Abstract
Early prospective studies suggested circulating insulin-like growth factor (IGF)-I was positively associated with risk of premenopausal, but not postmenopausal, breast cancer; however, a recent, large analysis reported a statistically significant positive association with postmenopausal disease. Therefore, we conducted a large study nested within the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial cohort to assess the association between circulating IGF-I and IGF binding protein (IGFBP)-3 levels and subsequent postmenopausal breast cancer risk. We included 389 breast cancer cases and 470 controls, aged 55-74, not using exogenous hormones at blood draw, and matched by age at and date of serum collection. Mean follow-up was 8.5 years; mean time between serum collection and diagnosis was 4.0 years. We used Cox proportional hazards regression models to obtain hazard ratios (HRs) and 95% confidence intervals (95% CIs). Multivariate HRs for IGF-I, IGFBP-3, and the molar ratio IGF-I/IGFBP-3, comparing the highest quintile to the lowest, were 1.28 (95% CI, 0.67-2.44), 1.12 (95% 0.55-2.27), and 1.25 (95% 0.72–2.15), respectively. Multivariate HRs per one quintile increase were 1.07 (95% 0.92–1.25) for IGF-I, 1.01 (95% 0.86–1.18) for IGFBP-3, and 1.10 (95% 0.98–1.24) for the molar ratio. These models included accepted breast cancer risk factors and height, along with baseline BMI and serum estradiol, both of which increased the risk associated with IGF-I and the molar ratio. IGF-I and the IGF-I/IGFBP-3 molar ratio were positively, although not statistically significantly, associated with postmenopausal breast cancer risk. Further research should emphasize larger studies, including pooled analyses, analyses by cancer subtype, improved exposure assessment, and possible mechanisms.
Similar content being viewed by others
Introduction
Insulin-like growth factor (IGF)-I is a polypeptide hormone hypothesized to play a role in breast carcinogenesis through stimulating mitosis and inhibiting apoptosis in normal and malignant breast epithelial cells [1, 2]. IGF binding protein-3 (IGFBP-3), the major binding protein for IGF-I, regulates IGF-I action, but may also have an independent effect on breast carcinogenesis through limiting the proliferation of breast epithelial cells [2].
Early prospective studies suggested that high circulating levels of IGF-I might be positively associated with subsequent breast cancer risk in premenopausal women [3]. A recent meta-analysis of prospective studies found that the positive association between IGF-I and premenopausal breast cancer risk was attenuated in more recent publications, although overall it remained positive and statistically significant [4].
The majority of cohort studies [3, 5–9] and several meta-analyses [10–12] have not shown statistically significant associations between prediagnostic circulating IGF-I levels and postmenopausal breast cancer risk. Several of these studies have been relatively large, with 835 [5], 514 [7], 411 [8], and 305 [3] postmenopausal breast cancer cases. However, the second largest study to date, with 614 breast cancer cases diagnosed after 50 years of age [13], reported a statistically significant positive association; and other studies have suggested positive associations overall [14] or in various subgroups of postmenopausal women [15, 16].
With one exception [8], studies that found no statistically significant association with circulating IGF-I also found no statistically significant association with IGFBP-3 [3, 5, 7]; and the study that did find a statistically significant positive association with IGF-I also reported a statistically significant positive association with IGFBP-3 [13].
Given the strong biologic rationale for a role for the IGF pathway in breast carcinogenesis and the inconsistent results from the epidemiologic studies, we investigated the relationships between circulating IGF-I and IGFBP-3 levels and subsequent postmenopausal breast cancer risk in a study nested within the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO) cohort. With a total of 389 incident breast cancer cases, it is among the larger studies among postmenopausal women to address this issue.
Materials and Methods
Study Design and Population
Study subjects were participants in the PLCO, a multi-site randomized intervention trial designed to evaluate the efficacy of screening for prostate, lung, colorectal, and ovarian cancers. Females and males, aged 55-74 at study entry, were randomized into one of two arms: a control arm in which patients received their regular care from their personal physicians and an intervention arm in which women were screened for colorectal, lung, and ovarian cancer and men were screened for colorectal, lung, and prostate cancer. Subjects were recruited between November 1993 and July 2001 in ten centers throughout the USA. Potential participants were excluded from the trial if they had a history of one of the four PLCO cancers, had a recent history of screening procedures for one of the cancers, or were undergoing treatment for any cancer. Details of the study have been published elsewhere [17, 18].
