Abstract
Purpose
Knowledge of how alterations in pharmacogenomics and pharmacogenetics may affect drug therapy in the intensive care unit (ICU) has received little study. We review the clinically relevant application of pharmacogenetics and pharmacogenomics to drugs and conditions encountered in the ICU.
Source
We selected relevant literature to illustrate the important concepts contained within.
Principal findings
Two main approaches have been used to identify genetic abnormalities - the candidate gene approach and the genome-wide approach. Genetic variability in response to drugs may occur as a result of alterations of drug-metabolizing (cytochrome P [CYP]) enzymes, receptors, and transport proteins leading to enhancement or delay in the therapeutic response. Of relevance to the ICU, genetic variation in CYP-450 isoenzymes results in altered effects of midazolam, fentanyl, morphine, codeine, phenytoin, clopidogrel, warfarin, carvedilol, metoprolol, HMG-CoA reductase inhibitors, calcineurin inhibitors, non-steroidal anti-inflammatory agents, proton pump inhibitors, and ondansetron. Changes in cholinesterase enzyme function may affect the disposition of succinylcholine, benzylisoquinoline muscle relaxants, remifentanil, and hydralazine. Genetic variation in transport proteins leads to differences in the response to opioids and clopidogrel. Polymorphisms in drug receptors result in altered effects of β-blockers, catecholamines, antipsychotic agents, and opioids. Genetic variation also contributes to the diversity and incidence of diseases and conditions such as sepsis, malignant hyperthermia, drug-induced hypersensitivity reactions, cardiac channelopathies, thromboembolic disease, and congestive heart failure.
Conclusion
Application of pharmacogenetics and pharmacogenomics has seen improvements in drug therapy. Ongoing study and incorporation of these concepts into clinical decision making in the ICU has the potential to affect patient outcomes.
Résumé
Objectif
Peu d’études ont cherché à savoir comment des modifications de la pharmacogénomique et de la pharmacogénétique pouvaient affecter les traitements médicamenteux à l’unité de soins intensifs (USI). Nous passons en revue l’application, pertinente d’un point de vue clinique, de la pharmacogénétique et de la pharmacogénomique aux médicaments et aux conditions rencontrés à l’USI.
Source
Nous avons sélectionné la littérature pertinente afin de décrire les concepts importants qu’elle comportait.
Constatations principales
Deux approches principales ont été utilisées afin d’identifier les anomalies génétiques, soit l’approche de gène candidat et l’approche à l’échelle du génome. La variabilité génétique en réponse aux médicaments peut survenir en raison d’altérations au niveau des enzymes métabolisant les médicaments (cytochrome P [CYP]), des récepteurs et des protéines de transport, altérations qui entraînent une exacerbation ou un retard de la réponse thérapeutique. Pertinente à l’USI, la variation génétique des iso-enzymes CYP-450 modifie les effets du midazolam, du fentanyl, de la morphine, de la codéine, de la phénytoïne, du clopidogrel, de la warfarine, du carvédilol, du métoprolol, des inhibiteurs de la HMG-CoA réductase, des inhibiteurs de la calcineurine, des agents anti-inflammatoires non stéroïdiens, des inhibiteurs de la pompe à protons et de l’ondansétron. Des changements de la fonction enzymatique de la cholinestérase pourraient affecter le métabolisme de la succinylcholine, des myorelaxants tels que les benzylisoquinolines, du rémifentanil et de l’hydralazine. La variation génétique au niveau des protéines de transport provoque des différences de réaction aux opioïdes et au clopidogrel. Les polymorphismes au niveau des récepteurs médicamenteux altèrent les effets des bêtabloquants, des catécholamines, des agents antipsychotiques et des opioïdes. La variation génétique contribue également à la diversité et à l’incidence de maladies et de conditions telles que le sepsis, l’hyperthermie maligne, les réactions hypersensibles provoquées par les médicaments, les canalopathies cardiaques, les maladies thromboemboliques et l’insuffisance cardiaque congestive.
Conclusion
L’application de la pharmacogénétique et de la pharmacogénomique a permis d’améliorer les traitements médicamenteux. L’étude continue de ces concepts et leur intégration dans la prise de décision clinique à l’USI pourraient avoir un impact sur les issues des patients.
Similar content being viewed by others
The complete description of the human genome was published in 2002.1,2 Although application of genomics to medicine was initially embraced as the potential future for drug discovery3 and management,4 it has proven to be more difficult than was originally thought.5-7 Nevertheless, scientists have continued to unravel the role that genetic variability may play in altering the response to drug therapy, including variations in drug disposition.8,9 As a result, the clinical application of genetic information to guide clinical decision making and drug therapy is emerging.10 Genetic variability in response to drugs occurs as a result of molecular alterations of drug-metabolizing enzymes, drug targets, and transport proteins.11 Such insights have led to application of genetics in a variety of scenarios, including treatment of breast cancer,12 stroke,13 coronary artery disease,14 perioperative adverse events,15 and development of adverse drug reactions (ADRs).16
Rather than the traditional “one size fits all” approach to drug therapy, the application of targeted drug therapy might allow a more personalized approach, thereby minimizing the occurrence of therapeutic failures or adverse effects.17,18 Pharmacogenomic research seeks to characterize any particular individual’s susceptibility to a disease or drug effect based on their known genetic composition.19 When possible, it could revolutionize how drugs are discovered - by identifying those individuals most likely to respond to the experimental therapy - and eventually prescribed.20 Such an approach has been shown to be cost-effective.21 Compared to traditional dose-driven therapeutic drug monitoring - where pharmacological effect is associated with a given drug concentration and cannot be determined prior to the drug being used - pharmacogenomics would not depend on steady-state pharmacokinetics or compliance with drug administration for interpretation. Furthermore, it might be less invasive, could provide mechanistic information and predictive value for a number of drugs (e.g., metabolism by CYP3A4/5), and is stable throughout a patient’s life-span.22 Table 1 lists factors necessary for pharmacogenomics to result in a clinically important change in drug effect.
Despite the forgoing, the application of genetic variation to predict altered responses to drug therapy in patients in the intensive care unit (ICU) has received relatively little study.23 In part, it may be because diagnostic tests for genomic variability, until recently, have not been available within the short time frame necessary for decision making in the ICU.17,24,25 In addition, alterations in drug pharmacokinetics due to changes in bioavailability, volume of distribution, and drug- and disease-induced changes in drug metabolism and clearance that occur because of the nature of critical illness26 make it difficult to attribute observed differences in drug effects to alterations in genomic variability alone. Herein, we expand on the observations of Allen and Gelot23 and use the concepts of pharmacogenetics (i.e., application of a single genetic variant to describe an alteration in drug effect) and pharmacogenomics (i.e., the broader application of an individual’s genome to predict his or her response to medications) to explain some of the variability in clinical response commonly seen in a patient population. Our objective is to provide examples of the potential for the clinically relevant application of pharmacogenetics and pharmacogenomics to conditions and drugs commonly encountered in the ICU.
Concepts and definitions
Pharmacogenetics is the study of differences among individuals with regard to the clinical response to a particular drug (i.e., “one drug, many genomes”), whereas pharmacogenomics is the study of differences among compounds with regard to the gene expression response in a single normative genome (i.e., “many drugs, one genome”).27 Alterations in the human genetic code are common. When they occur in more than 1% of the population, they are described as genetic polymorphisms.28 Table 2 provides a glossary of terms frequently encountered when reading the literature on genetic alterations in drug effects. For further understanding of commonly used genetic terms and concepts, the reader is referred to other reviews.29-33 Examples of polymorphisms include variations in skin, hair, and eye color. Much of the genetic variation that occurs among individuals occurs because of single variations in the nucleotide sequence of the four base pairs of deoxyribonucleic acid - called single nucleotide polymorphisms (SNPs).34 By examining alterations in SNPs, geneticists have been able to identify the genetic variations associated with a particular condition, such as susceptibility to an ADR.35
Many factors affect response to drugs, including sex,36 age,37 critical illness,38 and concomitant drug therapy.39 Increasingly, however, it is recognized that genetic variation may play a significant role in the body’s handling of drugs.28,40 Differences in drug response identify groups of individuals with altered genetic profiles. Examples include familial cholinesterase deficiency and prolonged neuromuscular blockade following succinylcholine administration,28 peripheral neuropathy following isoniazide administration in patients with N-acetyltransferase deficiency,41 differential drug effects for treatment of hypertension in individuals of Black African origin,42 and alterations in p-glycoprotein function identified in twin studies (monozygotic vs dizygotic).43
Variation in genes encoding drug-metabolizing enzymes may lead to an absence of, reduction in, or increase in drug effect. For example, a high percentage of ADRs occur as a result of a genetic variation in one of the common cytochrome P (CYP)-450 drug-metabolizing enzymes.44 Individuals with two homozygous alleles coding for enzyme function are termed “normal” or “extensive metabolizers” (EMs) when more than one copy of the gene is present. Alternatively, individuals with two alleles resulting in inactive or absent enzyme function are termed “poor metabolizers” (PMs). Individuals with one functioning and one dysfunctional allele are termed “intermediate metabolizers” (IMs).28,45,46 In simplistic terms, individuals who are EMs have a normal response to a standard drug dose, whereas PMs would be unable to metabolize the drug to the same extent and are thus subject to a potentially excessive drug effect (including toxicity). Drug-metabolizing enzymes may also be responsible for conversion of prodrugs to their active moiety. Therefore, EMs in this scenario could potentially experience drug toxicity.47 This situation may be clinically relevant, however, only if other aspects that affect the variability of a particular drug’s response (e.g., age, sex) are minimal and the therapeutic index for the agent is narrow (e.g., warfarin). Furthermore, few drugs are metabolized by one enzyme system alone, and alterations in one metabolic pathway may not be reflected in an altered drug response if the other metabolic pathways can overcome the lack of metabolism by the deficient pathway.48
Likewise, variation in genes encoding drug transport proteins may alter absorption, distribution, and excretion of medications, resulting in an absence of, reduction in, or increase in drug effect. Patients with decreased expression of drug transport proteins in the duodenum may have increased drug bioavailability and therefore potentially be at risk of toxic effects.48 Decreased expression in the blood-brain barrier may increase drug access to the central nervous system sites of action.49
Variability in drug response can also be explained by genetic variability in drug targets. SNPs have been associated with genes that encode receptors, resulting in altered function, substrate binding affinity, expression, and both up- and down-regulation of receptors.48 Increased expression of receptors in tissues where the pharmacological effect is not desired can result in untoward effects. Conversely, down-regulation in response to agonism may result in lack of response, or tachyphylaxis.34,50
Ultimately, the consequences of variations in drug-metabolizing enzymes, transport proteins, and targets can be ineffective, even potentially toxic, drug therapy. This situation may lead to delay in the therapeutic response or ADRs. The latter may be a reason for the ICU admission itself,51 and either may be potentially devastating if experienced by the critically ill patient with already compromised physiological reserve. Later, we describe examples of genetic variation that have the potential to result in, or complicate, an ICU admission by categorizing the consequences of genetic variation as a resultant increase or decrease in drug effect.
