Abstract
Introduction
Medications for preventive treatment of migraine reduce migraine frequency, usually measured by a reduction in monthly migraine days (MMD), but generally do not eliminate the need for acute treatment. To assess the economic impact of treatment-related reductions in frequency, methodological guidance recommends capturing cost differences along the spectrum of MMD.
Objective
Characterize monthly migraine medication costs along the spectrum of MMD for patients using calcitonin gene-related peptide (CGRP) monoclonal antibodies (mAbs) for prevention.
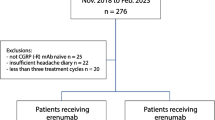
Methods
Medicaid State Drug Utilization Data (SDUD) were used to identify formulations and per-unit costs for oral, intranasal, and parenteral migraine-specific medications for acute and preventive treatment used by fee-for-service (FFS) Medicaid enrollees in 2020. National drug codes of relevant therapies were used to match SDUD to formulation characteristics including substance, route of administration, and branded/generic marketing status. Mean per-unit cost and the formulation’s share of total prescriptions were estimated. Monthly medication costs were modeled based on formulations’ per-unit costs and frequency of acute medication use during clinical trials of CGRP mAbs.
Results
In the SDUD, there were 563,338 prescriptions for migraine-specific acute medications; triptans accounted for 97.37%. Triptan formulations prescribed were 83.78% oral tablet, 10.89% orally disintegrating tablet, 2.60% intranasal, and 2.73% parenteral. Dihydroergotamine accounted for < 1% of total prescriptions and had the highest per-unit cost ($443.50, branded intranasal). There were 97,119 prescriptions for CGRP mAbs, the majority for erenumab (45.73%) or galcanezumab (45.24%). Modeled monthly acute and preventive medication costs ranged from approximately $550 in patients with the fewest MMD treated with oral triptans to > $1500 in patients with the most MMD treated with dihydroergotamine.
Conclusion
In consideration of the migraine-specific acute medications used in FFS Medicaid 2020, for patients using CGRP mAbs for prevention, medication costs may vary significantly with the number of breakthrough attacks treated per month and the type of migraine-specific acute therapy used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Preventive treatment of migraine aims to reduce the number of days per month with migraine (monthly migraine days [MMD]), but it rarely eliminates the need for acute treatment of occasional “breakthrough” attacks. |
Recent methodological guidance on economic evaluation of preventive treatments for migraine recommends modeling costs varying across the full spectrum of migraine frequency; however, existing evaluations of calcitonin gene-related peptide (CGRP) monoclonal antibodies (mAbs) generally model only mean costs by ranges of MMD. |
We analyzed medication costs across the spectrum of MMD, for Medicaid patients on preventive treatment with a CGRP mAb and acute treatment of breakthrough attacks with a migraine-specific acute medication, to provide cost estimates to inform future economic evaluations. |
What was learned from the study? |
Based on the types of acute treatments used in fee-for-service (FFS) Medicaid in 2020, modeled monthly medication costs ranged from approximately $550 in patients with the fewest MMD treated with orally administered triptans to > $1500 in those with the most MMD treated with dihydroergotamine. |
For patients with migraine taking CGRP mAb preventive treatment, the cost of acute treatment may vary significantly with the frequency of breakthrough attacks and the type of migraine-specific acute medication used. |
Introduction
Migraine is a chronic neurologic condition characterized by recurrent attacks of headache featuring unilateral, pulsating or throbbing pain generally exacerbated by physical activity and accompanied by nausea and/or vomiting and sensitivity to light or sound [1]. In the USA, an estimated 47 million people have migraine [2]. Migraine-related disability has negative effects on performance at work and in school and on participation in and enjoyment of social life; it is the most common cause of years lived with disability in people younger than 50 [3]. The burden of migraine falls most heavily on young-adult and middle-aged women (aged 18–44), and people who are unemployed, elderly, or disabled; those with family income less than $35,000 per year have also been observed to be disproportionately affected [4].