Demographic, medical history, health-related behavior, and dietary information were obtained through baseline questionnaires completed by study participants at or around the time of randomization. Blood was collected from subjects randomized to the screening arm on the morning of the cancer screening exams.
Breast and other cancers were primarily identified through annual study update questionnaires sent to the participants that ascertained type and date of any cancer diagnosis in the previous year. Confirmation of these self-reported cancer diagnoses was sought from study hospitals and usually obtained within 2 years of self-report. Cancers were also identified through annual linkage to the National Death Index, State Cancer Registries, physician reports, and next-of-kin reports. Active follow-up of study participants is still ongoing. As of June 30, 2005, 9.6% of the women without breast cancer in the intervention arm of the trial were censored due to death or non-response.
Study subjects provided written informed consent. The study was approved by the Institutional Review Boards of the National Cancer Institute and the ten participating sites.
Study Sample
For the initial studies of biochemical and genetic biomarkers and breast cancer incidence, a study sample was selected from the 39,115 women randomized to the intervention arm of the trial (Table 1). A total of 1,141 women who had completed a baseline questionnaire and at least one annual study update form, provided a blood sample at baseline, reported no history of breast cancer prior to randomization into the study, and signed a consent form for biomarker studies were identified with incident breast cancer through June 30, 2005. A total of 1,141 controls meeting the same eligibility criteria were selected by randomly sampling women who had not been diagnosed with breast cancer by June 30, 2005 and were frequency matched to cases in eight strata defined by age at randomization (55-59, 60-64, 65-69, and 70-74) and date of blood collection (before or after September 30, 1997, the median date of baseline blood collection).
Subsequent to the selection of controls, additional exclusion criteria were applied to both cases and controls to arrive at the analytic file for the current analysis (Table 1). Cases and controls had to have at least two vials of serum drawn at study entry, be postmenopausal and not currently using menopausal hormone therapy at the time of the blood draw, and have assay results for serum IGF-I and IGFBP-3. A total of 389 breast cancer cases and 470 controls met all eligibility criteria.
All breast cancer cases except one had ICD-O-2 codes of C500-C509 on hospital pathology reports; 308 cases (79%) were invasive and 80 in situ (21%). Estrogen receptor (ER) status was available for 267 of the breast cancer cases (78%); 222 of those with known ER status (83%) were ER positive and 45 (17%) were ER negative. A total of 293 breast cancer cases (75%) were ductal (ICD-O codes 8500 and 8521), 57 (15%) were lobular (ICD-O codes 8520 and 8522), and 39 (19%) were other or unknown histologies (ICD-O codes 8140, 8141, 8201, 8211, 8480, 8501, 8503, and 8510).
IGF-I and IGFBP-3 Measurement
Serum levels of IGF-I and IGFBP-3 were assayed in 2006 by enzyme-linked immunosorbent assay with reagents from Diagnostic Systems Laboratory (Webster, TX, USA) at the Lady Davis Research Institute of the Jewish General Hospital and McGill University, Montreal, Quebec, Canada. For each analyte, samples from the study subjects were randomly assigned to batches of 74 samples, with approximately equal numbers of cases and controls in each batch. Replicate IGF-I and IGFBP-3 measurements for each sample were averaged. In addition, two aliquots from two of four quality control samples were inserted randomly in each batch. Laboratory personnel were unable to distinguish among case, control, and quality-control specimens. The total coefficients of variation for the assays for IGF-I and IGFBP-3 were 5.1% and 4.8%, respectively, based on a nested components of variance analysis with logarithmically transformed measurements of the quality control samples [19].
The molar ratio of IGF-I/IGFBP-3 was calculated as 0.130 × IGF-I concentration in nanogram per milliliter)/0.036 × IGFBP-3 concentration in nanogram per milliliter [20].
