Abstract
Attention to nutrition continues to grow. The recent surge in interest has included widening agreement on two major issues: first, nutrition goals cannot be achieved through targeted actions alone; nutrition-sensitive interventions are needed as well. Second, the multiple actions required to address all forms of malnutrition through the lifecycle cannot be proxied by a single target or metric. Although the Millennium Development Goals included one concrete measure of nutrition (children underweight), the post-2015 Sustainable Development Goals will include multiple measures that better inform a diversity of policy and programming actions. This suggests a need for improved understanding of how multiple forms of malnutrition are linked, how public investments may affect one form of malnutrition but possibly not others, and how best to measure progress on multiple nutrition fronts, including through nutrition-sensitive actions, such as investments in agriculture. This paper proposes a composite index that highlights the state of nutrition across six separate nutrition goals endorsed by the World Health Assembly in 2012, allowing for ranking (comparison among countries) and monitoring of change (within countries) over time. Establishing an index that captures gains or losses in nutrition across all six goals simultaneously highlights the complexity of nutrition problems and required solutions. Such an index can be used to track progress towards goals set for 2025, but also support dialogue on the individual index components and how investments should be prioritized for maximum impact.
Similar content being viewed by others
Introduction
Background
The world faces many different food-related nutrition and health problems, including obesity and diet-related non-communicable diseases as well as undernutrition and widespread vitamin and mineral deficiencies. Universal access to diverse high quality diets has to be a key element of policies and targeted interventions that seek to tackle all such forms of malnutrition (Global Panel 2014). Quality diets represent the bridge between policymakers focused on food and agriculture and the separate community of public health and nutrition specialists, both of which are paying increased attention to the complexity of global nutrition problems. The Scaling Up Nutrition (SUN 2010) movement, the 2013 Lancet series papers on maternal and child nutrition (which included attention to nutrition-sensitive agriculture), the World Health Assembly’s endorsement in 2012 of a Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition and the second International Conference on Nutrition in 2014, all reflect an increasing convergence of thinking on priority nutrition problems and growing agreement on evidence-based solutions that span a range of important sectors. An important element of this revitalized agenda has been recognition that because there are many kinds of nutrition concerns through the lifecycle, no single policy or program can alone resolve them all. The corollary of such recognition is that nutrition problems cannot be distilled into a single metric. Just as ‘health’ is not defined as the absence of a single disease or medical condition, ‘nutrition’ is about more than the absence of one or more manifestations of nutrient deficiency.
The complexity of nutrition nomenclature has hindered the international community for many decades as it sought to promote government and donor investments. The Millennium Development Goals (MDGs) were notably weak in this regard; that is, they were based on a single metric of undernutrition (the prevalence rate of children underweight) to represent all forms of nutritional compromise. As that metric was embedded within MDG1, which also included multiple measures of poverty and food supply, the nutrition target became largely invisible (UNHLP 2013). For example, there was much self-congratulation in 2014 when it was reported that MDG1 had been achieved several years ahead of schedule (World Bank 2014). However, success in that case was only measured in relation to the poverty reduction target of MDG1; progress on the nutrition target (halving the proportion of children under 5 years of age who are underweight) will not be met by countless developing countries despite being a component of MDG1 (UN 2014; 2005).
The slow and uneven progress on nutrition across nations has raised concern among those tasked with defining new goals for the post-2015 era (IFPRI 2014). The UN’s High Level Panel, for example, argued that poverty should be seen not only in economic terms but also in terms of malnutrition (UNHLP 2013). They therefore recommended that three separate measure of child undernutrition be included to track progress on “food security and good nutrition” in the post-2015 era. Going further still, the World Health Assembly’s (WHA) comprehensive plan proposed six separate nutrition targets based on their individual and collective epidemiological and public health relevance. The WHA’s message was that nutrition goals cannot be met in piecemeal or one-at-a time fashion – they are all important and must all be addressed immediately (De Onis et al. 2013). As most governments regularly track few if any nationally representative nutrition indicators, very few pay attention to the range of manifestations of malnutrition that affects their country. As a result, most nutrition policies and strategies are either blunt instruments (poorly tailored to address the multiple forms of malnutrition found in most countries) or too broadly cast to offer concrete guidance on the many policy and program levers that can be marshalled to tackle nutrition problems.
This paper presents a new single-metric index of nutrition that captures ‘net’ progress across all six WHA targets: the Net State of Nutrition Index (NeSNI). This metric adopts the methodological approach promoted by the Human Development Index because it is widely understood, transparent, easy to use and has been influential in highlighting the relative rankings of nations for several decades. Collating data from 89 low and middle income developing countries (those with standardized and comparable data across all six indicators), the NeSNI presents a) individual country outcomes, b) how they rank against all other nations, and c) how groups of countries cluster together in terms of the similarity of their nutrition problems. The paper has four sections. The first, following this introduction, lays out key aspects of the current global nutrition situation as a basis for explaining the targets set by the World Health Assembly and adopted as part of the Second International Conference on Nutrition Framework (FAO/WHO 2014). It then describes existing indices or scores for tracking nutrition globally, and how the new proposed index is different. A third section explains the methodological approach used here and sources of data. The fourth presents results and discusses implications of the results in terms of data quality and policy relevance. A final section offers conclusions and recommendations.
Global problems and global goals
Recent estimates suggest that 161 million children under the age of 5 years are stunted worldwide, at least 51 million suffer wasting, while another 42 million children are overweight or obese (Black et al. 2013; UNSCN 2014).Footnote 1 In addition, there are billions of people (children and adults) deficient in one or more vitamins or minerals.Footnote 2 Faced with such significant challenges, governments around the world have been urged by the United Nations and by nutrition champions to commit the resources and political vigor necessary to significantly improve nutrition globally by 2025. Many governments have made public their intent to bring about major changes, with over 50 developing nations signing up to a global platform of action under the Scaling Up Nutrition movement (SUN 2010). Many more signed up to the Declaration of the Second International Conference on Nutrition (FAO/WHO 2014). In other words, most developing country governments are committing themselves to meeting multiple nutrition targets in the coming decades, and such targets are framed by the six indicators endorsed by the WHA (WHO 2012). To be achieved by 2025, those WHA targets are as follows:
-
1.
