Abstract
Background
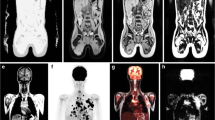
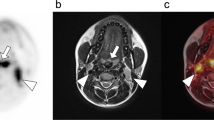
Positron emission tomography/computed tomography (PET/CT) with 2-deoxy-2-[18F]fluoro-D-glucose (FDG) has become the standard of care for the initial staging and subsequent treatment response assessment of many different malignancies. Despite this success, PET/CT is often supplemented by MRI to improve assessment of local tumor invasion and to facilitate detection of lesions in organs with high background FDG uptake. Consequently, PET/MRI has the potential to expand the clinical value of PET examinations by increasing reader certainty and reducing the need for subsequent imaging. This study evaluates the ability of FDG-PET/MRI to clarify findings initially deemed indeterminate on clinical FDG-PET/CT studies.
Methods
A total of 190 oncology patients underwent whole-body PET/CT, immediately followed by PET/MRI utilizing the same FDG administration. Each PET/CT was interpreted by our institution's nuclear medicine service as a standard-of-care clinical examination. Review of these PET/CT reports identified 31 patients (16 %) with indeterminate findings. Two readers evaluated all 31 PET/CT studies, followed by the corresponding PET/MRI studies. A consensus was reached for each case, and changes in interpretation directly resulting from PET/MRI review were recorded. Interpretations were then correlated with follow-up imaging, pathology results, and other diagnostic studies.
Results
In 18 of 31 cases with indeterminate findings on PET/CT, PET/MRI resulted in a more definitive interpretation by facilitating the differentiation of infection/inflammation from malignancy (15/18), the accurate localization of FDG-avid lesions (2/18), and the characterization of incidental non-FDG-avid solid organ lesions (1/18). Explanations for improved reader certainty with PET/MRI included the superior soft tissue contrast of MRI and the ability to assess cellular density with diffusion-weighted imaging. The majority (12/18) of such cases had an appropriate standard of reference; in all 12 cases, the definitive PET/MRI interpretation proved correct. These 12 patients underwent six additional diagnostic studies to clarify the initial indeterminate PET/CT findings. In the remaining 13 of 31 cases with indeterminate findings on both PET/CT and PET/MRI, common reasons for uncertainty included the inability to distinguish reactive from malignant lymphadenopathy (4/13) and local recurrence from treatment effect (2/13).
Conclusions
Indeterminate PET/CT findings can result in equivocal reads and additional diagnostic studies. PET/MRI may reduce the rate of indeterminate findings by facilitating better tumor staging, FDG activity localization, and lesion characterization. In our study, PET/MRI resulted in more definitive imaging interpretations with high accuracy. PET/MRI also showed potential in reducing the number of additional diagnostic studies prompted by PET/CT findings. Our results suggest that whole-body PET/MRI provides certain diagnostic advantages over PET/CT, promotes more definitive imaging interpretations, and may improve the overall clinical utility of PET.



Similar content being viewed by others
Abbreviations
- ADC:
-
apparent diffusion coefficient
- CT:
-
computed tomography
- DWI:
-
diffusion-weighted imaging
- ECO:
-
external cervical os
- FA:
-
flip angle
- FDG:
-
2-deoxy-2-[18F]fluoro-D-glucose
- FOV:
-
field of view
- FS:
-
fat saturation
- HASTE:
-
half-Fourier acquisition single-shot turbo spin echo
- PET:
-
positron emission tomography
- Q-fat sat:
-
quick fat saturation mode
- SPACE:
-
sampling perfection with application of optimized contrasts using different flip angle evolution
- ST:
-
slice thickness
- T1W:
-
T1-weighted
- T2W:
-
T2-weighted
- TE:
-
time to echo
- TR:
-
time to repetition
- TSE:
-
turbo spin echo
- VIBE:
-
volumetric interpolated breath-hold examination
References
Fletcher JW, Djulbegovic B, Soares HP, Siegel B, Lowe VJ, Lyman GH, et al. Recommendations on the use of 18F-FDG PET in oncology. J Nucl Med. 2008;49:480–508.
Coenegrachts K, De Geeter F, ter Beek L, Walgraeve N, Bipat S, Stoker J, et al. Comparison of MRI (including SS SE-EPI and SPIO-enhanced MRI) and FDG-PET/CT for the detection of colorectal liver metastases. Eur Radiol. 2009;19:370–9.
Kitajima K, Suenaga Y, Ueno Y, Kanda T, Maeda T, Deguchi M, et al. Fusion of PET and MRI for staging of uterine cervical cancer: comparison with contrast-enhanced (18)F-FDG PET/CT and pelvic MRI. Clin Imaging. 2014;38:464–9.