Unconjugated Estradiol Measurement
Unconjugated estradiol was measured in serum by liquid chromatography-tandem mass spectrometry (LC-MS/MS) [21]. Unconjugated estradiol was measured in serum by LC-MS/MS. Initially, an internal standard solution, including unconjugated 13C-estradiol, was added to 0.5 mL of serum. Glucuronide and sulfate residues were not enzymatically hydrolyzed. Unconjugated estradiol was extracted with dichloromethane. Estradiol and 13C-estradiol were quantitatively dansylated with dansyl chloride to improve ionization efficiency. The lower level of quantitation was 8 pg estradiol/mL serum (29.4 fmol/mL). Assay precision, including intrabatch and interbatch variation, was <5%; it was based on blinded quality control samples undergoing all preparation steps, including extraction and derivatization. Valid estradiol values were available for 445 controls and 369 cases that otherwise met the study inclusion criteria.
Statistical Analysis
Software for the Statistical Analysis of Correlated Data (SUDAAN Release 9.0.0), a family of statistical procedures for analysis of weighted data, was used for the statistical analysis. Cox proportional hazards regression models with age during the follow-up period as the time metric were used to calculate hazard rate ratios (HR) and 95% confidence intervals (CI). In a case-cohort type design, sampling weights of one for the cases and the inverse of the sampling fractions in the eight strata for the non-cases were used in the regression models. The full sample of 1,141 cases and 1,141 controls was processed using the “subpopn” statement to limit the dataset to the analytic file of 389 breast cancer cases and 470 controls. This approach, by using in the calculations the sampling information for observations not included in the subpopulation, ensured that standard errors were calculated correctly.
Median values were assigned for missing values for variables with very few missing values: age at first menarche (N = 1), height (N = 3), number of live births (N = 3), and age at first childbirth (N = 3). The three study subjects with missing values for family history of breast cancer were assigned to “No family history”. An “unknown category” was created for the following variables with more numerous missing values: body mass index (BMI) in kilogram per square meter, unconjugated estradiol, history of benign breast disease, age at menopause, type of menopause, and alcohol consumption.
Geometric mean levels of IGF-I and IGFBP-3 were examined according to levels of breast cancer risk factors (race, family history of breast cancer, personal history of benign breast disease, and type of menopause) among the controls. Pearson correlations between log2-transformed values of IGF-I and IGFBP-3 and continuous breast cancer risk factors (age at serum draw, body mass index, height, age at menarche, age at menopause, number of live births, age at first live birth, drinks of alcoholic beverages per day, education, and log2-transformed estradiol), weighted according to the inverse of the sampling fraction, were calculated among controls using PROC CORR in SAS.
HRs for IGF-I, IGFBP-3, and the molar ratio IGF-I/IGFBP-3 and breast cancer risk were examined according to quintiles of these variables among the controls, weighted to represent the cohort. Quintile categories of IGF-I and IGFBP-3 were treated as a continuous variable to test for linear trend; the HR from these analyses represents the risk associated with an increase of one quintile. Interactions between BMI and circulating estradiol levels (categorized as less than the median and greater than or equal to the median among the controls) and quintile categories of IGF-I and IGFBP-3 treated as a continuous variable were assessed by examining confidence intervals for the cross-product terms in the proportional hazards models.
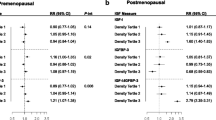
Several models for HRs across quintiles and HRs for a one quintile increase were created to control for confounding. These models include a minimally adjusted version with only the study design matching factors (models 1 in Table 4) and a second one also adjusted for accepted breast cancer risk factors and additional study design factors (time of day of blood collection and study center location; models 2 in Table 4), which changed the HR for a one quintile increase for IGF-I, IGFBP-3, and the molar ratio by ≤10%. Models 3 in Table 4 added IGF-I and IGFBP-3, each in quintiles, to the models for the other analyte. Subsequent models also included height in quintiles (model 4), baseline BMI in quintiles (model 5), serum unconjugated estradiol in quintiles (model 6), and all three of these variables (model 7). Adjusting for BMI and circulating estradiol, accepted risk factors for postmenopausal breast cancer which might share causal pathways with IGF-I, could potentially clarify the association with IGF-I.
Hazard ratios for the quintile variables treated as a continuous variable for different breast cancer subtypes were compared based on the point estimates and 95% confidence intervals.
All p values were two-sided, and p<0 .05 was considered statistically significant.
Results
The mean follow-up time for cases was 47.7 months, with a range of <1 month to 130 months, and that for controls was 91.8 months with a range of 9-137 months.
