All procedures performed in this study involving human participants were in accordance with the ethical standards of the respective institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent was not required.
Informed Consent
The institutional review board at our institute approved this retrospective study, and the requirement to obtain informed consent was waived.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H., Park, S., Ha, S. et al. False-negative Hepatobiliary Scintigraphy for Biliary Atresia. Nucl Med Mol Imaging 53, 356–360 (2019). https://doi.org/10.1007/s13139-019-00606-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-019-00606-w