There has recently been consensus on the nomenclature applied to pharmacogenomics. If adopted, it would help standardize the description of the altered genetic component.52 The following link provides comprehensive information on drug and genetic alterations that is updated regularly (https://www.pharmgkb.org/).53,54 Built on a knowledge pyramid, it provides information on a variety of relevant material, ranging from primary literature citations to clinical interpretation and implementation to dosing guidelines. Included also are interpretations and explanations of drug labels from the US Food and Drug Administration; European Medicines Agency; the Pharmaceuticals and Medical Devices Agency, Japan; and Health Canada (Santé Canada). There is cross-linking between clinically important pharmacogenomics, drug labels, and dosing guidelines. Under drug labels, lists of drugs are provided and categorized by (1) the genetic testing required or recommended, or (2) actionable or informative pharmacogenomics. For well-known pharmacogenomic associations, information is organized by gene/drug association and linked to dosing guidelines and drug label information. For example, phenytoin is listed in the table next to the three genes that affect its disposition (CYP2C19, CYP2C9, HLA-B), and for each of these genes there is a link to important pharmacogenomic information, which includes background on the function of the proteins encoded, gene frequencies, nomenclature, testing information, and drug and disease associations for the gene in question. Armed with this information, practitioners should be able to develop alternative drug strategies as necessary.
Application
Two main approaches have been employed for the clinical application of pharmacogenomics. The traditional approach has been to identify variability in drug response among individuals, confirm that the variation is not attributable to evident patient parameters (e.g., altered volume of distribution), and then seek an explanation in the SNPs in genes encoding proteins involved in the disposition of that particular drug (candidate gene approach).55 Once an SNP is found, gene frequencies - stratified by population - are necessary to determine the utility of testing for the allele in a given patient. If the frequency of the particular allele is determined to be substantial, an attempt is made to determine its clinical validity.56 Clinical validity is the genotype’s ability to predict a particular phenotype.57 Therefore, the allele in question could be considered clinically significant if (1) the frequency is considered significant, (2) the SNP can be detected with adequate sensitivity and specificity, and (3) the SNP reliably predicts response (efficacy or toxicity). In this “reactive” scenario, specific genetic testing can be performed prior to initiating use of the drug.58
For this genetic testing to be applicable to the ICU, point-of-care testing with rapid response rates would need to be readily available to guide decision making during the short time frame necessary for management of a critically ill patient. Additionally, variability in response to drugs in the critically ill may often be explained by the patient’s disease status or concomitant drugs, making identification of genomic variability difficult and potentially clinically irrelevant.59 Point-of-care testing, for example, has been successfully employed in the setting of clopidogrel administration following percutaneous coronary intervention. In a prospective randomized, proof-of-concept trial, Roberts et al. tested for the CYP2C19*2 genotype by way of a buccal swab.24 The results of the genetic test were available within 60 min, and patients who were carriers of this allele in the intervention arm received prasugrel instead of clopidogrel.
An alternative approach is to perform a genome-wide association study wherein the entire genomic profile of groups of patients with and without the disease or condition are compared, with genes indicative of the condition identified. The subsequent likely candidate gene(s) can then be studied in a confirmatory patient population.32,60,61 Genetic information gained can be used in a preemptive fashion, with genome identification using polymorphisms that are known and available at the time of prescribing and accompanying clinical decision support incorporated into the electronic health record.57 Investigators who prospectively performed genetic testing on patients scheduled for coronary arteriography recently reported using this method. The genetic information was stored and linked to the patient. At the time of prescribing clopidogrel, if the patient had a polymorphism such as CYP2C19*2, a drug genome interaction was displayed, as were recommendations for prescribing based on this interaction.62 Unfortunately, there is no reliable way to predict admission to the ICU for most critically ill patients. There is opportunity, however, to stratify patients that may be at increased risk for ICU admission (e.g., acute coronary syndrome), or certain surgical populations (e.g., coronary artery bypass graft surgery) that will likely require ICU care.
Both of these approaches, if applied to the ICU setting, could theoretically result in improved patient outcomes. They could (1) minimize the inefficient, potentially harmful use of trial and error for dosing that could result in sub- or supra-therapeutic drug levels and (2) decrease the time to achieve therapeutic drug levels in patients with diminished physiological reserve. Increased efficiency in drug utilization may result in improved outcomes and reduced costs of care related to adverse events.
Genetics and drug metabolism
Polymorphisms leading to altered drug effect that may have important clinical applications have been identified.63 Some of the common genetic variations for drug-metabolizing enzymes and potential substrates of interest to critical care practitioners are described below. Table 3 lists some examples of genetic alterations for drugs administered in the ICU.
CYP-450 isoenzymes
CYP-450 isoenzymes are responsible for oxidative metabolism of many drugs and endogenous substances. Although primarily located in hepatocytes, they are also found in enterocytes and embedded in cells of the kidney, lungs, and brain.64
CYP2C9
Drugs of interest metabolized by CYP2C9 and encountered in the ICU include warfarin, phenytoin, tolbutamide, glyburide, losartan, candesartan, irbesartan, and some of the non-steroidal anti-inflammatory agents, including celecoxib, diclofenac, ibuprofen, and flurbiprofen.33
Increased effect
The main genetic variants are CYP2C9*2/*3, which may lead to poor metabolism of such substrates as warfarin and non-steroidal anti-inflammatory agents, with associated increased bleeding risk.46,65 Phenytoin is mainly metabolized by CYP2C9.66 Patients with the CYP2C9*2/*3 alleles who are administered phenytoin (frequently administered in the ICU for seizure control) may be at increased risk for drug toxicity if administered standard doses.67 Monitoring drug levels is recommended.
CYP2C19
The CYP2C19 enzyme is responsible for metabolism of drugs such as the proton pump inhibitors omeprazole and lansoprazole, the benzodiazepine diazepam, the antifungal agent voriconazole, and the antiplatelet agent clopidogrel. Because the phenotypes of reduced (thrombosis) or exaggerated (bleeding) platelet inhibition are readily recognized, a large body of information concerning pharmacogenomic drug interactions with commonly prescribed medications and clopidogrel has been described.33,56
Increased effect
It is estimated that 15% of Caucasians and Africans and 30% of the Asian population have the CYP2C19*2 allele, which is most often implicated in loss of function and poor metabolism.23 In the case of the proton pump inhibitors, the presence of this allele may lead to excess acid suppression, which in the ICU has been associated with an increased risk of pneumonia.68 In contrast, omeprazole concentration was significantly elevated in EMs in the presence of clopidogrel - likely through clopidogrel-induced inhibition of CYP2C19.69
Decreased effect
Clopidogrel is widely used as an anti-platelet agent in the management of acute coronary syndromes,70 stroke,71 and other forms of peripheral vascular disease.72 It is a prodrug and requires metabolism, primarily by CYP2C19, to emerge in its active form. Failure to adequately metabolize clopidogrel to its active component may lead to adverse cardiac events73 and recurrent stroke,74 which are potentially devastating complications of inadequate anti-platelet therapy.74,75 Because the phenotype (poor inhibition of platelet function) can be readily identified, the correlation with the genetic contribution to adverse outcomes has received scrutiny.13,76,77 Although not all studies are supportive,78 meta-analyses showed that PMs are prone to early stent occlusion and adverse cardiac events.79,80 Tests are now available to identify PMs (failure to prevent platelet aggregation).24 These tests have been used in randomized trials to guide clopidogrel therapy with some success,81 making the requirement for more costly genotyping less necessary. They can be performed within a reasonable time frame, making the results clinically relevant for application in the ICU. When identified as a PM, the patient should be considered for alternative anti-platelet therapies (e.g., prasugrel).70 Algorithms have been developed using genetic testing to guide optimal drug management.82
CYP2D6
Also known as debrisoquine 4-hydroxylase, CYP2D6 is responsible for the metabolism of ~25% of prescribed drugs.33 The polymorphisms of the CYP2D6 gene have been categorized into four distinct phenotypes: (1) poor metabolizers, which have two defective alleles, thus rendering them incapable of metabolizing the gene substrates; (2) intermediate metabolizers, which have one defective and one normal gene; (3) extensive metabolizers, which have two functional alleles, and (4) ultra metabolizers (UMs), which have multiple copies of the functional gene.57,83,84 This categorization scheme has been adopted in many metabolic studies to describe genetic influences related to allelic distribution. The clinical consequences of drugs eliminated by CYP2D6 vary from toxic drug effects in PMs to inadequate drug effects in UMs.84 Although CYP2D6 appears to be highly polymorphic, testing for its variants CYP2D6*3/*4/*5/*6 has identified approximately 95% of PMs and IMs in a Caucasian population.85 Drugs affected by CYP2D6 polymorphisms commonly administered in the ICU include amitryptyline, codeine, hydrocodone, oxycodone, procainamide, citalopram, venlafaxine, paroxetine, haloperidol, respiridone, ondansetron, metoprolol, carvedilol, alprenolol, timolol, and tramadol.28,83 Dosing guidelines based on genetic testing have been published.86 Ethnic differences have also been observed, with patients of Asian ancestry having a higher proportion of PMs, as observed with haloperidol administration.87
Increased effect
Case reports of severe life-threatening and fatal adverse events have been reported in EMs given standard doses of codeine.84 Codeine is commonly administered to patients in the ICU as part of a multimodal pain regimen, often in combination with acetaminophen. Approximately 10% of codeine is metabolized via CYP2D6 to morphine (the metabolite responsible for analgesia). Therefore, enhanced analgesic effects are evident in EMs who may metabolize codeine more extensively, leading to a potential for increased morphine effect,84 including death in a breast-fed infant.88 Similar observations can be expected when tramadol is employed as it too is metabolized by CYP2D6, and its metabolite confers most of the analgesic effect.84
Decreased effect
Reduced effects of codeine may be seen in PMs of CYP2D6, resulting in diminished concentrations of morphine.89 Patients experiencing nausea and vomiting in the ICU are at increased risk of aspiration pneumonia and may be prescribed 5-hydroxytryptamine type 3 receptor antagonists (e.g., ondansetron) in an attempt to relieve these symptoms. The genetically determined ability to metabolize the drug may be associated with failure to relieve the nausea and vomiting (highest failure rate is in UMs).90 Similar observations have been made for ganisetron and dolasetron.91 Blood pressure control and management of heart failure utilizing carvedilol or metoprolol may be affected by CYP2D6 polymorphisms.92
CYP3A4/5
The genes for the metabolizing enzymes CYP3A4 (liver and upper intestine primarily) and CYP3A5 (liver, intestine, extrahepatic sites)93 are responsible for the genetic coding of enzymes involved in the metabolism of more than 50% of clinically utilized drugs and are subject to genetic variability.33 This includes metabolism of many of the highly utilized drugs employed for therapy in the ICU, including midazolam,94 fentanyl,95 and the calcineurin inhibitors cyclosporine and tacrolimus.28
Increased effect
Midazolam, which is exclusively metabolized by CYP3A4/5, serves as a probe for the function of this drug-metabolizing enzyme.59,96 Variability in the metabolism of midazolam occurs in the ICU97 and may, in part, be mediated by genetic differences in the CYP3A alleles.98,99 The CYP3A5*3 allele is associated with reduced midazolam metabolism and is differentially distributed among ethnic groups.100 In a recent study of ICU patients receiving midazolam, however, the presence of the allele CYP3A5*3/*3 was equally distributed as a percentage of the population at risk and not thought to be contributory to the development of coma or delirium.101
Opioids belonging to the phenypiperidine class (e.g., pethidine, fentanyl, sufentanil, alfentanil) are metabolized by the CYP450 enzyme system and are subject to genetic alterations in drug metabolism. Fentanyl, in particular, is metabolized by CYP3A4/5 and subject to variability in response.102 Alterations in p-glycoprotein (PGP) expression may also play a significant role in fentanyl disposition.103
The calcineurin inhibitors cyclosporine and tacrolimus are utilized to provide immunosuppression in patients undergoing solid organ transplant and are frequently initiated in the ICU following organ transplantation. A large body of studies has examined the effects of CYP3A4/5 polymorphisms on the metabolism of these drugs with variable results.28 For example, in a study of kidney transplant patients, genotyping revealed a significant effect of CYP3A5 polymorphisms on the plasma concentrations of tacrolimus in patients having the CYP3A5*3/*3 allele, thereby requiring less drug for effective immunity.104 No such relation was observed for cyclosporine. Dai et al. also observed a similar differential metabolism rate for patients with CYP3A5*1/*3 vs CYP3A5*3/*3 polymorphisms.105
Certain HMG-CoA reductase inhibitors (also referred to as statins), including lovastatin, atorvastatin, and simvastatin, are primarily metabolized by the CYP3A4/5 enzyme system.28 These agents are frequently encountered in the setting of the cardiovascular ICU, where their ongoing use has been associated with reduced delirium106 and a possible anti-inflammatory effect.107 Although pharmacogenetic differences can be detected between patients expressing CYP3A5*1 (expressors) vs CYP3A5*3 (non-expressors) and their ability to lower lipids,108 the clinical consequences are uncertain.
