Abstract
Background
Data on nonalcoholic fatty liver disease (NAFLD) in the Philippines are scarce. We aimed to compare the clinical and biochemical profiles of lean (BMI<23) vs. non-lean (BMI≥23) NAFLD patients.
Methods
Consecutive patients diagnosed with NAFLD on ultrasound in two outpatient hepatology clinics from February 2007-January 2017 were included. Patients with significant alcohol intake, alternative causes of steatosis, and incomplete data were excluded.
Results
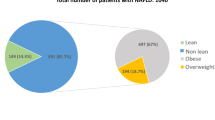
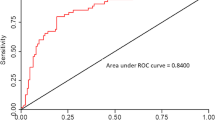
A total of 663 patients (57.9% male) were included. Most patients were non-lean (88.1%) and had an elevated alanine aminotransferase (ALT) (63%). Cirrhosis or hepatocellular carcinoma (HCC) were already present in 8.4% on initial consultation. Concomitant hepatitis B was equally common in patients with and without cirrhosis (20.7% vs. 17.5%; p=0.660) or HCC (17.9% vs. 12.8%; p=0.415). Independent factors associated with HCC/cirrhosis on initial consultation were older age (OR=1.038), low albumin (OR=0.428), high BARD score (BMI, AST/ALT ratio, T2 diabetes mellitus; OR=2.548) and the presence of symptoms (OR=1.808). Compared to lean NAFLD patients, non-lean patients were more likely to be younger (51.5±14.4 vs. 55±14.3; p=0.003), have DM (47.9% vs. 29.1%; p=0.002), hypertension (57.5% vs. 38%; p=0.001), dyslipidemia (73.1% vs. 54.4%; p=0.001) and metabolic syndrome (60.3% vs. 30.4%; p<0.0001), abnormal metabolic parameters (LDL-C, HDL-C, triglycerides, uric acid and FBS), and with elevated ALT (65.2% vs. 46.8%; p=0.002) and AST (41.1±29.6 vs. 35.3±28.3; p=0.008).
Conclusions
The proportion of lean NAFLD was 11.9%. Although metabolic derangements and its clinical consequences were present in about a third of lean patients, these were still more common in non-lean NAFLD. Cirrhosis or HCC were already present in a significant proportion (8.4%) of NAFLD patients on initial presentation.

Similar content being viewed by others
References
Ahmed M. Non-alcoholic fatty liver disease in 2015. World J Hepatol. 2015;7:1450–9.
Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–31.
De Lusong MA, Labio E, Daez L, Gloria V. Non-alcoholic fatty liver disease in the Philippines: comparable with other nations? World J Gastroenterol. 2008;14:913–7.
Bellentani S. The epidemiology of non-alcoholic fatty liver disease. Liver Int. 2017;37 Suppl 1:81–4.
Targher G, Bertolini L, Padovani R, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;3:1212–8.
Medina J, Fernandez-Salazar LI, Garcia-Buey L, Moreno-Otero R. Approach to the pathogenesis and treatment of nonalcoholic steatohepatitis. Diabetes Care. 2004;27:2057–66.
Fattahi MR, Niknam R, Safarpour A, Sepehrimanesh M, Lotfi M. The prevalence of metabolic syndrome in non-alcoholic fatty liver disease; a population-based study. Middle East J Digest Dis. 2016;8:131–7.
Leung JC, Loong TC, Wei JL, et al. Histological severity and clinical outcomes of nonalcoholic fatty liver disease in nonobese patients. Hepatology. 2017;65:54–64.
Kim D, Kim W, Joo SK, et al. Predictors of nonalcoholic steatohepatitis and significant fibrosis in non-obese nonalcoholic fatty liver disease. Liver Int. 2019;39:332–41.
Cho HC. Prevalence and factors associated with nonalcoholic fatty liver disease in a nonobese Korean population. Gut Liver. 2016;10:117–25.
Kwon YM, Oh SW, Hwang SS, Lee C, Kwon H, Chung GE. Association of nonalcoholic fatty liver disease with components of metabolic syndrome according to body mass index in Korean adults. Am J Gastroenterol. 2012 Dec;107:1852–8.
Feng RN, Du SS, Wang C, et al. Lean-non-alcoholic fatty liver disease increases risk for metabolic disorders in a normal weight Chinese population. World J Gastroenterol. 2014;20:17932–40.
Feldman A, Eder SK, Felder TK, et al. Clinical and metabolic characterization of lean Caucasian subjects with non-alcoholic fatty liver. Am J Gastroenterol. 2017;112:102–10.