Medications for migraine are typically distinguished as acute or preventive. Those used for acute treatment, which are taken to alleviate migraine pain and associated symptoms and to restore ability to function during a migraine attack [5], can be non-specific or migraine-specific. Non-specific agents include simple analgesics (e.g., aspirin, acetaminophen), nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen, naproxen), opioid analgesics, butalbital-containing analgesic products, and over-the-counter combinations of analgesics including caffeine (e.g., aspirin + acetaminophen + caffeine) [5]. Migraine-specific medications include drugs developed and approved for the treatment of migraine: serotonin agonists (triptans, lasmiditan); dihydroergotamine (DHE); and calcitonin gene-related peptide (CGRP) receptor antagonists (rimegepant and ubrogepant) [5, 6]. Clinical guidance recommends that acute treatments be offered to all patients with migraine [7], and they remain recommended for treating attacks (as necessary) with use of a preventive therapy [5].
Medications for the preventive treatment of migraine, which are intended to reduce attack frequency, severity, duration, and associated disability, as well as to improve response to acute treatment [5], are typically recommended when patients experience frequent or severely disabling attacks [5]. Estimates suggest that nearly 40% of patients with migraine, including almost all of those with chronic migraine, may benefit from preventive treatment [8]. Historically, however, few patients with migraine (3–13%) used preventive treatment, mainly due to inadequate efficacy and poor tolerability [9]. A newer class of preventive treatments, CGRP monoclonal antibodies (mAbs), includes four agents: erenumab, fremanezumab, and galcanezumab given as a subcutaneous injection, and eptinezumab given as an intravenous infusion [10]. Efficacy of preventive treatment is commonly assessed on the basis of reduction in migraine frequency, expressed in days per month with headache (monthly headache days, MHD) and/or days per month with migraine (monthly migraine days, MMD). Response to treatment may be considered on the basis of a threshold percentage reduction in MMD (e.g., by 30% or 50% [11,12,13,14]). As a result, the CGRP mAbs, like traditional preventive medications, may not eliminate the need for acute treatment of occasional breakthrough attacks [9, 14,15,16].
Medicaid is a joint federal and state program that provides free or low-cost health coverage to approximately 80 million people in the USA [17]; eligibility criteria vary by state, but the program generally covers low-income individuals [18]. As the prevalence and burden of migraine are higher in Medicaid-insured individuals than in the general migraine population [19], effective treatment of people with migraine has the potential to produce substantial improvements in overall health, productivity, and quality of life. Medicaid policies for use of a CGRP mAb for migraine prevention commonly require previous trial of and insufficient response to multiple oral preventive therapies [20, 21]. Patients who receive them may therefore have also had suboptimal experiences with one or more first-line acute therapies, as clinical guidelines recommend initiation of preventive therapy for patients with frequent attacks and contraindication to, failure of, or overuse of acute treatments [9]. Contraindication to triptans may be especially common in Medicaid populations as a result of the high prevalence of CV risk factors, including hypertension, hyperlipidemia, and diabetes [5, 22,23,24]. Thus, Medicaid patients progressing to use of a CGRP mAb for preventive treatment may also be eligible for second- or third-line medications for acute treatment (i.e., non-oral triptan and DHE formulations, gepants, and ditans), the combination of which could be associated with considerable costs [6].
Recent research of temporal trends from 2017 to 2020 in utilization and costs of migraine therapies indicates that while CGRP mAb use and contribution to overall costs of therapy have increased over time, triptans remain the most commonly used migraine-specific medications [25]. Accurate economic evaluation of CGRP mAbs for prevention should therefore account for the costs of triptans and other acute therapies used for management of breakthrough attacks. Methodological guidance on economic evaluation of preventive treatments for migraine [13] recommends modeling treatment costs varying across the full spectrum of migraine frequency, rather than only varying by particular ranges of frequency (e.g., chronic migraine as ≥ 8 MMD) [13]. However, existing economic evaluations of CGRP mAbs generally model mean costs and effects by ranges of MMD, potentially omitting important variation along the spectrum of migraine frequency [26]. We therefore sought to characterize the costs of acute treatment in patients receiving CGRP mAbs for the preventive treatment of migraine across the spectrum of MMD in a Medicaid population.