Selected characteristics of cases and controls are shown in Table 2. Mean age at blood draw was similar between cases and controls. Cases were less likely than controls to have had blood drawn in the morning between 9 and 12 and to have been diagnosed at study centers in the Southern USA. Cases were more likely to be taller and heavier; have higher circulating estradiol levels; have a family history of breast cancer and a personal history of benign breast disease; have an earlier age at menarche, fewer children, and a later age at first childbirth; and drink alcoholic beverages more frequently. These associations are consistent with what is known from the published literature on breast cancer risk factors. Contrary to expectation, cases did not have a later age at menopause or notably higher education levels.
Log2-transformed values of the serum concentrations of IGF-I and IGFBP-3 were statistically significantly correlated among controls (r = 0.69; p < .0001).
Geometric mean serum levels of IGF-I and IGFBP-3 (in nanogram per milliliter) according to levels of breast cancer risk factors and other selected variables are shown in Table 3. IGF-I and IGFBP-3 levels were weakly inversely, but statistically significantly, associated with estradiol levels and weakly positively, but statistically significantly, associated with height and education. IGF-I levels were weakly inversely, but statistically significantly, associated with age at serum draw, but those of IGFBP-3 were not. IGF-1 levels were also weakly inversely and statistically significantly associated with BMI, but IGFBP-3 did not vary significantly with BMI. Levels of IGFBP-3, but not IGF-I were weakly inversely and statistically significantly associated with age at menarche. IGFBP-3, but not IGF-I, levels were statistically significantly higher in Whites than in Blacks and other races, and in those women with a history of benign breast disease. Although not statistically significant, IGF-I and IGFBP-3 levels generally increased with time of day of the blood draw. Associations were not statistically significant for the other potential confounders.
Geometric mean serum levels (in nanogram/milliliter) for IGF-I were 209.26 (95% CI 203.01, 215.51) and 205.47 (95% CI 198.43, 212.51) in the cases and controls, respectively. Corresponding geometric mean levels for IGFBP-3 were 4,580.44 (95% CI 4,492.81, 4,668.07) and 4,578.62 (95% CI 4,499.85, 4,657.39). The geometric mean molar ratio was 0.16 in both cases and controls.
Table 4 includes multivariate models for IGF-I and IGFBP-3 and the IGF-I/IGFBP-3 molar ratio that sequentially adjust for study matching factors; accepted breast cancer risk factors; the other IGF measure; and height, BMI, and circulating estradiol, risk factors that may share causal pathways with IGF-I. Using the fully adjusted multivariate model (model 7), the HRs for IGF-I, IGFBP-3, and the molar ratio, comparing the highest quintile to the lowest, were 1.28 (95% CI, 0.67-2.44), 1.12 (95% 0.55-2.27), and 1.25 (95% 0.72-2.15), respectively. HRs for the molar ratio peaked in the fourth quintile (HR = 1.98; 95% CI 1.20-3.29). Multivariate HRs for the increase per quintile were 1.07 (95% CI 0.92-1.25) for IGF-I, 1.01 (95% 0.86-1.18) for IGFBP-3, and 1.10 (95% 0.98-1.24) for the molar ratio. The major confounders of the IGF-I and molar ratio associations with breast cancer risk were BMI and estradiol levels, adjustment for which noticeably increased HRs, and height, adjustment for which reduced the HRs.
Interactions between IGF-I and IGFBP-3 and age at serum donation (55-64, 65-74), BMI (less than median, greater than or equal to median at baseline), and circulating estradiol levels (less than median, greater than or equal to median) were not statistically significant.
To eliminate any effects of preclinical disease on the serum IGF measures, analyses were limited to the 283 breast cancer cases diagnosed more than 24 months after entry into the study and the 467 controls who exited the study at least 24 months after study entry. The HRs associated with a quintile increase in IGF-I, IGFBP-3, and the molar ratio (all using model 7) were essentially unchanged: 1.06 (95% CI 0.89, 1.26), 1.01 (95% CI 0.84, 1.20), and 1.11 (95% CI 0.98-1.27), respectively.