Hagstrom H, Nasr P, Ekstedt M, et al. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: a long-term follow-up study. Hepatol Commun. 2018;2:48–57.
Golabi P, Paik J, Fukui N, Locklear CT, de Avilla L, Younossi ZM. Patients with lean nonalcoholic fatty liver disease are metabolically abnormal and have a higher risk for mortality. Clin Diabetes. 2019;37:65–72.
Chen F, Esmaili S, Rogers GB, et al. Lean NAFLD: A distinct entity shaped by differential metabolic adaptation. Hepatology. 2020;71:1213–27.
Zou B, Yeo YH, Nguyen VH, Cheung R, Ingelsson E, Nguyen MH. Prevalence, characteristics and mortality outcomes of obese, nonobese and lean NAFLD in the United States, 1999-2016. J Intern Med. 2020;288:139–51.
Zeng J, Yang RX, Sun C, et al. Prevalence, clinical characteristics, risk factors, and indicators for lean Chinese adults with nonalcoholic fatty liver disease. World J Gastroenterol. 2020;26:1792–804.
Niriella MA, Kasturiratne A, Pathmeswaran A, et al. Lean non-alcoholic fatty liver disease (lean NAFLD): characteristics, metabolic outcomes and risk factors from a 7-year prospective, community cohort study from Sri Lanka. Hepatol Int. 2019;13:314–22.
Shao C, Ye J, Li F, Feng S, Wang W, Zhong B. Different predictors of steatosis and fibrosis severity among lean, overweight and obese patients with nonalcoholic fatty liver disease. Dig Liver Dis. 2019;51:1392–9.
Lazar MV, Eapen M, Nair HR, Siyad I, Gopalakrishna R. Correlation between insulin resistance and liver histology in patients with nonalcoholic steatohepatitis with and without obesity. Indian J Gastroenterol. 2020;39:42–49.
Younes R, Bugianesi E. NASH in lean individuals. Semin Liver Dis. 2019;39:86–95.
Pan WH, Yeh WT. How to define obesity? Evidence-based multiple action points for public awareness, screening, and treatment: an extension of Asian-Pacific recommendations. Asia Pac J Clin Nutr. 2008;17:370–4.
Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52.
Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–99.
Harrison SA, Oliver D, Arnold HL, Gogia S, Neuschwander-Tetri BA. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut. 2008;57:1441–7.
Shi Y, Wang Q, Sun Y, et al. The prevalence of lean/nonobese nonalcoholic fatty liver disease: a systematic review and meta-analysis. J Clin Gastroenterol. 2020;54:378–87.
FNRI-DOST. Food and Nutrition Research Institute-Department of Science and Technology Annual report 2014. Accessed from: https://www.fnri.dost.gov.ph/images/sources/AnnualReports/AR2014.pdf. on 30 June 2020.
Sookoian S, Pirola CJ. Systematic review with meta-analysis: risk factors for non-alcoholic fatty liver disease suggest a shared altered metabolic and cardiovascular profile between lean and obese patients. Aliment Pharmacol Ther. 2017;46:85–95.
Wong SN, Chua-Tan M, Hadloc A. Unchanging high prevalence of late hepatitis B virus discovery among patients with chronic hepatitis B: a comparison between two time periods. APASL HBV STC Conference 2018. 2018;Abs. O-001 (67).
Moorman AC, Xing J, Ko S, et al. Late diagnosis of hepatitis C virus infection in the Chronic Hepatitis Cohort Study (CHeCS): missed opportunities for intervention. Hepatology. 2015;61:1479–84.
David D, Raghavendran A, Goel A, et al. Risk factors for non-alcoholic fatty liver disease are common in patients with non-B non-C hepatocellular carcinoma in India. Indian J Gastroenterol. 2017;36:373–9.
Vilar-Gomez E, Chalasani N. Non-invasive assessment of non-alcoholic fatty liver disease: Clinical prediction rules and blood-based biomarkers. J Hepatol. 2018;68:305–15.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Ann Margaret Navarroza and Stephen Wong. The first draft of the manuscript was written by Ann Margaret Navarroza and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
AMCN, and SNW declare no competing interests.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Navarroza, A.M.C., Wong, S.N. Comparison of clinical and metabolic profiles of lean versus non-lean nonalcoholic fatty liver disease. Indian J Gastroenterol 40, 380–388 (2021). https://doi.org/10.1007/s12664-021-01184-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-021-01184-6