Methods
To identify migraine-specific therapies used and their respective costs per unit (i.e., one oral, intranasal, or parenteral dose), we used Medicaid State Drug Utilization Data (SDUD). The SDUD are reported on a quarterly basis by the US Centers for Medicare & Medicaid Services (CMS), reflecting prescription drug use in states participating in the Medicaid Drug Rebate Program, which specifies the prices Medicaid pays for drugs [27, 28]. For branded products, Medicaid pays either the manufacturer’s best price to any wholesaler, retailer, or provider or the average manufacturer price (AMP) minus 23.1%, whichever is lower. For generic products, Medicaid receives a rebate of 13% of AMP; there is no best-price option [27]. The rebate also includes a penalty for price increases exceeding inflation [27].
This analysis used fee-for-service (FFS) utilization records for 2020. Managed care organization (MCO) utilization records were excluded to focus the analysis on pharmacy costs, independent of the impact of capitated payments for medical and pharmacy benefits potentially paid to MCOs [29]. Key variables in the SDUD used in the analysis were the Medicaid amount reimbursed (excluding best-price rebates), the number of prescriptions, and the units reimbursed [30].
To identify prescriptions of migraine-specific acute and preventive therapies in the SDUD, we searched the US Food and Drug Administration (FDA)’s National Drug Code (NDC) directory [31] for the following terms: eptinezumab, erenumab, ergotamine, fremanezumab, galcanezumab, lasmiditan, rimegepant, triptan, or ubrogepant. Results of the search were reviewed to exclude substances without FDA indication for treatment of migraine (i.e., oxitriptan therapies), then NDCs associated with the remaining substances were compiled into a list of relevant formulations, and merged onto the SDUD, yielding a data set containing number of prescriptions, number of units prescribed, and Medicaid reimbursed amounts.
The data set was organized by substance (e.g., eletriptan vs. sumatriptan) and route of administration (i.e., oral, orally disintegrating tablet (ODT), intranasal, injection, infusion). Branded and generic formulations were distinguished on the basis of their marketing category designation in the NDC directory; records designated as “NDA” (New Drug Application) were considered branded, and those designated as “ANDA” (abbreviated NDA) or “NDA authorized generic” were considered generic.
For the analysis, total Medicaid amount reimbursed, number of prescriptions, and units reimbursed were calculated for each combination of substance, route of administration, and marketing category. Share of migraine-specific acute prescriptions was calculated as the formulation’s total prescriptions divided by total prescriptions of acute therapies identified. Share of migraine-specific preventive prescriptions was calculated as the formulation’s total prescriptions divided by total prescriptions of preventive therapies identified. Mean cost per unit was calculated as the formulation’s total Medicaid reimbursed amount divided by the formulation’s total units reimbursed.
Mean cost per unit estimates from the SDUD were used to determine total cost of preventive therapy with mAbs, including the cost of acute therapies used to treat breakthrough migraine attacks. Monthly use of migraine-specific medication for acute treatment of breakthrough attacks was estimated on the basis of the results of post hoc analyses [14] of acute medication use during three clinical studies of erenumab, a CGRP mAb, for the preventive treatment of migraine [32,33,34]. In these studies, investigators recorded days on which participants used migraine-specific acute therapy (triptans or ergotamine derivatives) and days on which migraine attacks occurred. The post hoc analysis of these data modeled days per month on which participants used medication for acute treatment as a function of MMD and other covariates, including age, sex, race, treatment group, prior failed preventive migraine medication status, and baseline MMD [14]. Since a meaningful percentage of erenumab-treated participants reported no use of acute medication, zero-inflated Poisson regression models were used to predict usage; robust standard errors clustered at the patient level were used to account for repeated measurements per patient [14]. In the present analysis, because clinical guidelines recommend against use of migraine-specific acute medications on 10 or more days per month because of the risk of medication overuse [5], but participants in the erenumab trials were predicted to exceed that threshold when they experienced more than 22 MMD [14], the highest number of MMD modeled was 22.
The analysis reported is based on previously conducted studies and public-use data and does not contain any new studies with human participants or animals performed by any of the authors.