Uridine diphosphate-glucuronosyltransferase 2B7 (UGT2B7)
Morphine is metabolized by UGT2B7 to morphine-3-glucuronide, which is thought to produce adverse central nervous system (CNS) effects, and morphine-6-glucuronide, a more potent analgesic than the parent compound.49 Differences in genes encoding this enzyme result in alterations in morphine metabolism.
Increased effect
The UGT2B7*2 allele is associated with increased nausea after morphine administration.109 Comparatively, the 840GG and GA alleles have resulted in reduced morphine metabolism (compared with the AA allele).110
Catechol-O-methyltransferase
Decreased effect
Catecholamines, such as epinephrine, are frequently administered in the ICU. They may modulate the effects of epidural analgesics administered for pain management.111 Catecholamines are metabolized by catechol-O-methyltransferase, which is subject to genomic variation. Substitution of methionine for valine at codon 158 of the enzyme (Met/Met) resulted in a three- to four-fold reduction in enzyme activity, which has been shown to result in enhanced morphine analgesia compared with the Val/Val or Val/Met alleles.112
Butrylcholinesterase
Butrylcholinesterase (i.e., pseudocholinesterase) is responsible for the hydrolytic degradation of several drugs administered in the ICU, including succinylcholine,113 the benzylisoquinoline muscle relaxants atracurium and mivacurium,26 and the opioid remifentanil.114
Increased effect
Genetic alterations in enzyme function may lead to a prolonged drug effect. The genetic alterations occur as a result of a point mutation on chromosome 3.113 Approximately 4% of the population may be affected, and point mutations are more commonly observed in patients of European ancestry.46 In addition to the usual (U) variant with normal enzyme activity, there are several variants with altered hydrolyzing effect including the atypical (A), fluoride-resistant (F), and silent (S) types - the latter associated with complete absence of an enzyme effect. There are also variants with a normal enzyme effect but reduced quantity, including the H, J, and K variants.115 The presence of an enzyme effect can be detected by measuring the degree of hydrolysis that occurs in the presence of the enzyme inhibitors dibucaine and fluoride.113 A normal (homozygous typical) dibucaine number is 70-80, whereas a heterozygous atypical number is 50-60, and a homozygous atypical number is less than 30.46 Formal genetic sequencing provides more specific details of the genetic defect, and it is not uncommon for individuals to have more than one genetic variant.115
N-acetyltransferase 2
N-acetyltransferase 2 is responsible for the metabolism of agents such as hydralazine (often used for hypertensive emergencies during the perioperative period) and procainamide (an antiarrythmic agent now seldom used in the ICU).27
Increased effect
Six polymorphisms are associated with a slow-metabolizer phenotype characterized by a prolonged drug effect.116 When used over prolonged periods of time, this phenotype has been characterized by the development of antinuclear antibodies and systemic lupus erythematosus, which is a compelling reason to limit the use of hydralazine.117
Genetics and transport proteins
P-glycoprotein
P-glycoprotein (PGP) is an efflux transporter with excretory and protective functions that is found in barrier and elimination organs, including the choroid plexus, blood-brain barrier, hepatocytes, renal tubular cells, and small intestine. SNPs in the ABCB1 gene have been associated with altered expression and function of PGP, leading to clinically significant changes in drug response.48,103,118,119 Substrates of PGP utilized in the ICU include amitriptyline, clopidogrel, corticosteroids, digoxin, diltiazem, domperidone, azole antifungal agents, lansoprazole, levetiracetam, levofloxacin, loperamide, morphine, pantoprazole, phenobarbital, phenytoin, propranolol, ranitidine, rifampin, HMG-CoA reductase inhibitors, calcineurin inhibitors, and verapamil.118
Increased effect
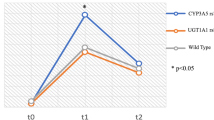
Many opioids (including morphine, methadone, and fentanyl) are subject to PGP transport regulation, limiting accumulation in cells. P-glycoprotein may limit the transport of morphine into the CNS, and variants in its genetic composition may have important clinical effects. Individuals homozygous for the 3435C>T allele (TT carriers) experienced greater pain relief than the heterozygous (CT) type or homozygous wild type (CC).120 Absorption of the PGP substrate digoxin was significantly increased in patients with the 3435C>T and TT alleles compared with the native CC allele.121
Decreased effect
The effect of clopidogrel may, in part, be dependent on PGP. Stakonovic et al. demonstrated significantly reduced plasma concentrations of clopidogrel relative to the active metabolite in patients with the ABCB1 3435TT allele compared with patients having the CC or CT allele.122 This observation has been reported in reviews by other investigators.75,123,124
Genetics and drug targets
Adrenergic receptor
Increased effect
The β-adrenergic receptor (B1AR) blocking agents are commonly used to manage blood pressure and heart rate rhythm disturbances in the ICU. Parvez et al. examined the role that loss of function polymorphism of the β1AR (G389R) played in the response to B1AR blocking agents and determined that the presence of this allele was associated with enhanced response to β1AR blocking agents in patients being treated for atrial fibrillation.125
Decreased effect
Catecholamines are frequently used in the ICU to support patients with hemodynamic deterioration due to a variety of shock states.126 Polymorphisms of the β2-adrenergic receptor (β2AR) have been described.34 Altered responses to β2 agonists used in the management of asthma127,128 or hypotension during regional anesthesia129 have been observed in patients homozygous for the B16 ARG/ARG genotype. Alterations in receptor density in (and hence function of) the heart during cardiac surgery have been shown.130 Functional polymorphisms in the β1AR have been shown to affect the response to β1AR blocking agents employed for the management of heart failure.131 Other studies have found an association between β1-receptor polymorphisms and reduced ability of β-adrenergic receptor blocking agents to lower blood pressure.132,133
Dopamine receptor
Decreased effect
Management of delirium in the ICU frequently requires antipsychotic agents with activity at the dopamine receptor.59,134 Review of studies suggests that subjects with the Ins/Ins allele of the D2 receptor have a better response to antipsychotic agents than those who have the Ins/Del allele.135,136 Patients homozygous for the D2 receptor Taq 1 gene polymorphism had a lower response to haloperidol than heterozygous patients,137 but this observation was not consistent and did not prove to be significant in a subsequent meta-analysis.135
μ Opioid receptor
Decreased effect
Pain management is an important component of compassionate care in the ICU. Morphine, commonly employed in the ICU for pain management, interacts with the μ opioid receptor. Alteration of SNPs (A118 > G118) in the gene OPRM1 has led to genetic variation in receptor function and has been associated with alterations in pain relief.40,120 The polymorphism 118A>G results in less-effective analgesia. Individuals with this variant (GG) require more morphine than individuals with the wild-type variant (AA) and experience more postoperative nausea and vomiting.13,40,138-140 As many as 40% of patients may have a poor response to opioid administration.141 Because the phenotype (pain) is readily observed, investigation of the genetic component to patient variability in pain perception can be determined. It is seldom necessary, however, as most opioids are titrated to effect. In practical terms, when a patient has inadequate pain relief from an opioid, the contribution of genetics to the problem is likely to be small.142 Switching to an alternative analgesic class (e.g., non-steroidal analgesics) may prove beneficial.
Genetics and disease conditions
Sepsis
The heritable characteristic of sepsis is under-appreciated. Heredity may play a greater role in determining the outcome of an episode of sepsis than in outcomes in patients with cardiovascular disease32 or cancer.143 It is commonly observed that the clinical presentation of sepsis (its phenotype characterized by fever, hemodynamic instability, organ dysfunction) is associated with widely variable responses to treatment. In part, it may be due to the wide variability in inciting organisms (viral, bacterial, fungal) and the response to the infection itself.144 Failure of experimental therapies may in part be due to failure to recognize the complexity of the sepsis disease process and our inability to study it correctly.145,146 However, variation in genetic composition may also have a significant role to play.143,144,147-149 For example, innate immunity (the first line of defense against invading organisms) involves three major mechanisms: pathogen recognition, phagocytosis, development of a procoagulant inflammatory response.150 Ongoing genetic research has identified SNPs associated with variability in the innate immune response, including pathogen detection,151-153 inflammation, and coagulation.154,155 Table 4 lists some gene products that have been associated with altered responses to a septic episode.
Decreased effect
Genome-wide association studies suggest that there is alteration in the innate immune system in patients with septic shock.156 Genetic variants in components of the innate immune system - including the pattern recognition receptor toll-like receptor 1 (TLR1),157 toll-like receptor 4 (TLR4),158 toll-like receptor 2 (TLR2),159 migration inhibition factor,160 bacterial permeability increasing protein,161 CD14,153 and plasminogen activator inhibitor162 genes - are associated with differential organ dysfunction and inflammation during a sepsis episode.
Failure to recognize the diversity of response to sepsis as reflected by levels of the inflammatory cytokine tumour necrosis α (TNFα) may be one explanation for the lack of demonstrable efficacy in randomized trials.145,163 For example, in a study of 1057 critically ill patients, mortality was 48.7% in patients homozygous for the TNF-308AA allele compared with those having the TNF-308GA (30.5%) or TNF-308GG (29.5%) allele.164 When response (as reflected by high levels of TNFα) is taken into account, efficacy can be demonstrated.145 The TNF2 polymorphism of the TNFA gene (increased TNFα levels) may be associated with up to a 3.7-fold increased risk of death from septic shock.165 In theory, if specific patient polymorphisms resulting in a variation of TNF production are known to be present at the time of presentation, prescribing an anti-TNF strategy might be targeted at this patient population with a good likelihood of efficacy.
