Abstract
Aim
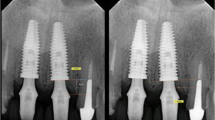
The objective of this retrospective cohort study was to compare the amount of marginal bone loss (MBL) in a bone-level and a soft-tissue-level implant system, both of which have similar intra-bony shape and surface composition. A subgroup analysis was done to compare the amount of MBL of each implant type in relation to the different vertical placement within the respective groups of implants.
Materials and Methods
Records of all patients who underwent implantation for replacement of teeth using comparable bone level (BL) and soft tissue level implants (TE) from 1st January 2006 to 31st December 2009 were scrutinized. Initial depth of implant placement (IDIP) was measured for all implants. Marginal bone loss was measured in patients whose records were available at time point corresponding to 12, 24 and 36 months post insertion.
Results
Out of a total of 384 implants, 337 implants were included for study. The mean MBL for the BL implants were 0.3, 0.38, 0.48 and for TE implant were 0.6, 0.54 and 0.93 for time periods 12, 24 and 36 months respectively. Although there was no statistically significant difference between the two groups at time periods at 6–12 months, in later time periods, there was a slightly greater amount of MBL around TE implants as compared to BL implants (p < 0.001). When comparing the IDIP and MBL in the same implant type, there was a statistically significant (p < 0.001) positive correlation between the depth of implant placement and the amount of MBL, with deeper placed implants having more bone loss.
Conclusion
Within the limitations of this retrospective cohort study design, one can conclude that BL implants had statistically significant lesser MBL as compared to TE in time periods above 12 months. Although the difference is statistically significant, the difference may not be clinically significant. The IDIP had an influence on the amount of MBL, with deeper placed implants and screw structure of the implant placed below the bone, having more MBL in the period of study.





Similar content being viewed by others
References
Albrektsson T, Zarb G, Worthington P, Eriksson AR (1986) The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1:11–25
Atieh MA, Ibrahim HM, Atieh AH (2010) Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol 81:1350–1366
Jones AA, Cochran DL (2006) Consequences of implant design. Dent Clin North Am 50:339–360
Hermann JS, Buser D, Schenk RK, Schoolfield JD, Cochran DL (2001) Biologic width around one- and two-piece titanium implants. Clin Oral Implants Res 12:559–571
Hermann JS, Schoolfield JD, Nummikoski PV, Buser D, Schenk RK, Cochran DL (2001) Crestal bone changes around titanium implants: a methodologic study comparing linear radiographic with histometric measurements. Int J Oral Maxillofac Implants 16:475–485
Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL (2001) Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol 72:1372–1383
Al-Nawas B, Kämmerer PW, Morbach T, Ophoven F, Wagner W (2001) Retrospective clinical evaluation of an internal tube-in-tube dental implant after 4 years, with special emphasis on peri-implant bone resorption. Int J Oral Maxillofac Implants 26:1309–1316
Hermann JS, Buser D, Schenk RK, Higginbottom FL, Cochran DL (2000) Biologic width around titanium implants. A physiologically formed and stable dimension over time. Clin Oral Implants Res 11:1–11
Jung RE, Jones AA, Higginbottom FL, Wilson TG, Schoolfeild J, Buser D, Hammerle CH, Cochran DL (2008) The influence of non matching implant and abutment diameters on radiographic crestal bone levels in dogs. J Periodontol 79:260–270
Enkling N, Jöhren P, Klimberg V, Bayer S, Mericske-Stern R, Jepsen S (2011) Effect of platform switching on peri-implant bone levels: a randomized clinical trial. Clin Oral Implants Res 22:1185–1192
Canullo L, Quaranta A, Teles RP (2010) The microbiota associated with implants restored with platform switching: a preliminary report. J Periodontol 81:403–411
Weng D, Nagata MJH, Bell M, Bosco AF, de Melo LGN, Richter EJ (2008) Influence of microgap location and configuration on the periimplant bone morphology in submerged implants. An experimental study in dogs. Clin Oral Implants Res 19:1141–1147
Degidi M, Perrotti V, Shibli JA, Novaes AB, Piatelli A, Iezzi G (2011) Equicrestal and subcrestal dental implants: a histologic and histomorphometric evaluation of nine retrieved human implants. J Periodontol 82:708–715
Novaes AB Jr, Barros RR, Mugila VA, Borges GJ (2009) Influence of interimplant distances and placement depth on papilla formation and crestal resorption: a clinical and radiographic study in dogs. J Oral Implantol 35:18–27
Barros RR, Novaes AB Jr, Mugila VA, Iezzi G, Piattelli A (2010) Influence of interimplant distances and placement depth on peri-implant bone remodeling of adjacent and immediately loaded Morse cone connection implants: a histomorphometric study in dogs. Clin Oral Implants Res 21:371–378