Results
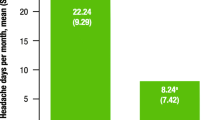
Approximately 12 million (17%) of 71 million Medicaid enrollees had FFS coverage in 2020 [35, 36]. Overall, they received 563,338 prescriptions (5.63 million units) for acute treatment with migraine-specific medications and 97,119 prescriptions (0.11 million units) for preventive treatment with CGRP mAbs. Generic triptan oral tablets accounted for 80.36% of the total prescriptions for migraine-specific acute therapies; the remainder were for non-oral and/or branded triptans (17.01%), ergotamine-based therapies (0.88%), and novel acute therapies (rimegepant, ubrogepant, and lasmiditan) (1.75%). Note that while rimegepant has been approved by the FDA for preventive treatment of episodic migraine since May 27, 2021, its use was considered as an acute therapy in the analysis, as the Medicaid SDUD from 2020 precede rimegepant’s indication for prevention. Triptan formulations prescribed were 83.78% oral tablet, 10.89% orally disintegrating tablet, 2.60% nasal spray, and 2.73% injectable. DHE formulations accounted for 0.87% of all migraine-specific acute therapy prescriptions, the majority of which (approximately 80%) were intranasal versus injected. Migraine-specific acute and preventive prescription shares and mean (SD) cost-per-unit estimates are presented in Table 1.
To model the monthly drug costs along the spectrum of MMD, the cost-per-unit estimates presented in Table 1 were grouped into several classes for ease of interpretation. These include oral and ODT triptans, intranasal triptans, injected (SC) triptans, intranasal DHE, injected DHE, oral ergotamine-based therapies (i.e., generic oral ergotamine and ergotamine + caffeine), and novel acute therapies (i.e., rimegepant, ubrogepant, and lasmiditan). Of note, monthly costs of treating breakthrough attacks with any of the therapeutic categories/formulations in Table 1 may be calculated using the notes to Table S1 in the Supplementary Material. Within each class, the cost per unit estimates of different formulations were weighted proportionally to their prescription share in Table 1. For example, the estimated mean cost per unit for intranasal triptans reflects generic intranasal triptans with weight of 67.19% (i.e., 1.70%/[1.70% + 0.83%]) and branded intranasal triptans with weight of 32.81% (i.e., 0.83%/[1.70%+ 0.83%]).
Figure 1 presents estimates of the monthly drug costs of preventive therapy with a CGRP mAb and migraine-specific medication for acute treatment of breakthrough attacks along the spectrum of MMD. Monthly days of migraine-specific acute therapy use by frequency of MMD, as reported in the erenumab clinical studies previously referenced [14], are labeled along the horizontal axis (e.g., a patient with 8 MMD uses migraine-specific acute therapies on 2.82 days per month). Costs varied considerably with the type of acute treatment used for breakthrough attacks, as well as with the frequency of breakthrough for all acute treatments except oral triptans. Monthly costs of a CGRP mAb and oral triptans ranged from $552 to $576 across the spectrum of MMD. Costs were similar for treatment of breakthrough with nasal triptans and oral ergotamine-based treatments (ranging from $625 to $1160 across the spectrum of MMD), and with injected triptans and novel acute therapies (ranging from $663 to $1439 across the spectrum of MMD). Costs were highest with DHE treatments used for breakthrough, ranging from $689 to $1606 for injected DHE formulations and from $958 to $3628 for nasal DHE formulations across the spectrum of MMD. See the Supplementary Material for series of estimated monthly costs across the spectrum of MMD.
Discussion
This analysis of prescription data for Medicaid enrollees with FFS coverage in 2020 showed that approximately 20% of migraine-specific acute therapy prescriptions were for formulations other than generic triptan tablets. This estimate is consistent with previous research in the USA [37] and England [38] as well as with a US budget impact analysis of new acute therapies [39] conducted in 2019 by the Institute for Clinical and Economic Review, suggesting that 15–25% of patients with migraine may progress beyond first-line migraine-specific acute treatments. Per-unit cost estimates based on Medicaid amounts reimbursed indicated that, among migraine-specific acute therapies, intranasal DHE is the most expensive followed by injectable DHE, injectable triptans, gepants (rimegepant, ubrogepant) and lasmiditan, intranasal triptans, other oral ergotamine-based therapies, and oral triptans. The estimated monthly costs by MMD presented in this study (see Table S1 in the Supplementary Material, listing values presented in Fig. 1) may be of use for future pharmacoeconomic evaluation of use of migraine-specific therapies.