The HRs for invasive cancer (N = 308) associated with a quintile increase in IGF-I, IGFBP3, and the molar ratio (all with model 7) were 1.04 (95% CI 0.88-1.22), 1.04 (95% CI 0.87-1.23), and 1.07 (95% CI 0.94-1.21), respectively. The corresponding results for in situ breast cancer (80 cases) were 1.22 (95% CI 0.93-1.61), 0.91 (95% CI 0.67-1.24), and 1.25 (95% CI 1.01-1.56). These HR estimates for invasive and in situ breast cancer had overlapping confidence intervals, suggesting no statistically significant differences.
When analyses were limited to the 293 ductal cancers (both invasive and in situ), the HRs associated with a quintile increase for IGF-1, IGFBP-3, and the molar ratio (all with model 7) were 1.13 (95% CI 0.96-1.34), 0.94 (95% CI 0.79-1.13), and 1.14 (95% CI 1.01-1.30), respectively. Corresponding HRs for the 57 lobular cancers were 1.09 (95% CI 0.78-1.54), 0.99 (95% CI 0.68-1.43), and 1.13 (95% CI 0.84-1.52). For the small number of cancers with other histologies (39 cases), the corresponding HRs were 0.70 (95% CI 0.38-1.29), 1.78 (95% CI 0.85-3.75), and 0.96 (95% CI 0.66-1.40). Confidence intervals for the different histologic subtypes were overlapping.
HRs for the 222 ER-positive cases per quintile increase in IGF-I, IGFBP3, and the molar ratio (all with model 7) were 1.05 (95% CI 0.87-1.28), 0.98 (95% CI 0.80-1.21), and 1.07 (95% CI 0.92-1.24), respectively. The corresponding HRs for the 45 ER-negative cases were 1.06 (95% CI 0.66-1.70), 1.09 (95% CI 0.71-1.68), and 1.03 (95% CI 0.71-1.50). Confidence intervals were overlapping.
Discussion
In this relatively large study with prospectively collected serum samples, we found small positive, but not statistically significant, associations between circulating levels of both IGF-I and the molar ratio IGF-I/IGFBP-3 and postmenopausal breast cancer risk. Circulating IGFBP-3 levels were not associated with risk. Adjustment for BMI and circulating estradiol levels each strengthened the associations with IGF-I and the molar ratio. No statistically significant differences were found according to invasive/in situ status or tumor histology, although the molar ratio was associated with statistically significant increases in risk of in situ breast cancer and breast cancer with a ductal histology. Similarly, no statistically significant differences were found by hormone receptor status. However, analyses by breast cancer histology and ER status were limited by the small number of cases in each subgroup.
The magnitude of the HRs for IGF-I in our study are slightly lower, but not markedly different, than those reported in the second largest prospective study to date, a study conducted within the European Prospective Investigation into Cancer and Nutrition (EPIC) with 614 cases of postmenopausal breast cancer, which reported a statistically significant positive association between IGF-I and breast cancer risk in women older than 50 years [13]. However, we did not find positive associations with IGFBP-3, as did the EPIC study. Another recent cohort study conducted in Australia and including 257 postmenopausal cases, also reported statistically significant positive associations with IGF-I and IGFBP-3 and breast cancer risk, but associations with IGF-I were of greater magnitude [14]. Several studies have suggested that associations among postmenopausal women were strongest among older postmenopausal women [14, 15]. Contrary to both of these studies [13, 14], we did not find a positive association between IGFBP-3 and breast cancer risk.
The majority of recent cohort studies of circulating IGF-I levels and breast cancer risk in postmenopausal women have reported no statistically significant associations [5–9]; three of these studies had more cases than our study [5, 7, 8]. Meta-analyses and systematic reviews of results published in October 2003 [10], July 2003 [11], and December 2002 [12] also report no statistically significant associations.
It is not immediately obvious why results among studies have been discrepant. Studies with prospectively collected blood samples have produced both statistically significant positive and nonsignificant/null associations. Furthermore, both significant positive [13] and nonsignificant/null [7, 8] findings have been reported in studies with a relatively large number of breast cancer cases. Studies with IGF-I and IGFBP-3 measured in serum and plasma have also produced both positive [13, 14] and null associations [5, 7–9]. We found no effect modification by age at blood draw, so differing age distributions are unlikely to explain the stronger positive associations in the study of Baglietto et al. [14] versus ours. We found no difference in the associations with our three IGF measures after excluding the first 2 years of follow-up, contrary to the study of Rinaldi et al. [13], in which associations were stronger after the exclusion of the early period of follow-up.