A 40 % reduction of the global number of children under five who are stunted (against 2010 global estimates);
-
2.
A 50 % reduction of anaemia in women of reproductive age;
-
3.
A 30 % reduction of low birth weight;
-
4.
No increase in childhood overweight;
-
5.
Increase the rate of exclusive breastfeeding in the first 6 months up to at least 50 %.
-
6.
Reduce and maintain childhood wasting to less than 5 %.
These six targets pay attention to chronic as well as acute conditions, to undernutrition as well as obesity, indirectly to quality of diet issues (framed by the micronutrient status of children and adults), and to birth outcomes (relating to maternal and in utero nutritional status of the fetus). Thus, the WHA targets frame ‘nutrition’ broadly as a multi-faceted challenge that includes several kinds of problems manifesting at different periods of the lifecycle.
Each of these relates in different ways not just to health but to the food and agricultural systems underpinning developing and middle income country diets. For example, the first indicator (child stunting) relates to the prevalence (proportion) of children under 5 years of age who are shorter for their age in relation to a WHO-defined child growth median (WHO 2006). Stunting has become the ‘metric of choice’ for a growing number of decision makers and analysts in the nutrition and public health domain who seek a measure that reflects long-term (chronic) nutritional compromise. Roughly one in four children under five were stunted in 2013, and 80 % of those 161 million stunted children live in just 14 countries (IFPRI 2014). Most of those countries have large populations still reliant on agriculture (as producers or as people engaged in rural service industries), and agricultural productivity contributes significantly to the incomes and food choices of the poor. The process of stunting typically starts early (at birth or even in utero) and is associated with impaired physiological and cognitive development, both of which can have long-lasting consequences for learning, productivity, and life-time earnings (Hoddinott et al. 2013). Stunting starts in utero with undernourished mothers whose diets and health are poor, and who may be heavily engaged in the labor of agriculture or other income-earning activities that generate relatively limited purchasing power.
Severe and moderate stunting carry elevated morbidity and mortality risks that should not be ignored (Black et al. 2013). A 40 % reduction in stunting by 2025 (from 2012) would represent an average annual relative reduction (ARR) rate of 4 %; between 1995 and 2010 the rate of reduction for 100 nations averaged 1.8 % per year (De Onis et al. 2013). In other words, this target alone represents a significant challenge. It has been noted that even if all evidence-based targeted interventions known to be effective in tackling undernutrition were implemented at scale (90 % coverage) in the countries of highest burden, only 20 % of stunting would be resolved (Bhutta et al. 2013). While the investments needed to make this happen are essential, the data suggest a role for non-health based nutrition-sensitive actions in agriculture, water and sanitation, social protection systems, etc. to resolve a greater share of the stunting problem worldwide (UNSCN 2014).Footnote 3
Anaemia, the second indicator, focuses not on children but on the prevalence of women of reproductive age suffering iron deficiency anaemia (defined as a haemoglobin level below 120 g/l (WHO (World Health Organization) 2008b). Roughly 120,000 deaths per year are attributed to iron deficiency (Lim et al. 2012), while it is also highlighted as a “substantial cause” of disability-adjusted life years (DALYs) lost due to anaemia (Murray et al. 2012). Resolving anaemia has proven to be difficult, despite interventions such as iron and folic acid supplementation of adult women, iron fortification of grain flours, multi-micronutrient fortification of commercial foods or supplementation via powders (UNICEF 2006). Biofortification (conventional cross-breeding and/or genetic modification for high iron traits) of crops such as beans, cassava, wheat and pearl millet is increasingly promoted as a food-based approach to addressing anemia through the diet (Petry et al. 2014). However, even with all kinds of interventions combined, a halving of the global rate of iron deficiency anaemia by 2025 would require an ARR of 5.3 %. As individual country experiences, where reduction has been sustained over many years, have been in the range of 4 to 8 % per year the target rate is possible; but it will require significant and sustained investments across many sectors to be achieved (WHO 2013).
The third measure, Low Birth Weight (LBW), represents weight at or near birth below 2,500 g (WHO/UNICEF 2005). Low birth weight usually represents poor nutrition and health of both mother and baby, and can result from birth small for gestational age (SGA) or born prematurely and small. It has been found that a considerable share of child stunting by age 3 can be attributed to SGA and other perinatal complications associated with LBW (Black et al. 2013). Both SGA and premature birth can be related to high workload of women (in agriculture or other activities requiring heavy lifting) late in their pregnancy. Indeed, interventions in agriculture that raise demand for household labour, particularly of women, may increase productivity and output at the expense of women’s opportunity costs of time for childcare, own-health seeking and even commitment to exclusive breastfeeding. Such trade-offs need to be better understood as a 30 % reduction in LBW from a 2006–2010 base period up to 2025 would require an ARR of almost 4 %. Such reductions have been reported from several countries in Africa and Latin America, but so far few countries of South Asia (where half the world’s cases of LBW are found) have matched such gains (WHO 2013).
