Abstract
The incidence of thyroid cancer in females is significantly higher than that in males; however, females are more likely to have more favorable outcomes. We aimed to determine the characteristics of differentiated thyroid carcinoma (DTC) subtypes in males and females, and to compare their clinical behavior and survival. A total of 68,337 cases were recruited from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. The disease-specific survival (DSS) of follicular variant papillary thyroid carcinoma (FVPTC) and follicular thyroid carcinoma (FTC) were similar to that of classical variant papillary thyroid carcinoma (CPTC) in male patients (FVPTC vs. CPTC, adjusted hazard ratio (aHR) = 0.947, P = 0.776; FTC vs. CPTC, aHR = 1.512, P = 0.104). In premenopausal female (< 55 years old), FVPTC had better DSS than CPTC (aHR = 0.321, P = 0.038) while FTC had worse DSS than CPTC (aHR = 3.272, P = 0.013); in postmenopausal female, FTC had poorer prognosis than CPTC (aHR = 2.145, P = 0.002), no statistical difference was found between CPTC and FVPTC (aHR = 0.724, P = 0.087). For patients younger than 55 years, women had significantly better DSS compared with men with CPTC (aHR = 0.376, P < 0.001) and FVPTC (aHR = 0.102, P < 0.001). However, no difference was observed in patients older than 55 years. Interestingly, outcomes of FTC were not affected by gender in patients of all ages. These results suggested that different clinical behaviors and outcomes of DTC subtypes should be considered in patients with different genders.
Similar content being viewed by others
Introduction
The incidence of thyroid cancer has increased by 211% over the past three decades [1]. Well-differentiated thyroid carcinoma (DTC) is the most common carcinoma of the malignant thyroid cancer, accounting approximately 90% of all the cases [2]. Based on the predominant histologic pattern, DTC is subdivided into follicular thyroid carcinoma (FTC) and papillary thyroid carcinoma (PTC) [3]. PTC is the most frequent type of DTC and is generally considered as an indolent tumor with excellent prognosis. Among the numerous PTC variants, classical variant papillary thyroid carcinoma (CPTC) constitutes half of the cases, and follicular variant papillary thyroid carcinoma (FVPTC) constitutes 9 to 22.5% of the cases [4]. A more recent study demonstrated that FVPTC accounted for up to 41% of all PTC [5]. Despite the favorable prognosis of DTC, PTC, and FTC have distinct clinical behaviors and outcomes. Mounting studies demonstrated that FTC had a poorer prognosis [6,7,8]. FTC is considered more aggressive mainly due to its ability of metastases via vascular invasion, especially distant metastasis [9], while some of the studies failed to find the survival difference between PTC and FTC [10]. Since FVPTC has a pathological appearance similar to follicular-patterned tumor and a nuclear appearance similar to CPTC, it has been speculated to possess both CPTC and FTC features. FVPTC was historically been considered as more aggressive than CPTC, while many studies found no significant difference in the clinical outcomes of these two subtypes [11, 12]. Inversely, other studies reported that FVPTC had less aggressive clinical behavior and similar or even better survival than CPTC [2, 5, 13].
It has long been acknowledged that the incidence of thyroid cancer in women is significantly higher than that in men. Thyroid cancer occurs over twofold higher in female compared to male [14]. The discrepancy of incidence suggests female gender as a possible epidemiologic risk factor [15]. However, women usually have more favorable DTC outcomes than men [16]. Several hypotheses have been proposed to explain the disparities between male and female patients with thyroid cancer: differential screening, gender-specific behavioral differences and biological sex differences [17]. Previous studies demonstrated that sex steroids might modulate normal or pathological thyroid growth and had different roles in the development of thyroid cancer depending on tumor histology [18,19,20]. In addition, expression of sex steroid receptors was also found to be different in tumor and normal tissue, and it was comparable between men and women [21].
The histopathological disparities between male and female have been well demonstrated in many reported series [15, 17, 22, 23]. However, whether the three subtypes of DTC have different clinical behaviors and outcomes in the same gender is unclear. To further investigate the association between gender and DTC, we conducted a retrospective analysis using data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. The purpose of this study was to determine the characteristics of CPTC, FVPTC, and FTC in males and females, and to compare their clinical behavior and survival.