We found no statistically significant differences according to ER status of the tumors, in spite of experimental evidence that the estrogen receptor mediates IGF-I stimulation of mitogenesis [22]. One cohort study in postmenopausal women reported positive associations with ER-positive tumors, but not ER-negative tumors [8], whereas another reported no differences by receptor status [5]. Several of the larger studies reported results were similar when in situ cancers were removed from analyses [5, 7]. Others were restricted to invasive cancers [3, 13, 14]. To our knowledge, other epidemiologic studies of breast cancer have not looked at associations with circulating IGF-I according to tumor morphology.
Strengths of this study include the prospective collection of serum, which reduces the possibility that circulating levels of the IGF measures or participation rates were influenced by disease, and the relatively long follow-up period, which allowed the accrual of a sufficient number of breast cancer cases diagnosed several years after serum collection to rule out the possibility that preclinical disease affected circulating levels of the IGF measures. Other strengths include the relatively large number of breast cancer cases and detailed information on most accepted breast cancer risk factors, including endogenous estradiol levels. Finally, a standardized, vetted protocol was used to collect and store serum samples; and the laboratory assays for the IGF assays were excellent.
As have other studies of the relationship between circulating levels of IGF-I and IGFBP-3 and subsequent breast cancer risk, we relied on blood samples collected at one point in time from each woman, even though IGF measures fluctuate over time and decrease with age. However, in an analysis of women with two blood collections, with a median time between collections of 14 months, intra-class correlations between repeat measurements were 0.66 (95% CI 0.51-0.77) and 0.86 (95% CI 0.79-0.91) for serum IGF-I and IGFBP-3, respectively [23], which suggests reasonable stability in the measurements over a limited period of time.
A limitation of our analysis is the absence of data on other potentially informative serologic parameters, including insulin/c-peptide. Addition of circulating estradiol levels to the IGF-I and molar ratio models strengthened the modest associations with breast cancer risk. Like estradiol, insulin may independently influence risk of breast cancer. In a recent large case-cohort analysis of postmenopausal women, fasting insulin was associated with a statistically significant 50% increase in breast cancer risk [5]. However, in two studies the correlations of IGF-I and IGFBP-3 with insulin/c-peptide were not statistically significant [5, 9], and adjustment for insulin/c-peptide levels did not change [9] or only slightly decreased associations with IGF-I [5].
In evaluating our results and those of others, it is important to consider the biology of the IGF signaling system. Three pools of IGFs exist in circulation. Approximately 75-80% of circulating IGF is bound to IGFBP-3 and the acid labile α-subunit (ALS) to form 150-200 kDa ternary complexes, 20-25% is complexed with the other five IGFBPs (but not ALS) as 50 kDa complexes, and less than 1% exists in free form [24]. The 150-200 kDa ternary complexes do not cross the capillary endothelial barrier and thus limit the bioavailability in various tissues. The smaller IGF-IGFBP complexes can permeate into the tissues, but prevent the binding of IGF to its receptors [24]. Thus, the bioavailability of IGFs to local tissues requires disruption of these IGF/IGFBP complexes, which can be facilitated by proteolysis of the IGFBPs [24]. The assays used in this and most epidemiologic studies measure total IGF-I (both bound and unbound) and total IGFBP-3 (both intact IGFBP-3 and some proteolytic fragments), but not necessarily the bioactive components. In a recent study among premenopausal women, an IGFBP-3 assay measuring only the forms able to bind IGF was used to measure “functional” IGFBP-3. Use of the IGF-I/“functional” IGFBP-3 molar ratio and adjustment of IGF-I for “functional” IGFBP-3 resulted in much stronger associations of these IGF measures with breast cancer risk [25].
Some have suggested that IGFBP-3 and certain IGFBP-3 fragments may be functional through mechanisms that do not involve IGF-I [26]. Others have suggested that an increasing molar ratio of IGF-I to IGFBP-3 simply reflects free, biologically active IGF-I [20]. Whatever the mechanism of action for IGFBP-3, analyses that distinguish between biologically active and inactive forms of IGFBP-3, as well as IGF-I, might help elucidate the relationship of the IGF signaling pathway to breast cancer risk.