Overweight, the fourth WHA indicator, relates to an equally important threat to child nutrition and health; namely, overweight. The indicator focuses on the prevalence of children under the age of five who are heavier in relation to their height (more than two standard deviations) in relation to the WHO benchmark child growth median (WHO 2006). Attention to overweight and obesity in global nutrition targets is a new development. The UN High Level Panel tasked with proposing post-2015 Sustainable Development Goals discussed the growing public health and economic costs linked to overweight and obesity, but it did not include any metric for such conditions among their proposed targets for nutrition. Rates of overweight continue to rise across all regions of the world: already by 2011, roughly 69 % of the global burden of overweight children under five was in low- and middle-income countries (UNICEF 2013). This is significant, as overweight and obesity are associated with 3.4 million deaths annually and with 3.8 % of disability-adjusted life-years (DALYs) worldwide (Ng et al. 2014). The association between early child under nutrition and later overweight and obesity is important in this regard. As noted by Sunguya et al. (2014), “children born with low weight or those who succumb to undernutrition in their early childhood have a high risk of early adulthood obesity and NCDs, including diabetes and heart diseases.” Hence the importance of taking an holistic view of nutrition, particularly in countries undergoing a rapid economic, dietary and nutrition transition (Uauy et al. 2011; Norris et al. 2012).
However, there are three main problems relating to this particular metric of (over)nutrition: a) very few developing countries systematically monitor trends in child overweight, b) there is as yet no empirically-documented intervention that has prevented an increase in overweight and obesity at a population-wide level anywhere in the world (which also represents an important opportunity for innovation and better documentation of potentially impactful practices), and c) there is a strong statistical inverse association over the long run between poverty reduction per capita in developing countries and the rise of child overweight – that is, while a policy of support for agriculture in poorer economies, for example, may be associated with a decline in stunting over time, that same policy may be associated with an increase in child obesity (Webb and Block 2012).Footnote 4 That association appears to be driven by rapidly changing diets associated with growth in disposable incomes, urbanization and lifestyle changes (UNSCN 2014). This suggests that the WHA target of a 0 % increase in overweight in the coming decade will be hard to achieve.
Exclusive breastfeeding during the first 6 months of a child’s life, the fifth indicator, is also a challenge to measure as it seeks to enumerate infants 0 to 5.9 months who were only fed breast milk in the previous 24 h (WHO 2008a). The WHA goal is to increase the global prevalence of exclusive breastfeeding to more than 50 %, up from 37 % in the 2006–2010 period (WHO 2013). The ARR to achieve such a goal would be around 2.3 %, which has certainly been exceeded by many countries in the past and hence is relatively achievable (UNICEF 2013). However, mothers require appropriate information and support to be able to exclusively breastfeed for 6 full months. That can be a challenge in rural areas (where many women engaged in agriculture leave their children at home in the care of siblings) as well as in urban settings (where many women work far from home in jobs that are also unconducive to the presence of an infant) (FAO 2011).
Finally, the sixth WHA indicator is child wasting, measured as the prevalence of children under five who weigh too little for their length (weight-for-height less than two standard deviations below the child growth median (WHO 2006)). While wasting has long been seen as a problem linked to humanitarian emergencies (rather than a development issue), it is increasingly realized that even moderate and mild forms of wasting carry a high mortality risk, and that the number of wasted children in countries not affected by humanitarian disasters is large (Bhutta et al. 2013; Webb et al. 2014). For example, during the second half of the 2000s, 53 countries reported wasting rates exceeding 5 % (WHO 2013). While, there are proven interventions for treatment which, if taken to scale, would significantly reduce both prevalence rates and incidence (Bhutta et al. 2013), wasting has been rising in many parts of Africa and some areas of South Asia in recent years (IFPRI 2014). While dietary inadequacy does play a role in wasting, major drivers also include diseases, poor hygiene, and lack of health care. In other words, the multiple causality involved in wasting demands a multisectoral response.
The six WHA targets are presented in no order of priority; they represent a combined set of goals that together acknowledge the compounding of effects of multiple burdens of malnutrition.Footnote 5 The Declaration of the second International Conference on Nutrition made explicit that malnutrition should be understood as including “undernutrition, micronutrient deficiencies, overweight and obesity, as well as non-communicable diseases” (FAO/WHO 2014). It also acknowledged that governments cannot afford to pick and choose which form of malnutrition they want to focus on, as “different forms of malnutrition co-exist within most countries.” (FAO/WHO 2014) For this reason, a number of attempts have been made to derive multi-indicator scores or indices of nutrition to help encourage policymakers to think more holistically when they prioritize investments relevant to nutrition.
Multi-indicator nutrition scores
While the international community has come to accept the need for a more comprehensive, multifaceted approach to dealing with the complexity of nutrition throughout the lifecycle (UNHLP 2013; Habicht and Pelto 2014; Black et al. 2013), it remains unclear how progress (or lack thereof) will be adequately documented. Several options have been proposed, aside from tracking progress towards MDG1 (Fanzo and Pronyk 2011). These include a Global Nutrition Index (Rosenbloom et al. 2008), an International Nutrition Index (Wiesmann et al. 2000) which has become more widely known as the Global Hunger Index (von Grebmer et al. 2013), and the Global Hidden Hunger Index (Muthayya et al. 2013). Each of these is briefly considered below.
Rosenbloom et al. (2008) proposed a composite index to measure “overall nutrition status, and not just hunger.” This was an important step in seeking to standardize global metrics for nutrition (rather than any poorly defined concept of ‘hunger’), in such a way that data could be helpful to, and guide, national policies. Modeled on the Human Development Index, the authors used three measures relating to what they called a) nutritional deficit, b) nutritional excess, and c) food security. The metric for ‘nutritional deficit’ was an age-standardized statistic for disability adjusted life years (DALYs) lost “due to nutritional factors” (Rosenbloom et al. 2008). In practical terms, this means using the estimated DALYs lost per 100,000 population attributable to protein-energy malnutrition and micronutrient deficiency.