Zechner W, Watzak G, Gahleitner A, Busenlechner D, Tepper G, Watzek G (2003) Rotational panoramic versus intraoral rectangular radiographs for evaluation of peri-implant bone loss in the anterior atrophic mandible. Int J Oral Maxillofac Implants 18:873–878
Kullman L, Al-Asfour A, Zetterqvist L, Andersson L (2007) Comparison of radiographic bone heights assessments in panoramic and intraoral radiographs of implant patients. Int J Oral Maxillofac Implants 22:96–100
Al-Nawas B, Brägger U, Meijer HJ, Naert I, Persson R, Perucchi A, Quirynen A, Raghoebar GM, Reichert TE, Romeo E, Santing HJ, Schimmel M, Storelli S, Bruggenkate CT, Vandekerckhove B, Wagner W, Wismeijer D, Müller F (2012) A double-blind randomized controlled trial (RCT) of titanium-13zirconium versus titanium Grade IV small-diameter bone level implants in edentulous mandibles—results from a 1-year observation period. Clin Implant Dent Rel Res 14:896–904
Lazzara RJ, Porter SS (2006) Platform switching: a new concept in implant dentistry for controlling post restorative crestal bone levels. Int J Periodontics Restor Dent 2006:9–17
Canullo L, Fedele GR, Iannello G, Jepsen S (2010) Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial. Clin Oral Implants Res 21:115–121
Buser D, Wittneben J, Bornstein MM, Grütter L, Chappuis V, Belser UC (2011) Stability of contour augmentation and esthetic outcomes of implant-supported single crowns in the esthetic zone: 3-year results of a prospective study with early implant placement postextraction. J Periodontol 82:342–349
Wennström JL, Ekestubbe A, Gröndahl K, Karlsson S, Lindhe J (2005) Implant-supported single-tooth restorations: a 5-year prospective study. J Clin Periodontol 32:567–574
Chou CT, Morris HF, Ochi S, Walker L, DesRosiers D (2004) AICRG, Part II: crestal bone loss associated with the Ankylos implant: loading to 36 months. J Oral Implantol 30:134–143
Maeda Y, Miura J, Taki I, Sogo M (2007) Biomechanical analysis on platform switching: is there any biomechanical rationale? Clin Oral Implants Res 18:581–584
Canay S, Akca K (2009) Biomechanical aspects of bone-level diameter shifting at implant–abutment interface. Implant Dent 18:239–248
Cocchetto R, Traini T, Caddeo F, Celletti R (2010) Evaluation of hard tissue response around wider platform-switched implants. Int J Periodontics Restor Dent 30:163–171
Cappiello M, Luongo R, Di Iorio D, Bugea C, Cocchetto R, Celletti R (2008) Evaluation of peri-implant bone loss around platform-switched implants. Int J Periodontics Restor Dent 28:347–355
Buser D, von Arx T (2000) Surgical procedures in partially edentulous patients with ITI implants. Clin Oral Implants Res 11(Suppl 1):83–100
Pontes AEF, Ribeiro FS, Iezzi G, Piattelli A, Cirelli JA, Marcantonio E (2008) Biologic width changes around loaded implants inserted in different levels in relation to crestal bone: histometric evaluation in canine mandible. Clin Oral Implants Res 19:483–490
Pontes AEF, Ribeiro FS, da Silva VC, Margonar R, Piattelli A, Cirelli JA, Marcantonio E (2008) Clinical and radiographic changes around dental implants inserted in different levels in relation to the crestal bone, under different restoration protocols, in the dog model. J Periodontol 79:486–494
Todescan FF, Pustiglioni FE, Imbronito AV, Albrektsson T, Gioso M (2002) Influence of the microgap in the peri-implant hard and soft tissues: a histomorphometric study in dogs. Int J Oral Maxillofac Implants 17:467–472
Broggini N, McManus LM, Hermann JS, Medina R, Schenk RK, Buser D, Cochran DL (2006) Peri-implant inflammation defined by the implant–abutment interface. J Dent Res 85:473–478
Callan DP, Cobb CM, Williams KB (2005) DNA probe identification of bacteria colonizing internal surfaces of the implant–abutment interface: a preliminary study. J Periodontol 76:115–120
Quirynen M, van Steenberghe D (1993) Bacterial colonization of the internal part of the two-stage implants. An in vivo study. Clin Oral Implants Res 4:158–161
Acknowledgments
The study was supported by the ITI Research Scholarship grant by the ITI-Foundation to the corresponding author.
Conflict of interest
The senior authors Prof Wagner und Prof Al-Nawas declare that they were involved in education and scientific lectures and get research grants by the Straumann company but have no conflicts of interest in this study. All other authors have no conflict of interest in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The data from this study is part of the dissertation work submitted to Johannes Gutenberg University, Mainz as part of doctoral thesis of Dr. Vinay V. Kumar.
Rights and permissions
About this article
Cite this article
Kumar, V.V., Sagheb, K., Kämmerer, P.W. et al. Retrospective Clinical Study of Marginal Bone Level Changes with Two Different Screw-Implant Types: Comparison Between Tissue Level (TE) and Bone Level (BL) Implant. J. Maxillofac. Oral Surg. 13, 259–266 (2014). https://doi.org/10.1007/s12663-013-0532-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-013-0532-5