Genome-wide association studies have shown alterations in the adaptive immune response as well.166,167
Hypothetically, improvements in diagnostic precision and recognition of septic patients with distinct biomarkers for inclusion into clinical trials would minimize the likelihood of a type II statistical error.168 In adults, use of organ dysfunction in combination with a requirement for a vasopressor and an elevated lactate level identifies a population with septic shock.169 To date, however, no single biomarker or combination of biomarkers has the requisite sensitivity and specificity to fulfill this criterion for the pediatric population.170 The role that epigenetics may play in altering the host response to sepsis is still a focus of ongoing research.171
Malignant hyperthermia
Increased effect
Although rare, malignant hyperthermia may occur as a result of drug administration in the ICU. Succinylcholine113 and volatile anesthetic agents (used for ICU sedation)172 may precipitate this life-threatening condition, which is characterized by fever, myocardial necrosis, fatal arrhythmias, and acute renal failure. Malignant hyperthermia is inherited as an autosomal dominant condition and manifests as abnormal calcium metabolism at the cellular level.113 The genetic basis for the condition lies in mutations in the RYR1 (ryanodine) and CACNA1S genes.113 Genetic testing for susceptibility is available, and guidelines have been published.173 Management includes use of the ryanodine receptor antagonist dantrolene.174
Drug-induced hypersensitivity reactions
Increased effect
Adverse drug reactions have classically been categorized into type A (those that typically represent a dose response, are predictable based on their pharmacology, and frequently have a genetic component) or type B (idiosyncratic - not dose related or predictable; and the genetic contribution, although often not well characterized, may be important).175 Drug-induced hypersensitivity reactions can range from mild maculopapular exanthema to severe, life-threatening manifestations that require admission to the ICU, such as Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS).176,177
Although possible with other classes of medications, antiepilepsy drugs (AEDs) are the most commonly implicated, with an estimated incidence of severe hypersensitivity reactions of approximately one in 1000 to one in 10,000 patients exposed to AEDs. Associated AEDs are phenytoin, carbamazepine, lamotrigine, and phenobarbital.176,177 Several human leukocyte antigen (HLA) alleles have been associated with hypersensitivity reactions.178 The HLA-B*1502 allele is associated with SJS and TEN following carbamazepine exposure. The prevalence of HLA-B*1502 is highest in the Han Chinese, and that of carbamazepine-induced SJS and TEN is highest in this population as well.179 The HLA-B*1502 allele has also been implicated in phenytoin-induced SJS/TEN in Han Chinese and Thai populations.178,180 Carbamazepine hypersensitivity reactions (fever, eosinophilia) are more frequent in individuals who have at least one of three SNPs localized at the heat shock protein locus (two in HSP70-1 and one in HSP-Hom).175 Antiepilepsy drugs are commonly initiated in the ICU, particularly in neurosurgical and trauma ICUs. Genotyping in such high-risk populations could provide guidance on the appropriate antiepilepsy drug selected for a given ICU patient.
Patients infected with the human immunodeficiency virus (HIV) may be started on the non-nucleoside reverse transcriptase inhibitor (NNRTI) abacavir as part of an antiretroviral therapy drug cocktail. Approximately 5% of patients initiated on abacavir develop a hypersensitivity reaction characterized by fever, malaise, and a rash.181 Re-exposure may be life threatening. The allele HLA-B*5701 has been linked to abacavir hypersensitivity.182 Patients who have HLA-B*5701 in combination with another allele from the heat shock protein family (Hsp70 Hom M4973T) have a greater than 90% chance of developing abacavir hypersensitivity.183 In a randomized clinical trial, subjects randomized to a pre-prescription determination of HLA-B*5701 status and consequent management without abacavir if they screened positive had a 3.4% incidence of hypersensitivity reactions compared with a 7.8% incidence in the group randomized to abacavir as part of the standard-of-care protocol, thus demonstrating the utility of pre-prescription genomic screening.184 Based on these results, many HIV clinics are performing screening for HLA-B*5701 prior to prescribing abacavir. Patients treated with nevirapine (another NNRTI) are also subject to hypersensitivity reactions linked to an HLA class II allele HLA-DRB1*0101, but the severity of the reaction may be dependent on the CD4 count at the time of drug administration.185 The diagnostic possibility of a hypersensitivity reaction should be considered in any patient with HIV who presents with fever and a rash to the ICU, particularly if there has been a recent change in drug therapy.
Genotyping might reduce the incidence of ICU admission of patients with serious cutaneous hypersensitivity reactions. Additionally, genotyping could be utilized to guide AED selection among patients admitted with SJS/TEN. Point-of-care platforms unfortunately do not currently have the ability to perform HLA genotyping.57 A novel approach has been incorporation of an alert to the possible adverse effects and suggestions for genetic testing incorporated into the medical record.186
Cardiac channelopathies
Genetic mutations in the genes encoding for potassium and sodium channels in the heart (so-called channelopathies) may be associated with a predisposition to life-threatening arrhythmias. These arrhythmias may be a reason for ICU admission (sudden cardiac arrest in a previously healthy young individual) or occur as a consequence of interaction between a predisposed individual and drug administration while in the ICU (torsade de pointes).187
There are three major clinical conditions associated with genetic alterations in ion channel function in the heart: long QTc syndrome, catecholaminergic polymorphic ventricular tachycardia (CPVC), and Brugada syndrome.188 For the long QTc syndrome, although 16 genes have been implicated, only three genetic mutations - in the genes KCNQ1(LQT1), KCNHQ (LQT2), SNA5A(LQT3) - are responsible for approximately 75% of cases.187,189,190 The phenotype is sudden cardiac arrest or syncope associated with a prolonged QTc on the electrocardiogram. Specific electrocardiographic abnormalities may help classify the type of mutation.191 A scoring system (Schwartz score)188 has been developed to assess risk for arrhythmias that require further genetic assessment. Treatment is, to a large extent, dependent on the type of mutation - β-blockers for LQT1 and LQT2 and sodium channel blockers (mexiletine) for LQT3 - that should be initiated only under monitored conditions.188,191 Once a proband has been identified, family screening should occur and prophylactic therapy initiated as indicated.
Abnormalities in the RYR2 gene (responsible for intracellular calcium regulation) account for ~50% of the cases of CPVC identified.187,190 Typically, this arrhythmia is precipitated by exercise, but whether the stress-induced tachycardias (e.g., sepsis or postoperatively) often seen in the ICU can precipitate the arrhythmia has not (to our knowledge) been examined.
Brugada syndrome is characterized by a distinctive, coved-type, ST-segment elevation in leads V1 to V3, right ventricular conduction abnormalities, and life-threatening ventricular arrhythmias.190 The syndrome typically occurs in men during the fifth decade of life, at night, and with a family history of sudden cardiac death. Most genetic abnormalities are related to the sodium channel, with SCN5A responsible for ~20% of observed cases. More than 200 SCN5A mutations have been identified to date.
A number of drugs commonly employed in the ICU have been associated with the development of a prolonged QTc and, in some cases, torsade de pointes.192 Examples include amiodarone, erythromycin, clarithromycin, ketoconazole, and haloperidol.
An algorithm for identifying and managing these arrhythmias has been proposed.190
Thromboembolic disease
Decreased effect
The most common inherited thrombophilias include deficiencies in three natural anticoagulant proteins (antithrombin, protein C, protein S) and specific mutations in genes for factor V and prothrombin.193 The first presentation of an inherited defect in the coagulation system may be an acute thrombotic event that necessitates ICU admission. For example, about 2-3% of cases of portal vein thrombosis are due to an inherited coagulation disorder, but the odds of having such an event in the presence of an inherited coagulation defect is more than eight-fold that of normal individuals.194 Up to 30% of known patients with a thrombotic disorder have a recurrence.195 The factor V Leiden mutation involves a single amino acid substitution of glutamine for arginine at position 506 of the factor V gene, leading to activated protein C resistance.196 The prothrombin G20210A mutation represents a single point mutation (G®A at position 20210) in the factor II gene, leading to increased prothrombin concentration.197 There are racial differences in the presence of inherited thrombophilias, with factor V Leiden and prothrombin G20210A mutations more common in Caucasians and protein C and S deficiency more common in Asian populations.198 For example, the most common inherited thrombophilia in the Japanese population is 586A>G (also known as p.Lys196Glu), which accounts for up to 30% of cases, whereas in the Chinese population the most prevalent inherited thrombophilia is due to a protein C mutation (565C>T, p.Arg189Trp).198 Predisposing factors for the development of venous thrombotic events (VTEs) in susceptible patients include immobility, surgery, trauma, cancer, female sex, hormonal therapy, and pregnancy,193,199-201 which are prevalent conditions seen in the ICU and are addressed by routine use of VTE prophylaxis.202 Guidelines have been published concerning testing of patients and their families following an unprovoked VTE episode.203
Increased effect
Warfarin metabolism is subject to modification by genetic abnormalities in the CYP2C9 gene (*2 and *3 alleles vs *1), which is responsible for metabolism of S warfarin, and the VKORC1 gene (GA and AA alleles vs GG alleles), which is responsible for its molecular target.204 A meta-analysis of studies indicated that bleeding risk is increased in subjects with one of these mutations, and dosage adjustment is advised.205 However, a meta-analysis of studies of the utility of dosing based on genetic information to reduce the bleeding risk have produced conflicting results.204,206-210
Because many patients present with a de novo mutation, and there is a large variability in the phenotypic presentation of bleeding, the first presentation of patients with congenital bleeding disorders may be a traumatic event and bleeding of sufficient magnitude to warrant ICU admission.211 Diagnosis under these circumstances can be difficult. If a bleeding disorder is suspected, however, a schema for the diagnostic workup based on commonly available laboratory tests is available.211 Hemophilia A (factor VIII deficiency - F8 gene) and hemophilia B (factor IX deficiency - F9 gene) are common inherited X-linked recessive bleeding disorders resulting in deficient coagulation. There is a large variability in the number of genetic alterations leading to factor VIII and factor IX deficiency.212 Although most commonly observed early in life, the phenotype of bleeding may not manifest until the patient undergoes a surgical procedure or experiences a minor traumatic event that precipitates bleeding of sufficient magnitude to warrant treatment and observation in the ICU.211 Treatment in both instances of factor deficiency is replacement of the missing factor, although the possibility of using gene transfer therapy is becoming a reality.211,213
Altered platelet function due to von Willebrand’s disease is the most common inherited defective platelet function leading to increased bleeding. Von Willebrand’s disease is subclassified into three subtypes: type 1, partial quantitative deficiency; type 2, qualitative deficiency (further subclassified into four disorders); type 3, total deficiency.214 Types 1 and 2 are inherited in an autosomal dominant pattern, whereas type 3 is inherited as an autosomal recessive trait.215 Type 1 accounts for about 70% of cases.211 Management is with DDAVP, factor replacement, and antifibrinolytic agents.211,214
Reviews of the genetics of other rare bleeding disorders are available.216,217
Congestive heart failure
Congestive heart failure with or without arrhythmia is a common reason for ICU admission and is a significant burden on the health care system.218 The genetic contribution to the development of congestive heart failure as a result of cardiomyopathies is increasingly recognized.219 Hypertrophic cardiomyopathies have a genetic basis, and more than 13 genes with over 900 mutations in sarcomere expression have been identified.220 Similarly, the genetic contribution to dilated cardiomyopathies is being unraveled.219 The American Heart Association and the European Society of Cardiology both recognize the genetic component to many of these diseases in their classification schemes.221-223 Genetic testing for the presence of an inherited cardiomyopathy is available224 and may prove useful when making management decisions, such as early insertion of an automated implantable cardioverter-defibrillator.225
Response to heart failure therapies may be altered by genetic variations.226 Reductions in response to β-adrenergic receptor blocking agents was associated with alterations in the BAR ARG389ARG polymorphism in the Beta-Blocker Evaluation Survival Trial (BEST) trial of patients with severe heart failure. Patients with the ARG389GLY polymorphism had a 38% reduction in survival benefit compared with the ARG389ARG group.227 These investigators also showed that a deletion polymorphism in the α-2 receptor (α 2c DEL 322-325) resulted in subjects having a much greater sympatholytic effect to the β-adrenergic receptor blocking agent bucindolol with no effect on mortality compared with wild-type responders, who showed a 30% reduction in mortality.228 In a substudy - the Genetic Risk Assessment of Heart Failure in African Americans (GRAHF) study - of the African American Heart Failure Trial, the effects of subjects carrying the aldosterone synthase gene (CYP11B2) promoter polymorphisms C-344TT/TC or CC were examined.229 Patients with the C-344CC polymorphism (associated with increased aldosterone synthase activity) had significantly poorer event-free survival. The above studies serve as reminders that significant variation may exist in response to heart failure therapies. When an unexpected result does occur, the possibility that the variance has a genetic component should be considered.