This was a novel approach, but it relied on modelled estimates of DALYs lost due to deficiencies rather than actually measured deficiencies, and the micronutrient deficiencies included in the estimates was not reported.Footnote 6 The second of the three measures (excess) refers obliquely to rates of obesity — in this case not of children (because the 2005 global dataset for obesity used did not have sufficient data on children), but for women aged 15 to 100 years with a Body Mass Index (BMI) greater than or equal to 30.Footnote 7 The third metric, ‘food security’, used the much-critiqued FAO metric of chronic undernourishment, which represents a national food disappearance accounting approach often used as a proxy for nutritional deficiency (Smith and Haddad 2014). The three indicators were combined (equally weighted), and scaled from 0 to 1 in order to achieve standardization. The scaled measures were then averaged for each country, resulting in a ranking of 192 nations for which data were available (including industrialized countries). The results put Japan, France and Denmark at the top of the list, and Liberia, Haiti and Sierra Leone at the bottom.
The Rosenbloom et al. (2008) index has elements in common with the von Grebmer et al. (2013) Global Hunger Index (GHI). The latter, a long-standing index widely used for advocacy purposes by civil society organizations, is presented as a tool to “comprehensively measure and track hunger globally”. The original nomenclature of ‘nutrition index’ fell by the wayside in the early 2000s. The GHI also aggregates three separate indicators: i) the same FAO measure of chronic undernutrition, ii) child mortality and iii) the prevalence of underweight among under 5 s (the same metric as used for MDG1). The GHI is calculated by taking the percentage of the population in each country that is undernourished, the percentage of children younger than 5 years old who are underweight, and the percentage of children dying before the age of five. Each indicator is standardized to provide a single data point on a 100-point scale (where zero is the best score representing zero ‘hunger’). For 2013, the top (best) countries (of 120 for which data were available) were Albania, Mauritius and Uzbekistan; at the bottom were Comoros, Eritrea and Burundi. While the GHI has the advantage of being in relatively wide use for a decade or more, it suffers from the inclusion of both the FAO measure (of food availability) and child mortality as proxy ‘contributors’ to nutrition - neither is a proximate metric of any nutritional outcome or deficiency.Footnote 8
The most recent composite index is the Hidden Hunger Index (Muthayya et al. 2013). Also designed as an advocacy tool, the HHI focuses on preschool children, and also averages data for three equally-weighted indicators standardized on a scale of 0 to 100: namely, prevalence rates of child stunting, iron deficiency anaemia, and vitamin A deficiency (defined as low serum retinol levels). Using data from 149 countries with a low HDI (≤0.9), the HHI lists Hungary, Cuba and Croatia as the countries with the best hidden hunger status, while Benin, Kenya and Niger sit at the bottom of the rankings.
Each of the above indices offers various benefits and insights. They are simple to explain (transparent) and perform few transformations on what are publically-available data. As such, they are flexible enough to communicate with policymakers about issues that can be framed variously as hunger, food insecurity or malnutrition depending on the audience. What is more, as they are applied in a standardized way across countries they represent useful entry points for dialogue on nutrition priorities and possible actions.
Then why would another index offer value-added? Ravallion (2010) points out that “mashup indices exist because theory and rigorous empirics have not given enough attention to the full range of measurement problems faced in assessing development outcomes.” In other words, indices have traditionally been created with a view to bringing more attention to bear on the multifaceted nature of various development problems (be they ‘poverty’ or ‘hunger’ or ‘development’). For nutrition this is important given the WHA’s clear acknowledgement that “global nutrition challenges are multifaceted.” (WHO 2013). But Ravallion (2010) also rightly cautions against combining ‘apples and oranges’; that is, he criticizes approaches that mix an eclectic set of indicators that offer a semblance of inter-connectivity, but for which there is limited theoretical basis for aggregation. In this, he singles out the Alkire and Foster’s (2007) multi-dimentional index of poverty, which uses ten indicators to represent health, education and living standards.
The Net State of Nutrition Index proposed here is different. First, this index is the first to explicitly acknowledge that nutrition has ‘over and under’ dimensions to it that must be taken into account by policymakers; in other words, it represents an aggregate of ‘like’ metrics that all relate directly (empirically) to observable nutrition outcomes. Second, it is the first to construct a nutrition index tied to formal targets that governments have committed to. The index forces attention to the ‘net’ gains made at national levels and heads off potential cherry-picking of data among the six nutrition targets separately. None of the nutrition-specific indices reviewed above proposes a ‘net’ nutrition perspective that empirically accounts for lost ground in one area of nutrition as a consequence of making progress in another area; such as, for example, not acting to prevent an increase in obesity because of an overly narrow focus on treating wasting. The index proposed here addresses each of these problems.
Materials and methods
Like most other nutrition indices, the statistical approach adopted here to construct the Net State of Nutrition Index (NeSNI) rests on the United Nations Development Programme’s Human Development Index (UNDP 2013).Footnote 9 This choice is based on the fact that most governments already know of and understand the HDI, and because of its transparency (not relying on subjective or econometric weighing schemes). The HDI ranks countries based on three dimensions aimed at characterizing human development: a) life expectancy at birth; b) achievements in education; c) GDP per capita. A maximum and minimum value is assigned to each indicator, and the three are equally weighted, resulting in the following equation:
where i indicates an individual HDI dimension; x is the value of that dimension; and max and min are the assigned maximum and minimum values for each dimension. The HDI values range from 0 to 1, where one indicates the best case (a country with the highest levels of human development), while 0 indicates a country with the lowest human development.
The NeSNI follows the same structure, but combines the six WHA indicators. Minimum and maximum values are chosen based on the lowest and highest value of each indicator across all countries, and indicators are equally weighted (Table 1). Unlike the HDI, the NeSNI includes indicators which seek change in two directions, and ‘no change’ in a third; one indicator needs to rise to meet the defined target (exclusive breastfeeding), one should not increase (overweight), while the other four are expected to decline (stunting, anaemia, low birth weight, and wasting). Thus, the NeSNI is constructed using the following three steps:
- Step 1:
-
for indicators such as stunting, anaemia, low birth weight, overweight, wasting:
$$ A = {\displaystyle \sum_{i=1}^5}\left(ma{x}_i - {x}_i\right)/\left(ma{x}_i - mi{n}_i\right) $$As with the HDI, i is the pool of these 5 indicators; x is the value; max and min are the range of possible values for that indicator.