In summary, the present study found positive, but not statistically significant, associations between circulating levels of IGF-I and the molar ratio IGF-I/IGFBP-3 and postmenopausal breast cancer risk. These associations were strengthened by incorporating circulating estradiol into the models, which suggests that IGF-I increases the risk of postmenopausal breast cancer through a pathway partially independent of postmenopausal endogenous estrogen. We did not have sufficient power to determine with confidence whether the IGF-I associations differed by breast tumor morphology, histology, and steroid hormone receptor status. Further research on the role of IGF-I in breast cancer etiology should emphasize larger studies, including pooled analyses; analyses by breast cancer subtype; improved exposure assessment, with an emphasis on measuring bioavailable IGF-I; and possible mechanisms of action.
References
Sachdev D, Yee D (2001) The IGF system and breast cancer. Endocr Relat Cancer 8:197–209
Lann D, LeRoith D (2008) The role of endocrine insulin-like growth factor-I and insulin in breast cancer. J Mammary Gland Biol Neoplasia 13:371–379, Epub 2008 Nov 22
Hankinson SE, Willett WC, Colditz GA, Hunter DJ, Michaud DS, Deroo B, Rosner B, Speizer FE, Pollak M (1998) Circulating concentrations of insulin-like growth factor-I and risk of breast cancer. Lancet 351:1393–1396
Renehan AG, Harvie M, Howell A (2006) Insulin-like growth factor (IGF)-I, IGF binding protein-3, and breast cancer risk: eight years on. Endocr Relat Cancer 13:273–278
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE, Manson JE, Li J, Ho GFY, Xue X, Anderson GL, Kaplan RC, Harris TG et al (2009) Insulin, insulin-like growth factor-I, and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 101:48–60
Allen NE, Roddam AW, Allen DS, Fentiman IS, dos Santos SI, Peto J, Holly JMP, Key TJ (2005) A prospective study of serum insulin-like growth factor-I (IGF-I), IGF-II, IGF-binding protein-3 and breast cancer risk. Br J Cancer 92:1283–1287
Schernhammer ES, Holly JM, Pollak MN, Hankinson SE (2005) Circulating levels of insulin-like growth factors, their binding proteins, and breast cancer risk. Cancer Epidemiol Biomarkers Prev 14:699–704
Grønbaek H, Flyvbjerg A, Mellemkjaer L, Tjønneland A, Christensen J, Sørensen HT, Overvad K (2004) Serum insulin-like growth factors, insulin-like growth factor binding proteins, and breast cancer risk in postmenopausal women. Cancer Epidemiol Biomarkers Prev 13:1759–1764
Keinan-Boker L, Bueno de Mesquita HB, Kaaks R, Van Gils CH, Van Noord PAH, Rinaldi S, Riboli E, Seidell JC, Grobbee DE, Peeters PHM (2003) Circulating levels of insulin-like growth factor I, its binding proteins -1, -2, -3, c-peptide and risk of postmenopausal breast cancer. Int J Cancer 106:90–95
Fletcher O, Gibson L, Johnson N, Altmann DR, Holly JMP, Ashworth A, Peto J, dos Santos SI (2005) Polymorphisms and circulating levels in the insulin-like growth factor system and risk of breast cancer: a systematic review. Cancer Epidemiol Biomarkers Prev 14:2–19
Shi R, Yu H, McLarty J, Glass J (2004) IGF-I and breast cancer: a meta-analysis. Int J Cancer 111:418–423
Renehan AG, Zwahlen M, Minder C, O’Dwyer ST, Shalet SM, Egger M (2004) Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet 363:1346–1353
Rinaldi S, Peeters PHM, Berrino F, Dossus L, Biessy C, Olsen A, Tjonneland A, Overvad K, Clavel-Chapelon F, Boutron-Ruault MC, Téhard B, Nagel G et al (2006) IGF-I, IGFBP-3 and breast cancer risk in women: the european prospective investigation into cancer and nutrition (EPIC). Endocr Relat Cancer 13:593–605