Conclusion
Pharmacogenomics and pharmacogenetics in regard to drug therapy is beginning to be applied to patients in the ICU. As technology for rapid discovery of genetic mutations advances and becomes more available, it is possible that in the not too distant future clinicians will have rapidly available, patient-specific, genetic information at the bedside. Already, such application has resulted in improvements in determining the optimal antiplatelet therapy for patients with coronary artery disease. Improvements have also been made in the areas of warfarin dosing, pain management, and immunosuppressive therapy. Furthermore, malignant hyperthermia, inherited cardiac channelopathies, and coagulation disorders of relevance to critical care are being addressed with pharmacogenomics and pharmacogenetics. Given our current inability to predict efficacy and untoward adverse drug effects in a population that lacks the luxury of time for trial and error and has little physiological reserve to compensate for adverse effects, we predict that the application of pharmacogenomics in the ICU will increase and translate into clinically meaningful outcomes. As point-of-care genetic testing becomes more readily available, the genetic contribution of multiple drug therapies will become more predictable, and the combination of medications that is most likely to result in the desired effects for the individual could be chosen.
References
Lander ES, Linton LM, Birren B, et al. Initial sequencing and analysis of the human genome. Nature 2001; 409: 860-921.
Venter JC, Adams MD, Myers EW, et al. The sequence of the human genome. Science 2001; 291: 1304-51.
Ginsburg GS, McCarthy JJ. Personalized medicine: revolutionizing drug discovery and patient care. Trends Biotechnol 2001; 19: 491-6.
Roses AD. Pharmacogenetics and the practice of medicine. Nature 2000; 405: 857-65.
Jameson JL, Longo DL. Precision medicine-personalized, problematic, and promising. N Engl J Med 2015; 372: 2229-34.
Hoehe MR, Kroslak T. Genetic variation and pharmacogenomics: concepts, facts, and challenges. Dialogues Clin Neurosci 2004; 6: 5-26.
McKinnon RA, Ward MB, Sorich MJ. A critical analysis of barriers to the clinical implementation of pharmacogenomics. Ther Clin Risk Manag 2007; 3: 751-9.
Charlab R, Zhang L. Pharmacogenomics: historical perspective and current status. Methods Mol Biol 2013; 1015: 3-22.
Pirmohamed M. Pharmacogenetics: past, present and future. Drug Discov Today 2011; 16: 852-61.
Relling MV, Evans WE. Pharmacogenomics in the clinic. Nature 2015; 526: 343-50.
Meisel C, Gerloff T, Kirchheiner J, et al. Implications of pharmacogenetics for individualizing drug treatment and for study design. J Mol Med (Berl) 2003; 81: 154-67.
Ellsworth RE, Decewicz DJ, Shriver CD, Ellsworth DL. Breast cancer in the personal genomics era. Curr Genomics 2010; 11: 146-61.
Wang Y, Zhao X, Lin J, et al. Association between CYP2C19 loss-of-function allele status and efficacy of clopidogrel for risk reduction among patients with minor stroke or transient ischemic attack. JAMA 2016; 316: 70-8.
Gerdes LU, Gerdes C, Kervinen K, et al. The apolipoprotein epsilon4 allele determines prognosis and the effect on prognosis of simvastatin in survivors of myocardial infarction: a substudy of the Scandinavian simvastatin survival study. Circulation 2000; 101: 1366-71.
Schwinn DA, Podgoreanu M. Pharmacogenomics and end-organ susceptibility to injury in the perioperative period. Best Pract Res Clin Anaesthesiol 2008; 22: 23-37.
Park BK, Pirmohamed M. Toxicogenetics in drug development. Toxicol Lett 2001; 120: 281-91.
Ahasic AM, Christiani DC. Personalized critical care medicine: how far away are we? Semin Respir Crit Care Med 2015; 36: 809-22.
Hertz DL, McLeod HL. Integrated patient and tumor genetic testing for individualized cancer therapy. Clinical Pharmacol Ther 2016; 99: 143-6.
Evans WE, Johnson JA. Pharmacogenomics: the inherited basis for interindividual differences in drug response. Annu Rev Genomics Hum Genet 2001; 2: 9-39.
Caskey CT. Using genetic diagnosis to determine individual therapeutic utility. Annu Rev Med 2010; 61: 1-15.
Veenstra DL, Higashi MK, Phillips KA. Assessing the cost-effectiveness of pharmacogenomics. AAPS PharmSci 2000; 2: E29.
Ensom MH, Chang TK, Patel P. Pharmacogenetics: the therapeutic drug monitoring of the future? Clin Pharmacokinet 2001; 40: 783-802.
Allen JM, Gelot S. Pharmacogenomics in the intensive care unit: focus on potential implications for clinical practice. Recent Pat Biotechnol 2014; 8: 116-22.
Roberts JD, Wells GA, Le May MR, et al. Point-of-care genetic testing for personalisation of antiplatelet treatment (RAPID GENE): a prospective, randomised, proof-of-concept trial. Lancet 2012; 379: 1705-11.
Pirmohamed M, Burnside G, Eriksson N, et al. A randomized trial of genotype-guided dosing of warfarin. N Engl J Med 2013; 369: 2294-303.
Roberts DJ, Hall RI. Drug absorption, distribution, metabolism and excretion considerations in critically ill adults. Expert Opin Drug Metab Toxicol 2013; 9: 1067-84.
Mango R, Vecchione L, Raso B, et al. Pharmacogenomics in cardiovascular disease: the role of single nucleotide polymorphisms in improving drug therapy. Expert Opin Pharmacother 2005; 6: 2565-76.
Gardiner SJ, Begg EJ. Pharmacogenetics, drug-metabolizing enzymes, and clinical practice. Pharmacol Rev 2006; 58: 521-90.
Sweeney BP. Watson and Crick 50 years on. From double helix to pharmacogenomics. Anaesthesia 2004; 59: 150-65.
Evans CH, Rosier RN. Molecular biology in orthopaedics: the advent of molecular orthopaedics. J Bone Joint Surg Am 2005; 87: 2550-64.
Fagerlund TH, Braaten O. No pain relief from codeine…? An introduction to pharmacogenomics. Acta Anaesthesiol Scand 2001; 45: 140-9.
Skibsted S, Bhasin MK, Aird WC, Shapiro NI. Bench-to-bedside review: future novel diagnostics for sepsis - a systems biology approach. Crit Care 2013; 17: 231.
Ingelman-Sundberg M, Sim SC, Gomez A, Rodriguez-Antona C. Influence of cytochrome P450 polymorphisms on drug therapies: pharmacogenetic, pharmacoepigenetic and clinical aspects. Pharmacol Ther 2007; 116: 496-526.
Palmer LJ, Silverman ES, Weiss ST, Drazen JM. Pharmacogenetics of asthma. Am J Respir Crit Care Med 2002; 165: 861-6.
Arledge T, Freeman A, Arbuckle J, Mosteller M, Manasco P. Applications of pharmacogenetics to drug development: the Glaxo Wellcome experience. Drug Metab Rev 2000; 32: 387-94.
Mawhinney LJ, Mabourakh D, Lewis MC. Gender-specific differences in the central nervous system’s response to anesthesia. Transl Stroke Res 2013; 4: 462-75.
Reeve E, Wiese MD, Mangoni AA. Alterations in drug disposition in older adults. Expert Opinion Drug Metab Toxicol 2015; 11: 491-508.
Tansley G, Hall R. Pharmacokinetic considerations for drugs administered in the critically ill. Br J Hosp Med (Lond) 2015; 76: 89-94.
Hines LE, Murphy JE. Potentially harmful drug-drug interactions in the elderly: a review. Am J Geriatr Pharmacother 2011; 9: 364-77.
Ren ZY, Xu XQ, Bao YP, et al. The impact of genetic variation on sensitivity to opioid analgesics in patients with postoperative pain: a systematic review and meta-analysis. Pain Physician 2015; 18: 131-52.
Sunahara S, Urano M, Ogawa M. Genetical and geographic studies on isoniazid inactivation. Science 1961; 134: 1530-1.
Khan JM, Beevers DG. Management of hypertension in ethnic minorities. Heart 2005; 91: 1105-9.
Birkenfeld AL, Jordan J, Hofmann U, et al. Genetic influences on the pharmacokinetics of orally and intravenously administered digoxin as exhibited by monozygotic twins. Clin Pharmacol Ther 2009; 86: 605-8.
Phillips KA, Veenstra DL, Oren E, Lee JK, Sadee W. Potential role of pharmacogenomics in reducing adverse drug reactions: a systematic review. JAMA 2001; 286: 2270-9.
Weinshilboum R. Inheritance and drug response. N Engl J Med 2003; 348: 529-37.
Ama T, Bounmythavong S, Blaze J, Weismann M, Marienau MS, Nicholson WT. Implications of pharmacogenomics for anesthesia providers. AANA J 2010; 78: 393-9.
Gasche Y, Daali Y, Fathi M, et al. Codeine intoxication associated with ultrarapid CYP2D6 metabolism. N Engl J Med 2004; 351: 2827-31.
Evans WE, McLeod HL. Pharmacogenomics-drug disposition, drug targets, and side effects. N Engl J Med 2003; 348: 538-49.
Roberts DJ, Goralski KB, Renton KW, et al. Effect of acute inflammatory brain injury on accumulation of morphine and morphine 3- and 6-glucuronide in the human brain. Crit Care Med 2009; 37: 2767-74.
Thompson MD, Siminovitch KA, Cole DE. G protein-coupled receptor pharmacogenetics. Methods Mol Biol 2008; 448: 139-85.
Jolivot PA, Hindlet P, Pichereau C, et al. A systematic review of adult admissions to ICUs related to adverse drug events. Crit Care 2014; 18: 643.
Kalman LV, Agundez J, Appell ML, et al. Pharmacogenetic allele nomenclature: international workgroup recommendations for test result reporting. Clin Pharmacol Ther 2016; 99: 172-85.
Whirl-Carrillo M, McDonagh EM, Hebert JM, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther 2012; 92: 414-7.
Relling MV, Klein TE. CPIC: Clinical Pharmacogenetics Implementation Consortium of the Pharmacogenomics Research Network. Clin Pharmacol Ther 2011; 89: 464-7.
Roden DM, George AL Jr. The genetic basis of variability in drug responses. Nat Rev Drug Discov 2002; 1: 37-44.
Brockmoller J, Tzvetkov MV. Pharmacogenetics: data, concepts and tools to improve drug discovery and drug treatment. Eur J Clin Pharmacol 2008; 64: 133-57.
Abul-Husn NS, Owusu Obeng A, Sanderson SC, Gottesman O, Scott SA. Implementation and utilization of genetic testing in personalized medicine. Pharmgenomics Pers Med 2014; 7: 227-40.