Medicaid coverage policies for use of an oral preventive therapy commonly align with those for trial of a migraine-specific acute therapy beyond first-line triptans. It is therefore anticipated that Medicaid patients using CGRP mAbs for prevention may also use migraine-specific acute therapies beyond first-line oral triptans. In this study, the type of acute medication used for treatment of breakthrough attacks while using a CGRP mAb was found to be an important driver of total monthly medication costs. While restricting use of migraine-specific medications to at most 10 days of acute treatment per month (in accordance with clinical guidance against medication overuse), at higher levels of MMD, we found that the cost of medication for acute treatment exceeded the cost of the CGRP mAb used for prevention; this was true for DHE at lower levels of MMD. We also found that treatment costs were significantly influenced by baseline MMD. These findings support recent methodological guidance on pharmacoeconomic evaluation of migraine therapies [13], recognizing the importance of distinguishing outcomes and costs associated with interventions across the spectrum of migraine frequency.
Results of this study have practical relevance to healthcare decision-making around the affordable and cost-effective use of migraine therapies. Previous analyses of clinical studies of CGRP mAbs for prevention indicate that use of migraine-specific acute treatments for management of breakthrough MMD rises exponentially with the number of breakthrough MMD [14]. Consequently, as reflected in this study, patients who do not achieve a desired response (e.g., 30% or 50% reduction from baseline MMD) may continue to require frequent use of migraine-specific acute treatments for management of breakthrough attacks, which is associated with high costs particularly for those with high baseline MMD and/or use of acute treatment beyond first-line triptans. Despite acute management of breakthrough attacks, such patients are likely to continue to experience significant burden of migraine, as similar impact on a patient’s ability to function on the job, at school, at home, and in social situations has been observed for moderate vs. high levels of attack frequency (e.g., 10–14 vs. ≥ 15 MHDs) as measured by the Migraine Disability Assessment Test (MIDAS) and Headache Impact Test (HIT-6) [40]. Accordingly, clinical guidelines recommend that to determine treatment continuation, the clinical benefit of a CGRP mAb should be assessed after at least 3/6 months of treatment for those administered monthly/quarterly, to ensure benefits have been achieved [5]. Results of this study may help inform decision-making relating to the optimal duration and criteria for continuation of preventive therapy, by providing estimates of the costs of acute treatment conditional on the number of breakthrough MMD a patient continues to experience. Similar research of the variation by MMD of other important costs and effects, such as costs of non-pharmacologic healthcare resource use (in particular, emergency room visits and hospitalizations) and effects on patient productivity (i.e., presenteeism and absenteeism) [41], would help further improve the accuracy of future economic evaluations of novel preventive therapies.
This study has certain strengths and limitations. Strengths include the size and the quality of the SDUD prescriptions data set. Cost-per-unit results estimated in the analysis were validated by comparison to wholesale acquisition costs (WAC) data [42] and annual medication costs modeled in an economic evaluation of CGRP mAbs in the USA [43]. Because the analysis was restricted to individuals covered by FFS Medicaid, however, generalizations to other populations should be made with caution. Estimates may also overstate the net cost of branded relative to generic drugs because Medicaid reimbursements reflect costs before best-price rebates, which are higher for branded than generic drugs (because of both statutory requirements and likely competitive pressures). At the same time, the cost of acute treatment may have been underestimated because the analysis does not account for the use of multiple units per treatment day. A further limitation may be that migraine-specific acute medication use was costed by unit, rather than prescription, while units are bundled by pack size in real-world utilization. Finally, the SDUD do not provide insight into which drugs are most commonly used for acute treatment by patients using CGRP mAbs for preventive treatment. Future research characterizing the types of migraine-specific acute therapies most commonly used by patients on mAbs for prevention would assist in the interpretation of this study’s results.