Baglietto L, English DR, Hopper JL, Morris HA, Tilley WD, Giles GG (2007) Circulating insulin-like growth factor-I and binding protein-3 and the risk of breast cancer. Cancer Epidemiol Biomarkers Prev 16:763–768
Rollison DE, Newschaffer CJ, Tao Y, Pollak M, Helzlsouer KJ (2006) Premenopausal levels of circulating insulin-like growth factor I and the risk of postmenopausal breast cancer. Int J Cancer 118:1279–1284
Kaaks R, Lundin E, Rinaldi S, Biessy C, Søderberg S, Lenner P, Janzon L, Riboli E, Berglund G, Hallmans G (2002) Prospective study of IGF-I, IGF-binding proteins, and breast cancer risk, in northern and southern Sweden. Cancer Causes Control 13:307–316
Prorok PC, Andriole GL, Bresalier RS, Buys SS, Chia D, Crawford ED, Fogel R, Gelmann EP, Gilbert F, Hasson MA, Hayes RB, Johnson CC, Mandel JS, Oberman A et al (2000) Design of the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial 1. Control Clin Trials 21:273–309S
Hayes RB, Sigurdson A, Moore L, Peters U, Huang WY, Pinsky P, Reding D, Gelmann EP, Rothman N, Pfeiffer RM, Hoover RN, Berg CD, for the PLCO Trial Team (2005) Methods for etiologic and early marker investigations in the PLCO trial. Mutat Res 592:147–154
Fears TR, Ziegler RG, Donaldson JL, Falk RT, Hoover RN, Stanczyk FZ, Vaught JB, Gail MH (2000) Reproducibility studies and interlaboratory concordance for androgen assays in female plasma. Cancer Epidemiol Biomarkers Prev 9:403–412
Juul A, Dalgaard P, Blum WF, Bang P, Hall K, Michaelsen KF, Müller J, Skakkebaek (1995) Serum levels of insulin-like growth factor (IGF)-binding protein-3 (IGFBP-3) in healthy infants, children, and adolescents: the relation to IGF-I, IGF-II, IGFBP-1, IGFBP-2, age, sex, body mass index, and pubertal maturation. J Clin Endocrinol Metab 80:2534–2542
Xu X, Roman JM, Issaq HJ, Keefer LK, Veenstra TD, Ziegler RG (2007) Quantitative measurement of endogenous estrogens and estrogen metabolites in human serum by liquid chromatography-tandem mass spectrometry. Anal Chem 79:7813–7821
Yee D, Lee AV (2000) Crosstalk between the insulin-like growth factors and estrogens in breast cancer. J Mammary Gland Biol Neoplasia 5:107–115
Lukanova A, Zeleniuch-Jacquotte A, Lundin E, Micheli A, Arslan AA, Rinaldi S, Muti P, Lenner P, Koenig KL, Biessy C, Krogh V, Riboli E et al (2004) Prediagnostic levels of c-peptide, IGF-I, IGFBP-1, -2, and -3 and risk of endometrial cancer. Int J Cancer 108:262–268
Rajaram S, Baylink DJ, Mohan S (1997) Insulin-like growth factor-binding proteins in serum and other biological fluids: regulation and functions. Endocr Rev 18:801–831
Rinaldi S, Kaaks R, Zeleniuch-Jacquotte A, Arslan AA, Shore RE, Koenig KL, Dossus L, Riboli E, Stattin P, Lukanova A, Toniolo P (2005) Insulin-like growth factor-I, IGF binding protein-3, and breast cancer in young women: a comparison of risk estimates using different peptide assays. Cancer Epidemiol Biomarkers Prev 14:48–52
Renehan A (2005) Insulin-like growth-factor-binding protein-3, breast cancer risk, and different serum assays. Cancer Epidemiol Biomarkers Prev 14:1844
Acknowledgments
We are grateful for the outstanding computer support from Craig Williams at IMS, Inc. This study was funded by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics and contracts from the Division of Cancer Prevention, National Cancer Institute, National Institutes of Health, Department of Health and Human Services.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schairer, C., McCarty, C.A., Isaacs, C. et al. Circulating Insulin-like Growth Factor (IGF)-I and IGF Binding Protein (IGFBP)-3 Levels and Postmenopausal Breast Cancer Risk in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO) Cohort. HORM CANC 1, 100–111 (2010). https://doi.org/10.1007/s12672-010-0013-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-010-0013-y