Beitelshees AL, Voora D, Lewis JP. Personalized antiplatelet and anticoagulation therapy: applications and significance of pharmacogenomics. Pharmgenomics Pers Med 2015; 8: 43-61.
Roberts DJ, Haroon B, Hall RI. Sedation for critically ill or injured adults in the intensive care unit: a shifting paradigm. Drugs 2012; 72: 1881-916.
Kertai MD, Li YJ, Ji Y, et al. Genome-wide association study of new-onset atrial fibrillation after coronary artery bypass grafting surgery. Am Heart J 2015; 170(580-90): e28.
Sawhney V, Brouilette S, Abrams D, Schilling R, O’Brien B. Current genomics in cardiovascular medicine. Curr Genomics 2012; 13: 446-62.
Pulley JM, Denny JC, Peterson JF, et al. Operational implementation of prospective genotyping for personalized medicine: the design of the Vanderbilt PREDICT project. Clin Pharmacol Ther 2012; 92: 87-95.
Swen JJ, Nijenhuis M, de Boer A, et al. Pharmacogenetics: from bench to byte - an update of guidelines. Clin Pharmacol Ther 2011; 89: 662-73.
Michalets EL. Update: clinically significant cytochrome P-450 drug interactions. Pharmacotherapy 1998; 18: 84-112.
Higashi MK, Veenstra DL, Kondo LM, et al. Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA 2002; 287: 1690-8.
Mann MW, Pons G. Various pharmacogenetic aspects of antiepileptic drug therapy: a review. CNS Drugs 2007; 21: 143-64.
Brandolese R, Scordo MG, Spina E, Gusella M, Padrini R. Severe phenytoin intoxication in a subject homozygous for CYP2C9*3. Clin Pharmacol Ther 2001; 70: 391-4.
Patel AJ, Som R. What is the optimum prophylaxis against gastrointestinal haemorrhage for patients undergoing adult cardiac surgery: histamine receptor antagonists, or proton-pump inhibitors? Interact Cardiovasc Thorac Surg 2013; 16: 356-60.
Chen BL, Chen Y, Tu JH, et al. Clopidogrel inhibits CYP2C19-dependent hydroxylation of omeprazole related to CYP2C19 genetic polymorphisms. J Clin Pharmacol 2009; 49: 574-81.
Levine GN, Bates ER, Blankenship JC, et al. ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA Guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2015. DOI:10.1002/ccd.26325.
Passacquale G, Ferro A. Oral antiplatelet agents clopidogrel and prasugrel for the prevention of cardiovascular events. BMJ 2011; 342: d3488.
Robless P, Mikhailidis DP, Stansby G. Systematic review of antiplatelet therapy for the prevention of myocardial infarction, stroke or vascular death in patients with peripheral vascular disease. Br J Surg 2001; 88: 787-800.
Wei YQ, Wang DG, Yang H, Cao H. Cytochrome P450 CYP 2C19*2 associated with adverse 1-year cardiovascular events in patients with acute coronary syndrome. PloS One 2015; 10: e0132561.
McDonough CW, McClure LA, Mitchell BD, et al. CYP2C19 metabolizer status and clopidogrel efficacy in the Secondary Prevention of Small Subcortical Strokes (SPS3) study. J Am Heart Assoc 2015; 4: e001652.
Trenk D, Hochholzer W. Genetics of platelet inhibitor treatment. Br J Clin Pharmacol 2014; 77: 642-53.
Arima Y, Hokimoto S, Akasaka T, et al. Comparison of the effect of CYP2C19 polymorphism on clinical outcome between acute coronary syndrome and stable angina. J Cardiol 2015; 65: 494-500.
Golukhova EZ, Ryabinina MN, Bulaeva NI, Grigorian MV, Kubova M, Serebruany VL. Clopidogrel response variability: impact of genetic polymorphism and platelet biomarkers for predicting adverse outcomes poststenting. Am J Ther 2015; 22: 222-30.
Holmes MV, Perel P, Shah T, Hingorani AD, Casas JP. CYP2C19 genotype, clopidogrel metabolism, platelet function, and cardiovascular events: a systematic review and meta-analysis. JAMA 2011; 306: 2704-14.
Bauer T, Bouman HJ, van Werkum JW, Ford NF, ten Berg JM, Taubert D. Impact of CYP2C19 variant genotypes on clinical efficacy of antiplatelet treatment with clopidogrel: systematic review and meta-analysis. BMJ 2011; 343: d4588.
Zhang L, Yang J, Zhu X, et al. Effect of high-dose clopidogrel according to CYP2C19*2 genotype in patients undergoing percutaneous coronary intervention- a systematic review and meta-analysis. Thromb Res 2015; 135: 449-58.
Samardzic J, Bozina N, Skoric B, et al. CYP2C19*2 genotype influence in acute coronary syndrome patients undergoing serial clopidogrel dose tailoring based on platelet function testing: analysis from randomized controlled trial NCT02096419. Int J Cardiol 2015; 186: 282-5.
Lee JA, Lee CR, Reed BN, et al. Implementation and evaluation of a CYP2C19 genotype-guided antiplatelet therapy algorithm in high-risk coronary artery disease patients. Pharmacogenomics 2015; 16: 303-13.
Zanger UM, Raimundo S, Eichelbaum M. Cytochrome P450 2D6: overview and update on pharmacology, genetics, biochemistry. Naunyn Schmiedebergs Arch Pharmacol 2004; 369: 23-37.
Yiannakopoulou E. Pharmacogenomics and opioid analgesics: clinical implications. Int J Genomics 2015; 2015: 368979.
Sachse C, Brockmoller J, Bauer S, Roots I. Cytochrome P450 2D6 variants in a Caucasian population: allele frequencies and phenotypic consequences. Am J Hum Genet 1997; 60: 284-95.
Crews KR, Gaedigk A, Dunnenberger HM, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for cytochrome P450 2D6 genotype and codeine therapy: 2014 update. Clin Pharmacol Ther 2014; 95: 376-82.
Frackiewicz EJ, Sramek JJ, Herrera JM, Kurtz NM, Cutler NR. Ethnicity and antipsychotic response. Ann Pharmacother 1997; 31: 1360-9.
Koren G, Cairns J, Chitayat D, Gaedigk A, Leeder SJ. Pharmacogenetics of morphine poisoning in a breastfed neonate of a codeine-prescribed mother. Lancet 2006; 368: 704.
Eckhardt K, Li S, Ammon S, Schanzle G, Mikus G, Eichelbaum M. Same incidence of adverse drug events after codeine administration irrespective of the genetically determined differences in morphine formation. Pain 1998; 76: 27-33.
Candiotti KA, Birnbach DJ, Lubarsky DA, et al. The impact of pharmacogenomics on postoperative nausea and vomiting: do CYP2D6 allele copy number and polymorphisms affect the success or failure of ondansetron prophylaxis? Anesthesiology 2005; 102: 543-9.
Janicki PK, Schuler HG, Jarzembowski TM, Rossi M 2nd. Prevention of postoperative nausea and vomiting with granisetron and dolasetron in relation to CYP2D6 genotype. Anesth Analg 2006; 102: 1127-33.
Lymperopoulos A, McCrink KA, Brill A. Impact of CYP2D6 genetic variation on the response of the cardiovascular patient to carvedilol and metoprolol. Curr Drug Metab 2015; 17: 30-6.
Westlind A, Malmebo S, Johansson I, et al. Cloning and tissue distribution of a novel human cytochrome p450 of the CYP3A subfamily, CYP3A43. Biochem Biophys Res Commun 2001; 281: 1349-55.
Kharasch ED, Walker A, Isoherranen N, et al. Influence of CYP3A5 genotype on the pharmacokinetics and pharmacodynamics of the cytochrome P4503A probes alfentanil and midazolam. Clin Pharmacol Ther 2007; 82: 410-26.
Labroo RB, Paine MF, Thummel KE, Kharasch ED. Fentanyl metabolism by human hepatic and intestinal cytochrome P450 3A4: implications for interindividual variability in disposition, efficacy, and drug interactions. Drug Metab Dispos 1997; 25: 1072-80.
Fabre G, Rahmani R, Placidi M, et al. Characterization of midazolam metabolism using human hepatic microsomal fractions and hepatocytes in suspension obtained by perfusing whole human livers. Biochem Pharmacol 1988; 37: 4389-97.
Oldenhof H, de Jong M, Steenhoek A, Janknegt R. Clinical pharmacokinetics of midazolam in intensive care patients, a wide interpatient variability? Clin Pharmacol Ther 1988; 43: 263-9.
Lin YS, Dowling AL, Quigley SD, et al. Co-regulation of CYP3A4 and CYP3A5 and contribution to hepatic and intestinal midazolam metabolism. Mol Pharmacol 2002; 62: 162-72.
Wandel C, Witte JS, Hall JM, Stein CM, Wood AJ, Wilkinson GR. CYP3A activity in African American and European American men: population differences and functional effect of the CYP3A4*1B5’-promoter region polymorphism. Clin Pharmacol Ther 2000; 68: 82-91.
Roy JN, Lajoie J, Zijenah LS, et al. CYP3A5 genetic polymorphisms in different ethnic populations. Drug Metab Dispos 2005; 33: 884-7.
Skrobik Y, Leger C, Cossette M, Michaud V, Turgeon J. Factors predisposing to coma and delirium: fentanyl and midazolam exposure; CYP3A5, ABCB1, and ABCG2 genetic polymorphisms; and inflammatory factors. Crit Care Med 2013; 41: 999-1008.
Yuan R, Zhang X, Deng Q, Wu Y, Xiang G. Impact of CYP3A4*1G polymorphism on metabolism of fentanyl in Chinese patients undergoing lower abdominal surgery. Clin Chim Acta 2011; 412: 755-60.
Park HJ, Shinn HK, Ryu SH, Lee HS, Park CS, Kang JH. Genetic polymorphisms in the ABCB1 gene and the effects of fentanyl in Koreans. Clin Pharmacol Ther 2007; 81: 539-46.
Hesselink DA, van Schaik RH, van der Heiden IP, et al. Genetic polymorphisms of the CYP3A4, CYP3A5, and MDR-1 genes and pharmacokinetics of the calcineurin inhibitors cyclosporine and tacrolimus. Clin Pharmacol Ther 2003; 74: 245-54.
Dai Y, Hebert MF, Isoherranen N, et al. Effect of CYP3A5 polymorphism on tacrolimus metabolic clearance in vitro. Drug Metab Dispos 2006; 34: 836-47.
Page VJ, Davis D, Zhao XB, et al. Statin use and risk of delirium in the critically ill. Am J Respir Crit Care Med 2014; 189: 666-73.
Hall R. Identification of inflammatory mediators and their modulation by strategies for the management of the systemic inflammatory response during cardiac surgery. J Cardiothorac Vasc Anesth 2013; 27: 983-1033.
Kivisto KT, Niemi M, Schaeffeler E, et al. Lipid-lowering response to statins is affected by CYP3A5 polymorphism. Pharmacogenetics 2004; 14: 523-5.
Fujita K, Ando Y, Yamamoto W, et al. Association of UGT2B7 and ABCB1 genotypes with morphine-induced adverse drug reactions in Japanese patients with cancer. Cancer Chemother Pharmacol 2010; 65: 251-8.
Darbari DS, van Schaik RH, Capparelli EV, Rana S, McCarter R, van den Anker J. UGT2B7 promoter variant -840G>A contributes to the variability in hepatic clearance of morphine in patients with sickle cell disease. Am J Hematol 2008; 83: 200-2.