Methods
Data Source and Study Design
We performed this retrospective cohort analysis using data from SEER database which was designed and maintained by National Cancer Institute (the USA). All patients diagnosed with CPTC, FVPTC, or FTC diagnosed between 2004 and 2014 were identified using histopathology codes of the International Classification of Disease for Oncology, third edition (ICD-O-3). Histology codes were listed below to select patients of each subtype accordingly.
CPTC included 8050 (papillary carcinoma not otherwise specified, NOS), 8260 (papillary adenocarcinoma, NOS), and 8343 (papillary carcinoma, encapsulated); FVPTC: 8340 (papillary carcinoma, follicular variant); and FTC included 8330 (follicular adenocarcinoma, NOS), 8331 (follicular adenocarcinoma well differentiated), 8332 (follicular adenocarcinoma trabecular), and 8335 (follicular carcinoma, minimal invasive).
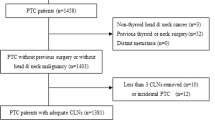
Exclusion criteria for this study included (1) age younger than 18 years, (2) tumor size, tumor extension, lymph node metastasis, or distant metastasis information were unknown; (3) removal of lymph node number was unknown. Patients underwent total thyroidectomy with or without postoperative radioactive iodine were eligible for our further analysis (Supplementary 1).
Our analysis included demographic variables: sex (male and female), age at diagnosis (< 45 and ≥ 45 years), race (white, black, other, and unknown). Cancer characteristics were classified included tumor size (less than 1 cm, 1.1 to 2 cm, 2.1 to 4 cm, and larger than 4 cm. These sizes were chosen based on American Joint Committee on Cancer T staging); tumor extension: intrathyroidal extension (codes 100, 200, 300, 400), minimal extrathyroidal extension (code 450) and gross extrathyroidal extension (codes 480, 500, 520, 550, 600, 620, 650, 700, 730, 800); lymph node metastasis (code 000: no lymph node metastasis, code 120: metastasis to level VI, codes 135, 155, 158, 160: metastasis to levels I, II, III, IV, V, or VII); and distant metastasis (code 00: no distant metastasis; code 12, 40, 51, 60: distant metastasis disease). Treatment characteristics included surgery therapy (code 50: total thyroidectomy); receipt of radiation therapy (none and radioactive iodine); lymph node surgery (none, 1 to 3 regional lymph nodes removed, 4 or more regional lymph nodes removed). All the variables were defined using the SEER specific codes.
Overall survival (OS) and disease-specific survival (DSS) were two main outcomes in our study; they were obtained using multivariate Cox proportional hazard regressions. Vital status was recorded as “alive” or “dead” in the SEER dataset. Survival time (in months) was calculated for each patient using the “Completed Months of Follow-up” given in the SEER database.
Statistical Analysis
Patient demographics, as well as cancer- and treatment-related characteristics, were compared between histological subgroups in both genders using chi-square or Fisher’s exact tests. For multivariate analysis, Cox proportional hazards regression were used to assess the association between histological subtype and probability of survival in both genders. HRs with their respective 95% confidence intervals were obtained to understand strength of the relative risk of histological subtype in different genders. Any HR > 1.0 showed an increased risk of death. P value < 0.05 was considered statistically significant and all tests were two sided.
Results
Patient Characteristics of Male
Based on the inclusion criteria, this study included a total of 68,337 patients diagnosed with CPTC, FVPTC, and FTC between 2004 and 2014. Among them, 15,247 (22.3%) were male and 53,090 (77.7%) were female. Of the total death of 2736, 422 patients died from thyroid cancer.
Among the total of 15,247 male patients, 9773 were diagnosed with CPTC, 4489 were diagnosed with FVPTC, and only 985 were diagnosed with FTC. The demographics and clinicopathologic features of the three histologic subgroups were compared in Table 1. FVPTC and FTC, rather than CPTC, were diagnosed more often in patients older than 45 years. The tumor size of CPTC and FVPTC were similar, while nearly half of FTC were larger than 4 cm. Extrathyroidal extension were more common in FVPTC (14.9%) than in FTC (10.9%), but less common than in CPTC (25.2%). Lymph node metastasis occurred more frequently in CPTC (38%) and FVPTC (17.2%), while it appeared rarely in FTC (3.7%). However, distant metastasis was more commonly observed in FTC (2.9%) than in CPTC (1.4%) and FVPTC (1.7%). Among the 183 patients died from thyroid cancer, 119 were CPTC, 41 were FVPTC, and 23 were FTC.