Conclusion
Among Medicaid enrollees with FFS coverage in 2020, approximately 20% of prescriptions for migraine-specific acute treatments were for medications other than generic oral triptan tablets, with intranasal DHE and injected DHE the most costly. For patients with high MMD prior to initiating a CGRP mAb for preventive treatment, and using migraine-specific medication other than a generic oral triptan for acute treatment of breakthrough attacks, the costs of acute treatment exceeded those of the CGRP mAb. Key factors in the economic impact of a reduction in MMD were MMD prior to use of the mAb, and the type of migraine-specific medication for acute treatment used for breakthrough attacks.
References
Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954–76.
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59.
Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: figures and trends from government health studies. Headache. 2018;58(4):496–505.
Ailani J, Burch RC, Robbins MS. The American Headache Society consensus statement: update on integrating new migraine treatments into clinical practice. Headache. 2021;61(7):1021–39.
Mayans L, Walling A. Acute migraine headache: treatment strategies. Am Fam Physician. 2018;97(4):243–51.
The American Headache Society. Position statement on integrating new migraine treatments into clinical practice. Headache. 2019;59(1):1–18.
Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–9.
Lipton RB. Headache horizons: the promise of dual treatment for migraine. Practical Neurology. 2021. https://practicalneurology.com/articles/2021-oct/headache-horizons-the-promise-of-dual-treatment-for-migraine. Accessed 21 June 2022.
Overeem LH, Raffaelli B, Mecklenburg J, Kelderman T, Neeb L, Reuter U. Indirect comparison of topiramate and monoclonal antibodies against CGRP or its receptor for the prophylaxis of episodic migraine: a systematic review with meta-analysis. CNS Drugs. 2021;35(8):805–20.
Diener HC, Tassorelli C, Dodick DW, et al. Guidelines of the International Headache Society for controlled trials of preventive treatment of migraine attacks in episodic migraine in adults. Cephalalgia. 2020;40(10):1026–44.
Di Tanna GL, Porter JK, Lipton RB, et al. Migraine day frequency in migraine prevention: longitudinal modelling approaches. BMC Med Res Methodol. 2019;19(1):20.
Mahon R, Huels J, Hacking V, et al. Economic evaluations in migraine: systematic literature review and a novel approach. J Med Econ. 2020;23(8):864–76.
Porter JK, Di Tanna GL, Lipton RB, Sapra S, Villa G. Costs of acute headache medication use and productivity losses among patients with migraine: insights from three randomized controlled trials. Pharmacoecon Open. 2019;3(3):411–7.
Ornello R, Casalena A, Frattale I, et al. Real-life data on the efficacy and safety of erenumab in the Abruzzo region, central Italy. J Headache Pain. 2020;21(1):32.
Robblee J, Devick KL, Mendez N, Potter J, Slonaker J, Starling AJ. Real-world patient experience with erenumab for the preventive treatment of migraine. Headache. 2020;60(9):2014–25.
Medicaid.gov. February 2021 Medicaid & CHIP enrollment data highlights. https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html. Accessed 12 Sept 2022.
Benefits.gov. Medicaid Program. https://www.benefits.gov/benefit/606. Accessed 12 Sept 2022.
Silberstein SD, Lee L, Gandhi K, Fitzgerald T, Bell J, Cohen JM. Health care resource utilization and migraine disability along the migraine continuum among patients treated for migraine. Headache. 2018;58(10):1579–92.
Pennsylvania Department of Human Services. Prior authorization of migraine prevention agents (formerly antimigraine agents, other)—pharmacy services. 2020. https://www.dhs.pa.gov/providers/Pharmacy-Services/Documents/Clinical%20Guidelines%20SW%20PDL/Migraine%20Prevention%20Agents%2001.03.22.pdf. Accessed 12 Sept 2022.
Medi-Cal. Injections: drugs E-H policy—Eptinezumab-jjmr injection (Vyepti™). 2021. https://files.medi-cal.ca.gov/pubsdoco/publications/masters-mtp/part2/injectdruge-h.pdf. Accessed 12 Sept 2022.