Niemi G, Breivik H. The minimally effective concentration of adrenaline in a low-concentration thoracic epidural analgesic infusion of bupivacaine, fentanyl and adrenaline after major surgery. A randomized, double-blind, dose-finding study. Acta Anaesthesiol Scand 2003; 47: 439-50.
Rakvag TT, Klepstad P, Baar C, et al. The Val158Met polymorphism of the human catechol-O-methyltransferase (COMT) gene may influence morphine requirements in cancer pain patients. Pain 2005; 116: 73-8.
Alvarellos ML, McDonagh EM, Patel S, McLeod HL, Altman RB, Klein TE. PharmGKB summary: succinylcholine pathway, pharmacokinetics/pharmacodynamics. Pharmacogenet Genomics 2015; 25: 622-30.
Glass PS, Hardman D, Kamiyama Y, et al. Preliminary pharmacokinetics and pharmacodynamics of an ultra-short-acting opioid: remifentanil (GI87084B). Anesth Analg 1993; 77: 1031-40.
Levano S, Ginz H, Siegemund M, et al. Genotyping the butyrylcholinesterase in patients with prolonged neuromuscular block after succinylcholine. Anesthesiology 2005; 102: 531-5.
Fretland AJ, Leff MA, Doll MA, Hein DW. Functional characterization of human N-acetyltransferase 2 (NAT2) single nucleotide polymorphisms. Pharmacogenetics 2001; 11: 207-15.
Mansilla-Tinoco R, Harland SJ, Ryan PJ, et al. Hydralazine, antinuclear antibodies, and the lupus syndrome. Br Med J (Clin Res Ed) 1982; 284: 936-9.
Hodges LM, Markova SM, Chinn LW, et al. Very important pharmacogene summary: ABCB1 (MDR1, P-glycoprotein). Pharmacogenet Genomics 2011; 21: 152-61.
Jannetto PJ, Bratanow NC. Pharmacogenomic considerations in the opioid management of pain. Genome Med 2010; 2: 66.
Campa D, Gioia A, Tomei A, Poli P, Barale R. Association of ABCB1/MDR1 and OPRM1 gene polymorphisms with morphine pain relief. Clin Pharmacol Ther 2008; 83: 559-66.
Verstuyft C, Schwab M, Schaeffeler E, et al. Digoxin pharmacokinetics and MDR1 genetic polymorphisms. Eur J Clin Pharmacol 2003; 58: 809-12.
Stokanovic D, Nikolic VN, Konstantinovic SS, et al. P-glycoprotein polymorphism C3435T is associated with dose-adjusted clopidogrel and 2-Oxo-clopidogrel concentration. Pharmacology 2016; 97: 101-6.
Calderon-Cruz B, Rodriguez-Galvan K, Manzo-Francisco LA, et al. C3435T polymorphism of the ABCB1 gene is associated with poor clopidogrel responsiveness in a Mexican population undergoing percutaneous coronary intervention. Thromb Res 2015; 136: 894-8.
Wang XQ, Shen CL, Wang BN, Huang XH, Hu ZL, Li J. Genetic polymorphisms of CYP2C19 2 and ABCB1 C3435T affect the pharmacokinetic and pharmacodynamic responses to clopidogrel in 401 patients with acute coronary syndrome. Gene 2015; 558: 200-7.
Parvez B, Chopra N, Rowan S, et al. A common beta1-adrenergic receptor polymorphism predicts favorable response to rate-control therapy in atrial fibrillation. J Am Coll Cardiol 2012; 59: 49-56.
Avni T, Lador A, Lev S, Leibovici L, Paul M, Grossman A. Vasopressors for the treatment of septic shock: systematic review and meta-analysis. PloS One 2015; 10: e0129305.
Israel E, Drazen JM, Liggett SB, et al. Effect of polymorphism of the beta(2)-adrenergic receptor on response to regular use of albuterol in asthma. Int Arch Allergy Immunol 2001; 124: 183-6.
Liggett SB. Beta(2)-adrenergic receptor pharmacogenetics. Am J Respir Crit Care Med 2000; 161: S197-201.
Smiley RM, Blouin JL, Negron M, Landau R. beta2-adrenoceptor genotype affects vasopressor requirements during spinal anesthesia for cesarean delivery. Anesthesiology 2006; 104: 644-50.
Booth JV, Landolfo KP, Chesnut LC, et al. Acute depression of myocardial beta-adrenergic receptor signaling during cardiopulmonary bypass: impairment of the adenylyl cyclase moiety. Duke Heart Center Perioperative Desensitization Group. Anesthesiology 1998; 89: 602-11.
Johnson JA, Liggett SB. Cardiovascular pharmacogenomics of adrenergic receptor signaling: clinical implications and future directions. Clin Pharmacol Ther 2011; 89: 366-78.
Liu J, Liu ZQ, Tan ZR, et al. Gly389Arg polymorphism of beta1-adrenergic receptor is associated with the cardiovascular response to metoprolol. Clin Pharmacol Ther 2003; 74: 372-9.
Sofowora GG, Dishy V, Muszkat M, et al. A common beta1-adrenergic receptor polymorphism (Arg389Gly) affects blood pressure response to beta-blockade. Clin Pharmacol Ther 2003; 73: 366-71.
Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013; 41: 263-306.
Zhang JP, Lencz T, Malhotra AK. D2 receptor genetic variation and clinical response to antipsychotic drug treatment: a meta-analysis. Am J Psychiatry 2010; 167: 763-72.
Brandl EJ, Kennedy JL, Muller DJ. Pharmacogenetics of antipsychotics. Can J Psychiatry 2014; 59: 76-88.
Schafer M, Rujescu D, Giegling I, et al. Association of short-term response to haloperidol treatment with a polymorphism in the dopamine D(2) receptor gene. Am J Psychiatry 2001; 158: 802-4.
Chou WY, Wang CH, Liu PH, Liu CC, Tseng CC, Jawan B. Human opioid receptor A118G polymorphism affects intravenous patient-controlled analgesia morphine consumption after total abdominal hysterectomy. Anesthesiology 2006; 105: 334-7.
Sia AT, Lim Y, Lim EC, et al. A118G single nucleotide polymorphism of human mu-opioid receptor gene influences pain perception and patient-controlled intravenous morphine consumption after intrathecal morphine for postcesarean analgesia. Anesthesiology 2008; 109: 520-6.
Zhang W, Yuan JJ, Kan QC, Zhang LR, Chang YZ, Wang ZY. Study of the OPRM1 A118G genetic polymorphism associated with postoperative nausea and vomiting induced by fentanyl intravenous analgesia. Minerva Anestesiol 2011; 77: 33-9.
Argoff CE. Clinical implications of opioid pharmacogenetics. Clin J Pain 2010; 26(Suppl 10): S16-20.
Lotsch J, Geisslinger G. A critical appraisal of human genotyping for pain therapy. Trends Pharmacol Sci 2010; 31: 312-7.
Sutherland AM, Walley KR. Bench-to-bedside review: association of genetic variation with sepsis. Crit Care 2009; 13: 210.
van Deventer SJ. Cytokine and cytokine receptor polymorphisms in infectious disease. Intensive Care Med 2000; 26(Suppl 1): S98-102.
Marshall JC. Why have clinical trials in sepsis failed? Trends Mol Med 2014; 20: 195-203.
Cohen J, Vincent JL, Adhikari NK, et al. Sepsis: a roadmap for future research. Lancet Infect Dis 2015; 15: 581-614.
Pinheiro da Silva F, Cesar Machado MC. Personalized medicine for sepsis. Am J Med Sci 2015; 350: 409-13.
LaRosa SP, Opal SM. Biomarkers: the future. Crit Care Clin 2011; 27: 407-19.
Davenport EE, Burnham KL, Radhakrishnan J, et al. Genomic landscape of the individual host response and outcomes in sepsis: a prospective cohort study. Lancet Respir Med 2016; 4: 259-71.
Medzhitov R, Janeway C Jr. Innate immunity. N Engl J Med 2000; 343: 338-44.
Hibberd ML, Sumiya M, Summerfield JA, Booy R, Levin M, Meningococcal Research Group. Association of variants of the gene for mannose-binding lectin with susceptibility to meningococcal disease. Lancet 1999; 353: 1049-53.
Yee AM, Phan HM, Zuniga R, Salmon JE, Musher DM. Association between FcgammaRIIa-R131 allotype and bacteremic pneumococcal pneumonia. Clin Infect Dis 2000; 30: 25-8.
Gibot S, Cariou A, Drouet L, Rossignol M, Ripoll L. Association between a genomic polymorphism within the CD14 locus and septic shock susceptibility and mortality rate. Crit Care Med 2002; 30: 969-73.
Hermans PW, Hibberd ML, Booy R, et al. 4G/5G promoter polymorphism in the plasminogen-activator-inhibitor-1 gene and outcome of meningococcal disease. Lancet 1999; 354: 556-60.
Sapru A, Liu KD, Wiemels J, et al. Association of common genetic variation in the protein C pathway genes with clinical outcomes in acute respiratory distress syndrome. Crit Care 2016; 20: 151.
Pachot A, Lepape A, Vey S, Bienvenu J, Mougin B, Monneret G. Systemic transcriptional analysis in survivor and non-survivor septic shock patients: a preliminary study. Immunol Lett 2006; 106: 63-71.
Wurfel MM, Gordon AC, Holden TD, et al. Toll-like receptor 1 polymorphisms affect innate immune responses and outcomes in sepsis. Am J Respir Crit Care Med 2008; 178: 710-20.
Lorenz E, Mira JP, Frees KL, Schwartz DA. Relevance of mutations in the TLR4 receptor in patients with gram-negative septic shock. Arch Intern Med 2002; 162: 1028-32.
Gao JW, Zhang AQ, Wang X, et al. Association between the TLR2 Arg753Gln polymorphism and the risk of sepsis: a meta-analysis. Crit Care 2015; 19: 416.
Yende S, Angus DC, Kong L, et al. The influence of macrophage migration inhibitory factor gene polymorphisms on outcome from community-acquired pneumonia. FASEB J 2009; 23: 2403-11.
Michalek J, Svetlikova P, Fedora M, et al. Bactericidal permeability increasing protein gene variants in children with sepsis. Intensive Care Med 2007; 33: 2158-64.
Li L, Nie W, Zhou H, Yuan W, Li W, Huang W. Association between plasminogen activator inhibitor-1-675 4G/5G polymorphism and sepsis: a meta-analysis. PloS One 2013; 8: e54883.
Christaki E, Giamarellos-Bourboulis EJ. The beginning of personalized medicine in sepsis: small steps to a bright future. Clin Genet 2014; 86: 56-61.
Watanabe E, Zehnbauer BA, Oda S, Sato Y, Hirasawa H, Buchman TG. Tumor necrosis factor-308 polymorphism (rs1800629) is associated with mortality and ventilator duration in 1057 Caucasian patients. Cytokine 2012; 60: 249-56.
Mira JP, Cariou A, Grall F, et al. Association of TNF2, a TNF-alpha promoter polymorphism, with septic shock susceptibility and mortality: a multicenter study. JAMA 1999; 282: 561-8.
Tang BM, McLean AS, Dawes IW, Huang SJ, Lin RC. The use of gene-expression profiling to identify candidate genes in human sepsis. Am J Respir Crit Care Med 2007; 176: 676-84.