- Step 2:
-
for exclusive breastfeeding (EBF):
$$ B=\left({x}_{EBF} - mi{n}_{EBF}\right)/\left(ma{x}_{EBF} - mi{n}_{EBF}\right) $$x EBF is the actual value of the exclusive breastfeeding; max EBF and min EBF are the maximum and minimum values of breastfeeding.
- Step 3:
-
aggregates steps 1 and 2
$$ NeSNI=A+B $$
The data sources used are identified in Table 2. A sensitivity analysis was conducted to determine the degree to which co-linearity may be present, given that many nutrition problems co-exist within countries, within households and even by individuals. Table 3 shows that there are, as expected, statistically significant correlations among several of the indicators, most notably between anaemia and several physiological outcomes, because poor anthropometric status and micronutrient deficiencies are known to coexist in many instances, and undernourished mothers (including those suffering iron deficiency anaemia) often have undernourished babies. There is also a negative correlation between child overweight and manifestations of underweight, and between low birth weight and wasting in children under 5. While statistically significant in some instances, none of the correlations is so strong as to represent a like-for-like substitute. As such, all six variables are retained for the composite index. While the statistical correlation of other composite nutrition indices with the Human Development Index is high (R = 0.88 in the case of the Muthayya et al. (2013) Hidden Hunger Index), the NeSNI’s correlation is only R = 0.56. This suggests that the other nutrition indices rely more heavily on food supply, mortality and poverty measures as part of their scoring than elements more proximal to nutritional status.
Results
NeSNI scores were computed for 89 low and middle income countries for which data on all six variables could be collated (Table 4). At the top of the rankings are Uruguay, Colombia and Mongolia, while at the bottom are India, Niger and Yemen. Several countries widely considered to have made significant progress in tackling nutrition in recent years rank near the top, including Brazil, China and Costa Rica (UNICEF 2013; FAO/IFAD/WFP 2014). By contrast, none of these countries enter the top 10 of the rankings of the other index scoring approaches so far developed. Brazil, a poster-child for public sector-driven progress in reducing stunting (now only in single digits), does well to come in 5th in the NeSNI, but does not top the rankings in part due to suboptimal rates of exclusive breastfeeding (EBF) and continued problems with anaemia (almost one in four women are still affected by iron deficiency anaemia). Similarly, China has very low levels of EBF despite doing relatively well on the other indicators (except for child overweight which, while only 7 %, is climbing rapidly).
There is also a reality check in terms of the list of countries at the bottom of the NeSNI ranking. While it is often expected that countries facing crises (such as Niger, Yemen, and Sierra Leone) would rank lowest on a scale of progress on nutrition, the appearance in the bottom 10 of India, Nigeria and Pakistan (with Ethiopia, Indonesia and Bangladesh also in the bottom 20) underscores the reality that many nations with large populations have made little concrete progress on the broadly-framed dimensions of nutrition despite significant agricultural and macroeconomic growth over recent decades. Indeed, these large countries (in terms of population, size of economy and geography) are all among the 34 countries with the ‘highest burden of malnutrition’ according to the Lancet series on maternal and child nutrition (Black et al. 2013). As such, the NeSNI offers a credible ranking approach that closely mirrors the reality of existing multiple burdens of malnutrition.
Elsewhere in the rankings, many countries do well on one indicator but poorly on most others. For example, while there are some questions about the quality of data used, Nicaragua has one of the lowest rates of maternal anemia globally (around 9 %) due to a set of investments that, according to Mora (2007), included, “clear policies; updated technical guidelines; incorporation of iron and iron/folic acid supplements in the official list of essential medicines; addressing supply issues by establishing effective systems for procurement and logistical management of supply, as well as demand and compliance issues; and conducting operational research to address key constraints to implementation.” None of these interventions is particularly innovative, but together, along with significant improvements in food availability,Footnote 10 they appear to have made in-roads into a nutrition problem that continues to challenge most other countries around the world. That said, Nicaragua still has high levels of child stunting (22 %) and low exclusive breastfeeding (31 %), which highlights domains requiring prioritization going forward.
Many other countries can point to successes in one domain of nutrition but significant failure in at least one other. For example, Belarus has a low prevalence of child stunting (at 6 %), but reports extremely poor rates of exclusive breast feeding (15 %). Mongolia appears near the top of the rankings despite relatively high rates of stunting and overweight thanks to high rates of exclusive breastfeeding and low levels of anaemia. And Nepal records very low rates of child overweight, yet two-thirds of adult women are classified as anaemic (the highest rate among the 89 countries in this index), and stunting stands at around 40 %, although this has been falling in the past decade (FAO/IFAD/WFP 2014).
At the bottom end of the ranking, large economically strong countries, like India and Nigeria, in which agriculture contributes a large share of economic activity, demonstrate that gains in poverty reduction and agricultural productivity do not automatically translate into good nutrition. India still has a relatively low prevalence of child overweight, but it rates badly on all five other measures (including wasting, which still stands at roughly 20 % — one of the highest in the world). Nigeria also rates relatively well on one of the six indicators (LBW), but poorly on the other five (especially on anaemia and children overweight). The two countries at the very bottom of the rankings, Niger and Yemen, fare badly on all six variables. These are countries that have faced one crisis after another over several decades, but they even fare poorly on the metric of child overweight. In this case, huge efforts are needed not only to treat malnutrition that results from chronic emergency conditions but to resolve and prevent all other forms of poor nutrition from persisting into post-crisis years.