American Heart Association. Fact sheet: critical coverage for heart health: medicaid and cardiovascular disease. https://www.heart.org/-/media/Files/About-Us/Policy-Research/Fact-Sheets/Access-to-Care/Medicaid-and-CVD-Fact-Sheet.pdf. Accessed 12 Sept 2022.
Chapel JM, Ritchey MD, Zhang D, Wang G. Prevalence and medical costs of chronic diseases among adult medicaid beneficiaries. Am J Prev Med. 2017;53(6s2):S143–54.
D’Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743–53.
Nguyen JL, Munshi K, Peasah SK, et al. Trends in utilization and costs of migraine medications, 2017–2020. J Headache Pain. 2022;23(1):111.
Khanal S, Underwood M, Naghdi S, et al. A systematic review of economic evaluations of pharmacological treatments for adults with chronic migraine. J Headache Pain. 2022;23(1):122.
Dolan R. Understanding the Medicaid prescription drug rebate program. Kaiser Family Foundation. 2019. https://www.kff.org/medicaid/issue-brief/understanding-the-medicaid-prescription-drug-rebate-program/. Accessed 21 June 2022.
Medicaid.gov. State Drug Utilization Data FAQs. 2021. https://www.medicaid.gov/medicaid/prescription-drugs/state-drug-utilization-data/state-drug-utilization-data-faq/index.html. Accessed 21 June 2022.
Gifford K, Winter A, Wiant L, Dolan R, Tian M, Garfield R. How state Medicaid programs are managing prescription drug costs: results from a State Medicaid Pharmacy Survey for state fiscal years 2019 and 2020. Kaiser Family Foundation. 2020. https://www.kff.org/report-section/how-state-medicaid-programs-are-managing-prescription-drug-costs-pharmacy-benefit-administration/. Accessed 21 June 2022.
Medicaid.gov. State Drug Utilization Data FAQs—what are the data field descriptions for the State Drug Utilization Data (SDUD)? 2021. https://www.medicaid.gov/medicaid/prescription-drugs/state-drug-utilization-data/state-drug-utilization-data-faq/index.html. Accessed 21 June 2022.
United States Food and Drug Administration. National Drug Code Directory. Current through 11/05/2020. https://www.accessdata.fda.gov/scripts/cder/ndc/index.cfm. Accessed 12 Sept 2022.
Sun H, Dodick DW, Silberstein S, et al. Safety and efficacy of AMG 334 for prevention of episodic migraine: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Neurol. 2016;15(4):382–90.
Tepper S, Ashina M, Reuter U, et al. Safety and efficacy of erenumab for preventive treatment of chronic migraine: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol. 2017;16(6):425–34.
Goadsby PJ, Reuter U, Hallström Y, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med. 2017;377(22):2123–32.
Kaiser Family Foundation. State health facts—share of Medicaid population covered under different delivery systems. 2019. https://www.kff.org/medicaid/state-indicator/share-of-medicaid-population-covered-under-different-delivery-systems/?currentTimeframe=0&sortModel=%7B. Accessed 21 June 2022.
Kaiser Family Foundation. State health facts—total monthly Medicaid/CHIP enrollment and pre-ACA enrollment. 2019. https://www.kff.org/health-reform/state-indicator/total-monthly-medicaid-and-chip-enrollment/?currentTimeframe=22&sortModel=%7B. Accessed 21 June 2022.
Harris L, L’Italien G, O’Connell T, Hasan Z, Hutchinson S, Lucas S. A framework for estimating the eligible patient population for new migraine acute therapies in the United States. Adv Ther. 2021;38(10):5087–97.
Harris L, L’Italien G, Croop R, et al. Estimated migraine patient population in England progressing beyond first-line acute management. Value Health. 2021;25(1):S140.
Institute for Clinical and Economic Review. Acute treatments for migraine—final evidence report. 2020. https://icer-review.org/wp-content/uploads/2019/06/ICER_Acute-Migraine_Final-Evidence-Report_updated_030320.pdf. Accessed 21 June 2022.