Patient Characteristics of Female
A total of 53,090 female patients were diagnosed with DTC, with 33,628 CPTC, 16941 FVPTC, and 2521 FTC cases. The demographics and cancer characteristics of the three histologic subgroups are compared in Table 2. FVPTC and FTC patients were more frequently diagnosed older than 45 years than CPTC. The size of CPTC and FVPTC were usually smaller than 2 cm, while FTC were more often diagnosed with tumor size between 2 and 4 cm. Extrathyroidal extension occurred more frequently in CPTC (18.8%) and PTC (11.5%) than that in FTC (7.4%). Lymph node metastasis was more common in CPTC (24.6%) compared with FVPTC (10.7%), while only 2% of FTC had lymph node metastasis. Distant metastasis was more rarely diagnosed in female with CPTC (0.4%) and FVPTC (0.6%) compared to FTC (2.6%).
Overall Survival and Disease-Specific Survival in Male and Female
OS of the three subtypes in males were comparable (Fig. 1a). Despite the DSS between FTC and CPTC were comparable, there was no statistical significance (aHR = 1.512, P = 0.104). DSS of FVPTC was similar to that for CPTC (aHR = 0.947, P = 0.776) (Fig. 1b, Supplementary 2). There was also no significant difference of OS among the three types of DTC in females (Fig. 1c). Interestingly, the DSS of FVPTC was better than that of CPTC (aHR = 0.678, P = 0.029). FTC patients had a significantly poorer DSS (aHR = 2.157, P < 0.001) compared with CPTC (Fig. 1d, Supplementary 2).
Overall survival (OS) and disease-specific survival (DSS) curves of multivariate Cox analysis. a OS is based on histologic type in male. b DSS is based on histologic type in male. c OS is based on histologic type in female. d DSS is based on histologic type in female. P values calculated by multivariate Cox analysis. aHR adjusted hazard ratio (adjusted for age at diagnosis, race, tumor size, tumor extension, lymph nodes metastases, distant metastases, radiotherapy, removal of lymph node number)
Gender Disparity in Disease-Specific Survival in Patients Stratified by Age of 55 Years
The female reproductive hormones affect the clinical behaviors of DTC, so the age of menopause should be considered. Since 90 to 95% of women reached menopause at the age of 55 years in the USA [24], patients were further stratified by the age of 55. In females younger than 55, DSS were significantly different among the three histologic subtypes. FVPTC patients had better DSS than that of CPTC (aHR = 0.321, P = 0.038), and DSS of FTC was significantly poorer than CPTC (aHR = 3.272, P = 0.013). In females older than 55, the histologic subtype of CPTC and FVPTC had no significant difference in DSS (aHR = 0.724, P = 0.087), while the FTC patients had significantly worse DSS than the CPTC patients (aHR = 2.145, P = 0.002) (Fig. 2a, b). DSS of FVPTC and FTC were similar to that of CPTC in males at all ages (Fig. 2c, d).
DSS curves of multivariate Cox analysis in female. a. DSS is based on histologic type in premenopausal females. b DSS is based on histologic type in postmenopausal females. c DSS is based on histologic type in males younger than 55 years. d DSS is based on histologic type in males older than 55 years. P values calculated by multivariate Cox analysis. aHR adjusted hazard ratio (adjusted for race, tumor size, tumor extension, lymph nodes metastases, distant metastases, radiotherapy, removal of lymph node number)
For patients younger than 55, DSS of CPTC was better in females than that in males (aHR = 0.376, P < 0.001), while for patients with CPTC older than 55, DSS of both genders were comparable (aHR = 1.004, P = 0.976). The same result was also observed in FVPTC. However, for FTC patients, multivariate analysis demonstrated no statistical difference between genders either in patients at all ages (Fig. 3).