Tang BM, McLean AS, Dawes IW, Huang SJ, Lin RC. Gene-expression profiling of peripheral blood mononuclear cells in sepsis. Crit Care Med 2009; 37: 882-8.
Opal SM, Dellinger RP, Vincent JL, Masur H, Angus DC. The next generation of sepsis clinical trial designs: what is next after the demise of recombinant human activated protein C? Crit Care Med 2014; 42: 1714-21.
Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a New definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315: 775-87.
Wong HR. Genetics and genomics in pediatric septic shock. Crit Care Med 2012; 40: 1618-26.
Cornell TT, Wynn J, Shanley TP, Wheeler DS, Wong HR. Mechanisms and regulation of the gene-expression response to sepsis. Pediatrics 2010; 125: 1248-58.
Sackey PV, Martling CR, Granath F, Radell PJ. Prolonged isoflurane sedation of intensive care unit patients with the Anesthetic Conserving Device. Crit Care Med 2004; 32: 2241-6.
Hopkins PM, Ruffert H, Snoeck MM, et al. European Malignant Hyperthermia Group guidelines for investigation of malignant hyperthermia susceptibility. Br J Anaesth 2015; 115: 531-9.
Schneiderbanger D, Johannsen S, Roewer N, Schuster F. Management of malignant hyperthermia: diagnosis and treatment. Ther Clin Risk Manag 2014; 10: 355-62.
Pirmohamed M. Pharmacogenetics of idiosyncratic adverse drug reactions. Handb Exp Pharmacol 2010; 196: 477-91.
Bloch KM, Sills GJ, Pirmohamed M, Alfirevic A. Pharmacogenetics of antiepileptic drug-induced hypersensitivity. Pharmacogenomics 2014; 15: 857-68.
Grover S, Kukreti R. HLA alleles and hypersensitivity to carbamazepine: an updated systematic review with meta-analysis. Pharmacogenet Genomics 2014; 24: 94-112.
Rufini S, Ciccacci C, Politi C, Giardina E, Novelli G, Borgiani P. Stevens-Johnson syndrome and toxic epidermal necrolysis: an update on pharmacogenetics studies in drug-induced severe skin reaction. Pharmacogenomics 2015; 16: 1989-2002.
Patnaik M, Renda MJ, Athanasiou MC, Reed CR. The role of pharmacogenetics in treating central nervous system disorders. Exp Biol Med (Maywood) 2008; 233: 1504-9.
Leckband SG, Kelsoe JR, Dunnenberger HM, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for HLA-B genotype and carbamazepine dosing. Clin Pharmacol Ther 2013; 94: 324-8.
Phillips EJ. The pharmacogenetics of antiretroviral therapy. Curr Opin HIV AIDS 2006; 1: 249-56.
Mallal S, Nolan D, Witt C, et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet 2002; 359: 727-32.
Martin AM, Nolan D, Gaudieri S, et al. Predisposition to abacavir hypersensitivity conferred by HLA-B*5701 and a haplotypic Hsp70-Hom variant. Proc Natl Acad Sci USA 2004; 101: 4180-5.
Mallal S, Phillips E, Carosi G, et al. HLA-B*5701 screening for hypersensitivity to abacavir. N Engl J Med 2008; 358: 568-79.
Martin AM, Nolan D, James I, et al. Predisposition to nevirapine hypersensitivity associated with HLA-DRB1*0101 and abrogated by low CD4 T-cell counts. AIDS 2005; 19: 97-9.
Goldspiel BR, Flegel WA, DiPatrizio G, et al. Integrating pharmacogenetic information and clinical decision support into the electronic health record. J Am Med Inform Assoc 2014; 21: 522-8.
Abriel H, Zaklyazminskaya EV. Cardiac channelopathies: genetic and molecular mechanisms. Gene 2013; 517: 1-11.
Schwartz PJ, Ackerman MJ, George AL Jr, Wilde AA. Impact of genetics on the clinical management of channelopathies. J Am Coll Cardiol 2013; 62: 169-80.
Baskar S, Aziz PF. Genotype-phenotype correlation in long QT syndrome. Glob Cardiol Sci Pract 2015; 2015: 26.
John RM, Tedrow UB, Koplan BA, et al. Ventricular arrhythmias and sudden cardiac death. Lancet 2012; 380: 1520-9.
Patel C, Antzelevitch C. Pharmacological approach to the treatment of long and short QT syndromes. Pharmacol Ther 2008; 118: 138-51.
Khan IA. Clinical and therapeutic aspects of congenital and acquired long QT syndrome. Am J Med 2002; 112: 58-66.
Varga EA, Kujovich JL. Management of inherited thrombophilia: guide for genetics professionals. Clin Genet 2012; 81: 7-17.
Qi X, Ren W, De Stefano V, Fan D. Associations of coagulation factor V Leiden and prothrombin G20210A mutations with Budd-Chiari syndrome and portal vein thrombosis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2014; 12(1801-12): e7.
Heit JA. Predicting the risk of venous thromboembolism recurrence. Am J Hematol 2012; 87(Suppl 1): S63-7.
Voorberg J, Roelse J, Koopman R, et al. Association of idiopathic venous thromboembolism with single point-mutation at Arg506 of factor V. Lancet 1994; 343: 1535-6.
Poort SR, Rosendaal FR, Reitsma PH, Bertina RM. A common genetic variation in the 3’-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood 1996; 88: 3698-703.
Yin T, Miyata T. Dysfunction of protein C anticoagulant system, main genetic risk factor for venous thromboembolism in Northeast Asians. J Thromb Thrombolysis 2014; 37: 56-65.
Roach RE, Cannegieter SC, Lijfering WM. Differential risks in men and women for first and recurrent venous thrombosis: the role of genes and environment. J Thromb Haemost 2014; 12: 1593-600.
ESHRE Capri Workshop Group. Venous thromboembolism in women: a specific reproductive health risk. Hum Reprod Update 2013; 19: 471-82.
Bleker SM, Coppens M, Middeldorp S. Sex, thrombosis and inherited thrombophilia. Blood Rev 2014; 28: 123-33.
Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141(2 Suppl): e195S-226S.
De Stefano V, Rossi E. Testing for inherited thrombophilia and consequences for antithrombotic prophylaxis in patients with venous thromboembolism and their relatives. A review of the Guidelines from Scientific Societies and Working Groups. Thromb Haemost 2013; 110: 697-705.
Johnson JA, Cavallari LH. Warfarin pharmacogenetics. Trends Cardiovasc Med 2015; 25: 33-41.
Yang J, Chen Y, Li X, et al. Influence of CYP2C9 and VKORC1 genotypes on the risk of hemorrhagic complications in warfarin-treated patients: a systematic review and meta-analysis. Int J Cardiol 2013; 168: 4234-43.
Xu H, Xie X, Wang B, et al. Meta-analysis of efficacy and safety of genotype-guided pharmacogenetic dosing of warfarin. Int J Cardiol 2014; 177: 654-7.
Tang Q, Zou H, Guo C, Liu Z. Outcomes of pharmacogenetics-guided dosing of warfarin: a systematic review and meta-analysis. Int J Cardiol 2014; 175: 587-91.
Stergiopoulos K, Brown DL. Genotype-guided vs clinical dosing of warfarin and its analogues: meta-analysis of randomized clinical trials. JAMA Intern Med 2014; 174: 1330-8.
Liao Z, Feng S, Ling P, Zhang G. Meta-analysis of randomized controlled trials reveals an improved clinical outcome of using genotype plus clinical algorithm for warfarin dosing. J Thromb Thrombolysis 2015; 39: 228-34.
Franchini M, Mengoli C, Cruciani M, Bonfanti C, Mannucci PM. Effects on bleeding complications of pharmacogenetic testing for initial dosing of vitamin K antagonists: a systematic review and meta-analysis. J Thromb Haemost 2014; 12: 1480-7.
Bhat R, Cabey W. Evaluation and management of congenital bleeding disorders. Emerg Med Clin North Am 2014; 32: 673-90.
Rydz N, Leggo J, Tinlin S, James P, Lillicrap D. The Canadian “National Program for hemophilia mutation testing” database: a ten-year review. Am J Hematol 2013; 88: 1030-4.
High KH, Nathwani A, Spencer T, Lillicrap D. Current status of haemophilia gene therapy. Haemophilia 2014; 20(Suppl 4): 43-9.
Favaloro EJ, Bodo I, Israels SJ, Brown SA. von Willebrand disease and platelet disorders. Haemophilia 2014; 20(Suppl 4): 59-64.
Orfanakis A, Deloughery T. Patients with disorders of thrombosis and hemostasis. Med Clin North Am 2013; 97: 1161-80.
Peyvandi F, Bolton-Maggs PH, Batorova A, De Moerloose P. Rare bleeding disorders. Haemophilia 2012; 18(Suppl 4): 148-53.
Palla R, Peyvandi F, Shapiro AD. Rare bleeding disorders: diagnosis and treatment. Blood 2015; 125: 2052-61.
Davidson PM, Newton PJ, Tankumpuan T, Paull G, Dennison-Himmelfarb C. Multidisciplinary management of chronic heart failure: principles and future trends. Clin Ther 2015; 37: 2225-33.
Mestroni L, Merlo M, Taylor MR, Camerini F, Sinagra G. Heart failure and personalized medicine. J Cardiovasc Med (Hagerstown) 2011; 12: 6-12.
Wang L, Seidman JG, Seidman CE. Narrative review: harnessing molecular genetics for the diagnosis and management of hypertrophic cardiomyopathy. Ann Intern Med 2010. DOI:10.7326/0003-4819-152-8-201004200-00008.
Maron BJ, Towbin JA, Thiene G, et al. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 2006; 113: 1807-16.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J Heart 2016; 118: 891-975.
Writing Committee Members; Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128: e240-327.
Hershberger RE, Lindenfeld J, Mestroni L, et al. Genetic evaluation of cardiomyopathy - a Heart Failure Society of America practice guideline. J Card Fail 2009; 15: 83-97.
Meune C, Van Berlo JH, Anselme F, Bonne G, Pinto YM, Duboc D. Primary prevention of sudden death in patients with lamin A/C gene mutations. N Engl J Med 2006; 354: 209-10.
McNamara DM. Emerging role of pharmacogenomics in heart failure. Curr Opin Cardiol 2008; 23: 261-8.
Liggett SB, Mialet-Perez J, Thaneemit-Chen S, et al. A polymorphism within a conserved beta(1)-adrenergic receptor motif alters cardiac function and beta-blocker response in human heart failure. Proc Natl Acad Sci USA 2006; 103: 11288-93.
Bristow MR, Murphy GA, Krause-Steinrauf H, et al. An alpha2C-adrenergic receptor polymorphism alters the norepinephrine-lowering effects and therapeutic response of the beta-blocker bucindolol in chronic heart failure. Circ Heart Fail 2010; 3: 21-8.
McNamara DM, Tam SW, Sabolinski ML, et al. Aldosterone synthase promoter polymorphism predicts outcome in African Americans with heart failure: results from the A-HeFT Trial. J Am Coll Cardiol 2006; 48: 1277-82.
Funding
There are no funding sources or commercial or non-commercial affiliations that are or may be perceived to be a conflict of interest.
Author contributions
Meghan MacKenzie and Richard Hall contributed substantially to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data; and drafting the article.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
MacKenzie, M., Hall, R. Pharmacogenomics and pharmacogenetics for the intensive care unit: a narrative review. Can J Anesth/J Can Anesth 64, 45–64 (2017). https://doi.org/10.1007/s12630-016-0748-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-016-0748-1