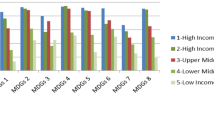
That several countries do well (or poorly) on one or more of the same indicators allows us to consider the clustering of nations into groups that share common characteristics. This is different from an application of arbitrary cut-offs in the ranking data to group countries as having mild, moderate, severe or alarming nutrition problems, as done by Muthayya et al. (2013). Instead, it is possible to use k-mean clustering to associate countries into four categories based on the commonality of their nutrition challenges. K-mean clustering groups observations based on the distance to the mean of each variable, in this case using their standardized Z-Score. Table 5 presents the results in terms of country aggregations, while the descriptives underpinning these four groupings are presented in supplementary material.
Table 5 indicates that countries having very different profiles in terms of size of population - both Bangladesh (population 155 million) and Nauru (population 10,000) are in group 1- size of economic activity (Nigeria and Haiti are together in group 2), or natural resource wealth (Botswana and its diamonds and Iraq with its oil are clustered in group 3 with Sao Tome which has limited natural resources) share common nutritional profiles. The first group is characterized by a high prevalence of stunting (average of 39 % across the 17 nations making up this group), despite high rates of exclusive breastfeeding (averaging more than 64 %) and low child overweight (less than 5 %). Group 2 has the highest average rate of anaemia (averaging 51 % across 30 countries), the highest rates of LBW (more than 16 % average), and the highest wasting (averaging over 9 %). The third group has the highest average prevalence of overweight (17 % across 13 states), while the fourth grouping has the lowest rates of exclusive breastfeeding (averaging 27 % across 29 countries), but also the lowest prevalence of LBW.
Such clustering underscores the fact that nutrition policy and investment priorities cannot all be the same for every country, but learning across nations with similar problems is possible. It is of course important for all governments to focus on the first 1,000 days and to promote best practices supportive of population-wide gains in nutrition (including high quality service delivery, institutions capable of implementing evidence-based interventions, and individuals appropriately trained for their responsibilities). Yet, nutrition problems tend to manifest as a mosaic of processes and symptoms that differ in ways that are not entirely predicted by national wealth, size or form of government.
This suggests that the NeSNI can be useful to donors and policymakers as they seek to define priority needs, and track progress in addressing those needs. The index alone does not tell the whole story – it is change over time in each of the component parts that matters. But combining these six features of nutrition that are tied to measurable time-bound goals can allow governments to have a more nuanced understanding of potential trade-offs among various nutrition-specific and nutrition-sensitive actions depending on net outcomes (that is, progress on one indicator of nutrition does not guarantee progress on all others, and can in fact co-exist with regression in the others). Countries will only climb in the rankings and meet the goals set if they consciously address nutrition across the lifecycle, invest in prevention but also treatment of existing problems, and think through potential negative side-effects of any policy or programme intervention that could improve one indicator while unintentionally worsening another (Webb and Block 2012).
Conclusions
The World Health Assembly targets set for improving nutrition by 2025 represent a major but tangible challenge to policymakers worldwide. They require governments and their development partners to pay much more attention to the multiple manifestations and underlying causes of poor nutrition, and to invest in interventions that promote gains while doing no unintended harm. It will take a concerted and coordinated effort by governments if they are to make the required net gains across all inter-related domains of nutrition. That is, unlike with the MDGs, where victory on MDG1 was proclaimed when just one of its component targets was reached, no country can record success on the NeSNI scale if they focus on just one or other of the individual targets. The complex causes of the world’s nutrition challenges calls for a comprehensive response. The 21st century’s food-related nutrition problems include obesity and diet-related non-communicable diseases, in addition to various forms of undernutrition, including widespread vitamin and mineral deficiencies. Access to high quality diverse diets is an essential basis for tackling all forms of malnutrition, thus attention to the quality and sustainability of agricultural systems is key to supporting multiple nutrition goals (Global Panel 2014). Food and agriculture policy makers should at the very least consider how their activities can support the WHA nutrition outcomes through impacts on diets, food prices, gendered resource control, women’s energy and time demands and farm-based income use. As noted above, while nutrition-sensitive interventions are distal to the nutrition outcomes of immediate concern, their contribution to improving such outcomes can be significant (Bhutta et al. 2013).
Documenting national progress in tackling nutrition has risen high on the list of policy makers’ demands. As every country’s situation is different, the precise approach to integrating nutrition-specific and nutrition-sensitive interventions must be country driven, and these have to pay attention to potential unintended effects. A nuanced understanding of this complex problem can be supported by an index that assesses net nutrition outcomes. In future, additional measures of nutrition could be added to the NeSNI (such as iodine deficiency or adolescent girl BMI). Similarly, improved and validated metrics of dietary quality and diversity would enhance the existing set of physiological indicators of nutrition and could also be included in future index formulations.
However, the coverage and quality of such data would have to be significantly improved. Problems of poor data quality and inadequate periodicity of data collected bedevil all attempts to track progress towards global targets. That only 89 countries currently have comparable data on all six WHA indicators means that investments in data collection and database construction remain a priority if global tracking of the effectiveness of investments made is to be taken seriously. In the post-2015 era, governments must pay much more attention not only to the evidence-base for making appropriate policies, but to the evidence base generated that documents subsequent outcomes.
The number of indicators aggregated matters less than the understanding gained that all manifestations of poor nutrition require equal attention. The NeSNI tool is unique in aggregating so many facets of malnutrition and in linking these to a target-setting agenda. Use of NeSNI may allow governments and their partners to monitor progress against WHA and other global commitments (such as the nutrition targets within the Sustainable Development Goals), while also helping policy makers better under understand that their own nutrition problems are multidimensional, often co-existing, and worthy of equal, urgent attention.
Notes
According to WHO (2013), stunting is defined as height-for-age < −2 standard deviations below the WHO child growth standard median for children aged under 5 years. Stunting becomes a public health problem when ≥ 20 % of the population is affected. Wasting is classified as weight-for-height < −2 standard deviations below the WHO child growth standard median for children aged under 5 years. Wasting becomes a public health problem when ≥ 5 % of the population is affected.