DSS curves of different differentiated thyroid carcinoma (DTC) types of multivariate Cox analysis. a DSS of classical variant papillary thyroid carcinoma (CPTC) is based on both genders younger than 55 years. b DSS of CPTC is based on both genders older than 55 years. c DSS of follicular variant papillary thyroid carcinoma (FVPTC) is based on both genders younger than 55 years. d DSS of FVPTC is based on both genders older than 55 years. e DSS of follicular thyroid carcinoma (FTC) is based on both genders younger than 55 years. f DSS of FTC is based on both genders older than 55 years. P values calculated by multivariate Cox analysis. aHR adjusted hazard ratio (adjusted for race, tumor size, tumor extension, lymph nodes metastases, distant metastases, radiotherapy, removal of lymph node number)
Discussion
The disparities of thyroid cancer between genders have been well-documented [23]. Women were believed to have a higher incidence of thyroid cancer than men; however, men appeared to have worse clinical outcomes [22]. In our current study, we compared the three types of DTC in both genders. Our analysis revealed some novel phenomenon about gender differences in DTC. First, CPTC, FVPTC, and FTC had similar outcomes in male patients. In premenopausal female, these three subtypes had significantly different outcomes; while in postmenopausal female, FTC had poorer prognosis than CPTC, no significant difference was observed between CPTC and FVPTC. Second, for patients younger than 55 years old, women had significantly better DSS compared with men with CPTC and FVPTC, while there was no difference in patients older than 55 years old. Interestingly, outcomes of FTC were not affected by gender.
Previous evidence indicated gender as a prognostic factor. Mitchell et al. performed a retrospective analysis based on SEER database and National Hospital Discharge Survey database between 1974 and 2000, and found that mortality rate for men was twofold higher than women [25]. A long-term follow-up prospective study by Mazzaferri et al. suggested male gender as an independently risk factor for thyroid cancer survival [26], which was consistent with previous reports [27,28,29]. In our study, we found similar results in CPTC and FVPTC patients younger than 55 years, while no statistical difference was revealed when patients older than 55 years. Multivariate analysis of FTC demonstrated no significant difference between genders. The possible impacts included differential screening, gender-specific behavioral differences, and biological sex difference [17]. Females are more likely to be screened by physicians for clinically unrecognized thyroid disease. In our study, genders had no effect on DSS for patients with CPTC and FVPTC older than 55 years and patients with FTC. These results discounted the major effect of differential screening on the disparities between male and female. Gender-specific behavioral differences are characterized by the greater tendency of women to seek medical attention than men. In our study, all patients underwent total thyroidectomy, and women were more likely to continue their follow-ups and maintain contact to their physicians. Even though the incidence of thyroid cancer is higher in females, thyroid cancers behaved more aggressively in men than women [17, 23]. It is possible that PTC cases have a worse prognosis in an estrogen-deficient environment than exposed to female hormones [22]. The influences of sex steroids on thyroid have been extensively studied. Sex steroids have different roles in the development of thyroid cancer depending on tumor histology [18,19,20]. It was reported that estrogen might have some protective effects on thyroid cancer, but definitive mechanism was lacking [30]. Experimental studies demonstrated a promoting effect of testosterone on thyroid tumor and a protective effect of estradiol on thyroid carcinoma development in rats [31]. Expression of AR was found to be upregulated in male patients. Moreover, AR mRNA expression was increased in the thyroid gland of men while decreased in women except those with FTC [32, 33]. Another study stated that PTC, rather than FTC, patients were more often diagnosed as ER positive [34]. These findings provided potential explanations for the phenomenon that DSS of CPTC and FVPTC were better in premenopausal female than male, while DSS of FTC had no significant difference in both genders.