Schaarschmidt BM, Grueneisen J, Heusch P, Gomez B, Umutlu L, Ruhlmann V, et al. Does 18F-FDG PET/MRI reduce the number of indeterminate abdominal incidentalomas compared with 18F-FDG PET/CT? Nucl Med Commun. 2015;36:588–95.
Catalano OA, Rosen BR, Sahani DV, Hahn PF, Guimaraes AR, Vangel MG, et al. Clinical impact of PET/MR imaging in patients with cancer undergoing same-day PET/CT: initial experience in 134 patients—a hypothesis-generating exploratory study. Radiology. 2013;269:857–69.
Fowler KJ, McConathy J, Narra VR. Whole-body simultaneous positron emission tomography (PET)-MR: optimization and adaptation of MRI sequences. J Magn Reson Imaging. 2014;39:259–68.
Thoeny HC, De Keyzer F. Extracranial applications of diffusion-weighted magnetic resonance imaging. Eur Radiol. 2007;17:1385–93.
Kanda T, Kitajima K, Suenaga Y, Konishi J, Sasaki R, Morimoto K, et al. Value of retrospective image fusion of 18F-FDG PET and MRI for preoperative staging of head and neck cancer: comparison with PET/CT and contrast-enhanced neck MRI. Eur J Radiol. 2013;82:2005–10.
Kitajima K, Suenaga Y, Ueno Y, Kanda T, Maeda T, Takahashi S, et al. Value of fusion of PET and MRI for staging of endometrial cancer: comparison with 18F-FDG contrast-enhanced PET/CT and dynamic contrast-enhanced pelvic MRI. Eur J Radiol. 2013;82:1672–6.
Kitajima K, Suenaga Y, Ueno Y, Kanda T, Maeda T, Makihara N, et al. Value of fusion of PET and MRI in the detection of intra-pelvic recurrence of gynecological tumor: comparison with 18F-FDG contrast-enhanced PET/CT and pelvic MRI. Ann Nucl Med. 2014;28:25–32.
Eiber M, Takei T, Souvatzoglou M, Mayerhoefer ME, Fürst S, Gaertner FC, et al. Performance of whole-body integrated 18F-FDG PET/MR in comparison to PET/CT for evaluation of malignant bone lesions. J Nucl Med. 2014;55:191–7.
Huellner MW, Barbosa F d. G, Husmann L, Pietsch CM, Mader CE, Burger IA, et al. TNM staging of NSCLC: Comparison of PET/MR and PET/CT. J Nucl Med. 2015.
Lee KH, Park CM, Lee SM, Lee JM, Cho JY, Paeng JC, et al. Pulmonary nodule detection in patients with a primary malignancy using hybrid PET/MRI: is there value in adding contrast-enhanced MR imaging? PLoS One. 2015;10:e0129660.
Reiner CS, Stolzmann P, Husmann L, Burger IA, Hüllner MW, Schaefer NG, et al. Protocol requirements and diagnostic value of PET/MR imaging for liver metastasis detection. Eur J Nucl Med Mol Imaging. 2014;41:649–58.
Van Ufford HMEQ, Kwee TC, Beek FJ, van Leeuwen MS, Takahara T, Fijnheer R, et al. Newly diagnosed lymphoma: initial results with whole-body T1-weighted, STIR, and diffusion-weighted MRI compared with 18F-FDG PET/CT. AJR Am J Roentgenol. 2011;196:662–9.
Ouyang J, Li Q, El Fakhri G. Magnetic resonance-based motion correction for positron emission tomography imaging. Semin Nucl Med. 2013;43:60–7.
Würslin C, Schmidt H, Martirosian P, Brendle C, Boss A, Schwenzer NF, et al. Respiratory motion correction in oncologic PET using T1-weighted MR imaging on a simultaneous whole-body PET/MR system. J Nucl Med. 2013;54:464–71.
Rakheja R, DeMello L, Chandarana H, Glielmi C, Geppert C, Faul D, et al. Comparison of the accuracy of PET/CT and PET/MRI spatial registration of multiple metastatic lesions. AJR Am J Roentgenol. 2013;201:1120–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
TJF – None; KJF – Research Support, Bracco Group; JM – Research Support, Eli Lilly & Co.; Research Consultant, General Electric Healthcare; Research Consultant, Blue Earth Diagnostics Ltd.; Research Consultant, Siemens AG; FD – None
Ethical Statement
The study was approved by an institutional review board or equivalent and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All subjects in the study gave written informed consent or the institutional review board waived the need to obtain informed consent.
Rights and permissions
About this article
Cite this article
Fraum, T.J., Fowler, K.J., McConathy, J. et al. Indeterminate Findings on Oncologic PET/CT: What Difference Does PET/MRI Make?. Nucl Med Mol Imaging 50, 292–299 (2016). https://doi.org/10.1007/s13139-016-0405-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-016-0405-1