Empirical data on micronutrient deficiencies are very difficult to come by as few governments conduct nationally representative surveys of micronutrient deficiencies, and even if they do, they usually only include one or two nutrients.
According to Ruel et al. (2013), nutrition-specific interventions are individually targeted to resolve immediate determinants of nutrition problems, while nutrition-sensitive interventions address underlying causes of poor nutrition more broadly.
It is not suggested that there is a direct or linear relationship between policy support for agriculture and rising obesity, but that greater attention should be paid to which kinds of agricultural support are more or less supportive of both stunting reduction and improving access to higher quality diets that could contribute to obesity prevention.
It should be noted that child underweight (low weight-for-age), which served as the single nutrition target in MDG1, was not included as part of the WHA set of indicators. This is largely because underweight represents a composite measure reflecting elements of both stunting and wasting, and hence poses problems in defining causes and appropriate solutions.
The authors refer to WHO death and DALY estimates for 2002 (available online at the WHO website) without further detail.
The age range 15 to 100 years is no typo – that is the range in WHO’s database: https://apps.who.int/infobase/report.aspx
Of course, child undernutrition and child mortality are correlated through the morbidity and mortality effects of nutritional deficiencies interacting with diseases, but they are not proximate indicators of nutrition.
Nicaragua’s rate of chronic undernourishment (the FAO metric of energy available at national level) declined from 54 % in 1990–92 to 17 % in 2012–14 (FAO/IFAD/WFP 2014).
References
Alkire, S., & Foster, J. (2007). Counting and multidimensional poverty measurement (Oxford poverty and human development initiative, working paper 7). Oxford: University of Oxford.
Alkire, S., & Santos, M. (2013). A multidimensional approach: poverty measurement & beyond. Social Indicators Research. doi:10.1007/s11205-013-0257-3.
Bhutta, Z. A., Das, J. K., Rizvi, A., Gaffey, M. F., Walker, N., Horton, S., et al. (2013). Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? The Lancet, 382(9890), 452–477. doi:10.1016/S0140-6736(13)60996-4.
Black, R. E., Victora, C. G., Walker, S. P., Bhutta, Z. A., Christian, P., de Onis, M., et al. (2013). Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet, 382(9890), 427–451. doi:10.1016/S0140-6736(13)60937-X.
De Onis, M., Dewey, K. G., Borghi, E., Onyango, A. W., Blössner, M., Daelmans, B., et al. (2013). The World Health Organization’s global target for reducing childhood stunting by 2025: rationale and proposed actions. Maternal & Child Nutrition, 9(S2), 6–26. doi:10.1111/mcn.12075.
Fanzo, J. C., & Pronyk, P. M. (2011). A review of global progress toward the millennium development goal 1 hunger target. Food and Nutrition Bulletin, 32(2), 144–158.
FAO (Food and Agriculture Organization of the United Nations). (2011). Women in agriculture: closing the gender gap for development. Rome: The State of Food and Agriculture.
FAO/WHO (Food and Agriculture Organization of the United Nations/World Health Organization) (2014). Conference outcome document: rome declaration on nutrition. Second International Conference on Nutrition, Document ICN2 2014/2. Rome. Italy.
FAO/IFAD/WFP (Food and Agriculture Organization of the United Nations/International Fund for Agriculture Development/World Food Programme). (2014). The state of food insecurity 2014: strengthening the enabling environment for food security and nutrition. Rome: FAO.
Global Panel (on Agriculture and Food Systems for Nutrition). (2014). How can agriculture and food system policies improve nutrition? Technical Brief. London: Global Panel on Agriculture and Food Systems for Nutrition.
Habicht, J.-P., & Pelto, G. H. (2014). From biological to program efficacy: promoting dialogue among the research, policy, and program communities. Advances in Nutrition: an International Review Journal, 5(1), 27–34. doi:10.3945/an.113.004689.
Hoddinott, J., Alderman, H., Behrman, J. R., Haddad, L., & Horton, S. (2013). The economic rationale for investing in stunting reduction. Maternal & Child Nutrition, 9(S2), 69–82. doi:10.1111/mcn.12080.
IFPRI (International Food Policy Research Institute) (2014). Global nutrition report 2014: actions and accountability to accelerate world's progress on nutrition. Washington, D.C.
Lim, S. S., Vos, T., Flaxman, A. D., Danaei, G., Shibuya, K., Adair-Rohani, H., et al. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380(9859), 2224–2260. doi:10.1016/S0140-6736(12)61766-8.
Mora, J. (2007). Integrated anemia control strategy has significantly reduced anemia in women and children in Nicaragua. Micronutrient initiative. http://www.micronutrient.org/CMFiles/PubLib/Nicaragua_Anemiacontrolprog_finalrpt1RXF-11272008-7660.pdf. Accessed 15 Dec 2014.
Murray, C. J. L., Vos, T., Lozano, R., Naghavi, M., Flaxman, A. D., Michaud, C., et al. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380(9859), 2197–2223. doi:10.1016/S0140-6736(12)61689-4.
Muthayya, S., Rah, J. H., Sugimoto, J. D., Roos, F. F., Kraemer, K., & Black, R. E. (2013). The global hidden hunger indices and maps: an advocacy tool for action. PLoS ONE, 8(6), e67860. doi:10.1371/journal.pone.0067860.
Ng, M., Fleming, T., Robinson, M., Thomson, B., Graetz, N., Margono, C., et al. (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 384(9945), 766–781. doi:10.1016/S0140-6736(14)60460-8.
Norris, S. A., Osmond, C., Gigante, D., Kuzawa, C. W., Ramakrishnan, L., Lee, N. R., et al. (2012). Size at birth, weight gain in infancy and childhood, and adult diabetes risk in five low- or middle-income country birth cohorts. Diabetes Care, 35(1), 72–79. doi:10.2337/dc11-0456.