Another observation in our study was the different outcomes of DTC subtypes in both genders. DSS for FVPTC, CPTC, and FTC were very similar in males older than 55; while no significant difference was observed in males younger than 55. Although CPTC, FVPTC, and FTC had distinct outcomes in premenopausal females, no statistical difference was found between CPTC and FVPTC in postmenopausal females, and FTC patients had significantly worse DSS in females. These might also due to the levels of sex steroids and the different expressions of their receptors. ER positive was more likely to be detected in PTC rather than FTC [34], thus in premenopausal female, CPTC and FVPTC had better DSS than FTC. The difference between CPTC and FVPTC in females might result from the discrepant expressions of ER in the tumor. Therefore, FVPTC had better DSS in premenopausal females, and males and postmenopausal females had no significant difference between CPTC and FVPTC. The protein levels of AR were increased in male patients with PTC and FTC, but downregulated in PTC and upregulated in FTC females [34]. Thus, FTC had worse DSS in female than CPTC and FVPTC, but not in males.
Besides the classical histological separation of classical PTC and FVPTC, a study of genomic characterization discovered three somatic mutation-based PTC subtypes, which were strongly associated with histologic subtype, lymph node status, extrathyroidal extension, stage and risk of recurrence. BRAFV600E and mutated RAS are mutually exclusive and drivers with distinct signaling consequence: Tumors driven by BRAFV600E has high MAPK signaling while tumors driven by RAS mutation have lower MAPK signaling. BRAFV600E-like (BVL) PTCs represent a diverse group of tumors and result in predominantly less-differentiated tumors enriched for classical and tall cell histology, while RAS-like (RL) PTCs result in highly differentiated tumors enriched for follicular histology with relatively low risk of recurrence [35].
There were several limitations in the presented study. Because of the indolent nature of DTC, it was difficult to study with large, prospective trials, and the database was potentially biased by prejudice and treatment practices. In addition, SEER database did not capture the information on recurrence records. Due to the rare specific mortality of DTC, currently, recurrence is believed to be more meaningful than death. And some other histological subtypes of PTC, such as tall cell variant which was not clearly coded in the database, were not included in our analysis. Based on the novel 2017 WHO Classification, non-invasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) was introduced to be a new subset of FVPTC [36]. In our study, NIFTP cannot be distinguished from other subtypes of FVPTC due to the limitation of SEER database. NIFTP presents extremely low recurrence or metastatic potential, while the clinical behaviors and outcomes of NIFTP between genders need further investigation. Since the information of tumor differentiation is not complete in SEER, another drawback for the study is that some PDTCs may be combined into our analysis. 2017 WHO Classification for PDTC used the proposal of Turin criteria which included (1) the presence of a solid/trabecular/insular pattern of growth, (2) the absence of the conventional nuclear features of papillary carcinoma, and (3) the presence of at least one of the following features: convoluted nuclei, mitotic activity ≥ 3 per 10 high-power fields, and tumor necrosis [36, 37]. Although it is possible that genetic variation between genders makes contribution to gender disparities, we could not comprehensively study genetic differences with this database. Lots of confounding factors associated with gender were not considered in our study: alcohol consumption, smoking, education level, income, use of health care and marital status. These factors contributed gender disparities as well.
In the previous studies, FVPTC was not separated from PTC. Some studies compared the clinical behavior and outcomes of DTC in the whole population, and the age of menopause was not considered. In our study, CPTC, FVPTC, and FTC had distinct clinical behaviors and outcomes in premenopausal females. DSS of FVPTC was similar to that of CPTC in postmenopausal females, while FTC patients had significantly worse DSS than CPTC. In males, no significant difference was observed among the three types. For patients younger than 55, women had significantly better DSS compared with men with CPTC or FVPTC, while difference was not found in patients older than 55. Outcomes of FTC were not affected by genders in patients at all ages. These results suggested the different clinical behaviors and outcomes of DTC subtypes between genders. Our findings were consistent with previously reported role of sex hormones in thyroid cancer. Thereby, different treatment strategy should be designed for male and female patients.
References
Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM (2017) Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA 317(13):1338–1348
Zidan J, Karen D, Stein M, Rosenblatt E, Basher W, Kuten A (2003) Pure versus follicular variant of papillary thyroid carcinoma: clinical features, prognostic factors, treatment, and survival. Cancer 97(5):1181–1185
Jossart GH, Clark OH, Jossart GH, Clark OH (1995) Well-differentiated thyroid cancer. Curr Probl Surg 31(12):933–1012
Yu XM, Schneider DF, Leverson G, Chen H, Sippel RS (2013) Follicular variant of papillary thyroid carcinoma is a unique clinical entity: a population-based study of 10,740 cases. Thyroid 23(10):1263–1268
Lang BH, Lo CY, Chan WF, Lam AK, Wan KY (2006) Classical and follicular variant of papillary thyroid carcinoma: a comparative study on clinicopathologic features and long-term outcome. World J Surg 30(5):752–758
Riesco-Eizaguirre G, Santisteban P (2007) New insights in thyroid follicular cell biology and its impact in thyroid cancer therapy. Endocr Relat Cancer 14(4):957–977
Ito Y, Miyauchi A (2009) Prognostic factors and therapeutic strategies for differentiated carcinomas of the thyroid. Endocr J 56(2):177–192
Sciuto R, Romano L, Rea S, Marandino F, Sperduti I, Maini CL (2009) Natural history and clinical outcome of differentiated thyroid carcinoma: a retrospective analysis of 1503 patients treated at a single institution. Ann Oncol 20(10):1728–1735
Aschebrook-Kilfoy B, Grogan RH, Ward MH, Kaplan E, Devesa SS (2013) Follicular thyroid cancer incidence patterns in the United States, 1980-2009. Thyroid 23(8):1015–1021
Elisei R, Molinaro E, Agate L, Bottici V, Masserini L, Ceccarelli C, Lippi F, Grasso L, Basolo F, Bevilacqua G, Miccoli P, Di Coscio G, Vitti P, Pacini F, Pinchera A (2010) Are the clinical and pathological features of differentiated thyroid carcinoma really changed over the last 35 years? Study on 4187 patients from a single Italian institution to answer this question. J Clin Endocrinol Metab 95(4):1516–1527
Carcangiu ML, Zampi G, Pupi A, Castagnoli A, Rosai J (1985) Papillary carcinoma of the thyroid. A clinicopathologic study of 241 cases treated at the University of Florence, Italy. Cancer 55(4):805–828
LiVolsi VA, Asa SL (1994) The demise of follicular carcinoma of the thyroid gland. Thyroid 4(2):233–236
Tielens ET, Sherman SI, Hruban RH, Ladenson PW (1994) Follicular variant of papillary thyroid carcinoma. A clinicopathologic study. Cancer 73(2):424–431
Schonfeld SJ, Neta G, Sturgis EM, Pfeiffer RM, Hutchinson AA, Xu L, Wheeler W, Guenel P, Rajaraman P, de Vathaire F, Ron E, Tucker MA, Chanock SJ, Sigurdson AJ, Brenner AV (2012) Common genetic variants in sex hormone pathway genes and papillary thyroid cancer risk. Thyroid 22(2):151–156
Yao R, Chiu CG, Strugnell SS, Gill S, Wiseman SM (2014) Gender differences in thyroid cancer: a critical review. Expert Rev Endocrinol Metab 6(2):215–243
Brierley JD, Panzarella T, Tsang RW, Gospodarowicz MK, O’Sullivan B (1997) A comparison of different staging systems predictability of patient outcome. Thyroid carcinoma as an example. Cancer 79(12):2414–2423
Machens A, Hauptmann S, Dralle H (2006) Disparities between male and female patients with thyroid cancers: sex difference or gender divide? Clin Endocrinol 65(4):500–505
Zeng Q, Chen GG, Vlantis AC, van Hasselt CA (2007) Oestrogen mediates the growth of human thyroid carcinoma cells via an oestrogen receptor-ERK pathway. Cell Prolif 40(6):921–935
Banu KS, Govindarajulu P, Aruldhas MM (2001) Testosterone and estradiol have specific differential modulatory effect on the proliferation of human thyroid papillary and follicular carcinoma cell lines independent of TSH action. Endocr Pathol 12(3):315–327