Petry, N., Egli, I., Gahutu, J. B., Tugirimana, P. L., Boy, E., & Hurrell, R. (2014). Phytic acid concentration influences iron bioavailability from biofortified beans in Rwandese women with low iron status. Journal of Nutrition, 144(11), 1681–1687. doi:10.3945/jn.114.192989.
Ravallion, M. (2010). On multidimensional indices of poverty. Working paper. Washington: World Bank. http://www.cgdev.org/doc/event%20docs/Multidimensional-Indices-of-Poverty.pdf. Accessed 15 Dec 2014.
Rosenbloom, J. I., Kaluski, D. N., & Berry, E. M. (2008). A global nutritional index. Food and Nutrition Bulletin, 29(4), 266–277.
Ruel, M. T., Alderman, H., & Maternal and Child Nutrition Study Group. (2013). Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? Lancet, 382(9891), 536–551. doi:10.1016/S0140-6736(13)60843-0.
Smith, L., & Haddad, L. (2014). Reducing child undernutrition: past drivers and priorities for the post-MDG Era (IDS working paper 441). Brighton: Institute of Development Studies.
Sunguya, B. F., Ong, K. I. C., Dhakal, S., Mlunde, L. B., Shibanuma, A., Yasuoka, J., et al. (2014). Strong nutrition governance is a key to addressing nutrition transition in low and middle-income countries: review of countries’ nutrition policies. Nutrition Journal, 13(1), 65. doi:10.1186/1475-2891-13-65.
SUN (Scaling Up Nutrition) (2010). Scaling up nutrition. A framework for action. http://siteresources.worldbank.org/NUTRITION/Resources/281846-1131636806329/PolicyBriefNutrition.pdf. Accessed 15 Dec 2014.
UN (United Nations) (2014). The millennium development goals report 2014. New York, NY.
UN (United Nations). (2005). Investing in development (pp. 1–353). New York: UN Millennium Project.
United Nations Development Programme. (2013). Human development report 2013 (pp. 1–216). New York: United Nations Development Programme.
UNHLP (United Nations High Level Panel of Eminent Persons) (2013). A New global partnership: eradicate poverty and transform economies through sustainable development. Report of the high- level panel of eminent persons on the post-2015 Development Agenda. New York, NY.
UNICEF. (2013). Improving child nutrition: The achievable imperative for global progress. New York, NY. http://www.unicef.org/gambia/Improving_Child_Nutrition_-_the_achievable_imperative_for_global_progress.pdf. Accessed 15 Dec 2014.
UNICEF. (2006). Vitamin and mineral deficiency: a global progress report. New York, NY.
UNSCN (United Nations’ Standing Committee on Nutrition). (2014). Nutrition and the post-2015 sustainable development goals. Geneva: Switzerland.
Uauy, R., Kain, J., & Corvalan, C. (2011). How can the developmental origins of health and disease (DOHaD) hypothesis contribute to improving health in developing countries? The American Journal of Clinical Nutrition, 94(6), 1759S–1764S. doi:10.3945/ajcn.110.000562.
von Grebmer K., Headey D., Olofinbiyi T., Wiesmann D., Fritschel H., Yin S., Yohannes Y., Foley C., von Oppeln C., Iseli B., Béné C. & Haddad L. (2013). Global Hunger Index 2013: The challenge of hunger: Building resilience to achieve food and nutrition security. IFPRI/Welthungerhilfe/Concern Worldwide/IDS: Bonn/Washington, DC/Dublin.
Webb, P., Boyd, E., de Pee, S., Lenters, L., Bloem, M., & Schultink, W. (2014). Nutrition in emergencies: Do we know what works? Food Policy, 49, 33–40. doi:10.1016/j.foodpol.2014.03.016.
Webb, P., & Block, S. (2012). Support for agriculture during economic transformation: impacts on poverty and undernutrition. Proceedings of the National Academy of Sciences of the United States of America, 109(31), 12309–12314. doi:10.1073/pnas.0913334108.
Wiesmann, D., von Braun J., & Feldbrugge T. (2000). An International Nutrition Index. Center for International Research. Discussion Papers on Development Policy No.26. Bonn, Germany.
World Bank (2014). Millennium development goals: eradicate extreme poverty and hunger by 2015. http://www.worldbank.org/mdgs/poverty_hunger.html. Accessed 15 Dec 2014.
WHO (World Health Organization). (2013). Global nutrition policy review: what does it take to scale up nutrition action? Geneva: WHO Document Production Services.
WHO (World Health Organization) (2012). Resolution WHA 65.6 maternal, infant and young child nutrition. In: Sixty-Fifth World Health Assembly, Geneva, 21–26 May. Resolutions and Decisions, Annexes. http://apps.who.int/gb/ebwha/pdf_files/WHA65-REC1/A65_REC1-en.pdf. Accessed December 4, 2014.
WHO (World Health Organization). (2008a). Indicators for assessing infant and young child feeding practices (pp. 1–26). Geneva: World Health Organization.
WHO (World Health Organization). (2008b). World prevalence of anaemia 1993–2005 (pp. 1–51). Geneva: World Health Organization.
WHO (World Health Organization) (2006). WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development.
World Health Organization/UNICEF. (2005). Low birthweight (pp. 1–31). Geneva: World Health Organization.
Acknowledgments
The authors would like to acknowledge the valuable comments made by two anonymous reviewers and by the editorial team on an earlier draft. Patrick Webb acknowledges support given for this work by USAID’s Feed the Future Innovation Laboratory for Nutrition. The paper was prepared in part as a contribution to the evidence-building mandate of the Global Panel on Agriculture and Food Systems for Nutrition.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Special section series
Strengthening the links between nutrition and health outcomes and agricultural research
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Webb, P., Luo, H. & Gentilini, U. Measuring multiple facets of malnutrition simultaneously: the missing link in setting nutrition targets and policymaking. Food Sec. 7, 479–492 (2015). https://doi.org/10.1007/s12571-015-0450-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12571-015-0450-0