Lee ML, Chen GG, Vlantis AC, Tse GM, Leung BC, van Hasselt CA (2005) Induction of thyroid papillary carcinoma cell proliferation by estrogen is associated with an altered expression of Bcl-xL. Cancer J 11(2):113–121
Hampl R, Nemec J, Heresova J, Kimlova I, Starka L (1985) Estrogen receptors in human goitrous and neoplastic thyroid. Endocrinol Exp 19(4):227–230
Jonklaas J, Nogueras-Gonzalez G, Munsell M, Litofsky D, Ain KB, Bigos ST, Brierley JD, Cooper DS, Haugen BR, Ladenson PW, Magner J, Robbins J, Ross DS, Skarulis MC, Steward DL, Maxon HR et al (2012) The impact of age and gender on papillary thyroid cancer survival. J Clin Endocrinol Metab 97(6):E878–E887
Rahbari R, Zhang L, Kebebew E (2010) Thyroid cancer gender disparity. Future Oncol 6(11):1771–1779
Weinstein M, Gorrindo T, Riley A, Mormino J, Niedfeldt J, Singer B, Rodriguez G, Simon J, Pincus S (2003) Timing of menopause and patterns of menstrual bleeding. Am J Epidemiol 158(8):782–791
Mitchell I, Livingston EH, Chang AY, Holt S, Snyder WH 3rd, Lingvay I, Nwariaku FE (2007) Trends in thyroid cancer demographics and surgical therapy in the United States. Surgery 142(6):823–828 discussion 828 e821
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97(5):418–428
Cunningham MP, Duda RB, Recant W, Chmiel JS, Sylvester JA, Fremgen A (1990) Survival discriminants for differentiated thyroid cancer. Am J Surg 160(4):344–347
Byar DP, Green SB, Dor P, Williams ED, Colon J, van Gilse HA, Mayer M, Sylvester RJ, van Glabbeke M (1979) A prognostic index for thyroid carcinoma. A study of the E.O.R.T.C. Thyroid Cancer Cooperative Group. Eur J Cancer 15(8):1033–1041
Lundgren CI, Hall P, Ekbom A, Frisell J, Zedenius J, Dickman PW (2003) Incidence and survival of Swedish patients with differentiated thyroid cancer. Int J Cancer 106(4):569–573
Rajoria S, Suriano R, George AL, Shanmugam A, Jussim C, Shin EJ, Moscatello AL, Geliebter J, Carpi A, Tiwari RK (2012) Estrogen activity as a preventive and therapeutic target in thyroid cancer. Biomed Pharmacother 66(2):151–158
M.M. AT Aruldhas, S.K. Banu, P. Govindarajulu. Thyroidal concentration of testosterone and estradiol determines the promotion of thyroid tumours in N-nitrosodiisopropanolamine (DHPN) treated Wistar rats in: 12th Asia Pacific Cancer Conference: Towards Total Cancer Control,Singapore :p 43
Stanley JA, Aruldhas MM, Chandrasekaran M, Neelamohan R, Suthagar E, Annapoorna K, Sharmila S, Jayakumar J, Jayaraman G, Srinivasan N, Banu SK (2012) Androgen receptor expression in human thyroid cancer tissues: a potential mechanism underlying the gender bias in the incidence of thyroid cancers. J Steroid Biochem Mol Biol 130(1–2):105–124
Zhai QH, Ruebel K, Thompson GB, Lloyd RV (2003) Androgen receptor expression in C-cells and in medullary thyroid carcinoma. Endocr Pathol 14(2):159–165
Dianbin Mu ZL, Yan A (1997) Detection and analysis of estrogen and progesterone receptors in thyroid tumors. Cancer Res Clin:101–102
(2014) Integrated genomic characterization of papillary thyroid carcinoma. Cell 159(3):676–690
Lloyd RV, Osamura RY, Kloppel G, Rosai J (2017) WHO classification of tumours of the endocrine organs, 4th edn. International Agency for Research on Cancer, Lyon
Burman KDI (2014) Poorly differentiated thyroid cancer poorly characterized? J Clin Endocrinol Metab 99(4):1167–1169
Acknowledgements
We thanked Qi Wu for assistance in improving the quality of language and revising the statistical method.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, D., Tang, J., Kong, D. et al. Impact of Gender and Age on the Prognosis of Differentiated Thyroid Carcinoma: a Retrospective Analysis Based on SEER. HORM CANC 9, 361–370 (2018). https://doi.org/10.1007/s12672-018-0340-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-018-0340-y