Torres-Ferrús M, Quintana M, Fernandez-Morales J, Alvarez-Sabin J, Pozo-Rosich P. When does chronic migraine strike? A clinical comparison of migraine according to the headache days suffered per month. Cephalalgia. 2017;37(2):104–13.
Lipton RB, Brennan A, Palmer S, et al. Estimating the clinical effectiveness and value-based price range of erenumab for the prevention of migraine in patients with prior treatment failures: a US societal perspective. J Med Econ. 2018;21(7):666–75.
RED BOOK Online. IBM Micromedex [database online]. https://www.micromedexsolutions.com. Accessed 12 Sept 2022.
Institute for Clinical and Economic Review. Calcitonin gene-related peptide (CGRP) Inhibitors as preventive treatments for patients with episodic or chronic migraine: effectiveness and value—final evidence report. 2018. https://icer.org/wp-content/uploads/2020/10/ICER_Migraine_Final_Evidence_Report_070318-1.pdf. Accessed 12 Sept 2022.
Cameron C, Kelly S, Hsieh SC, et al. Triptans in the acute treatment of migraine: a systematic review and network meta-analysis. Headache. 2015;55(Suppl 4):221–35.
Loo LS, Plato BM, Turner IM, et al. Effect of a rescue or recurrence dose of lasmiditan on efficacy and safety in the acute treatment of migraine: findings from the phase 3 trials (SAMURAI and SPARTAN). BMC Neurol. 2019;19(1):191.
Lipton RB, Dodick DW, Ailani J, et al. Effect of ubrogepant vs placebo on pain and the most bothersome associated symptom in the acute treatment of migraine: the ACHIEVE II randomized clinical trial. JAMA. 2019;322(19):1887–98.
Shafqat R, Flores-Montanez Y, Delbono V, Nahas SJ. Updated evaluation of IV dihydroergotamine (DHE) for refractory migraine: patient selection and special considerations. J Pain Res. 2020;13:859–64.
Nurtec ODT prescribing information. 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/212728s006lbl.pdf. Accessed 21 June 2022.
Aimovig prescribing information. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761077s011lbl.pdf. Accessed 21 June 2022.
Ajovy prescribing information. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761089s013lbl.pdf. Accessed 21 June 2022.
Emgality prescrbing information. 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761063s004lbl.pdf. Accessed 21 June 2022.
Vyepti prescribing information. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761119s002lbl.pdf. Accessed 21 June 2022.
Acknowledgements
Funding
Biohaven Pharmaceuticals, Inc. sponsored the analysis and development of the manuscript and funded the Rapid Service fee and the Open Access fee. The authors approved the final version after critically revising the manuscript/publication for important intellectual content. The publication of study results was not contingent on the sponsor’s approval or censorship of the manuscript.
Medical Writing and/or Editorial Assistance
The authors would like to thank Chris Caiazza for medical writing support, which was funded by Biohaven Pharmaceuticals, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors conducted final review and approval of the manuscript, and contributed to the concept and design of the research, appraisal of results of the targeted literature review, and/or drafting of the manuscript. JW and TO conducted data analyses described in the manuscript.
Disclosures
James A. Moren has received compensation as a consultant for Allergan/AbbVie, Biohaven Pharmaceuticals, Eli Lilly and Company, and Teva Pharmaceuticals. Linda Harris, Gilbert L’Italien, Tamela Martin, and Vladimir Coric are employed by and hold stock/stock options in Biohaven Pharmaceuticals, Inc. Tom O’Connell and Jonathan J. Woolley are employees of Medicus Economics, LLC, a paid consultant of Biohaven Pharmaceuticals, Inc. Biohaven Pharmaceuticals paid the publication charges for this piece, via reimbursement to Medicus Economics.
Compliance with Ethics Guidelines
The analysis reported is based on previously conducted studies and public-use data and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Harris, L., O’Connell, T., Woolley, J.J. et al. Observational Analysis of the Costs Associated with Acute Treatment of Breakthrough Migraine Attacks in Medicaid Patients Using Preventive Therapies. Adv Ther 40, 1141–1152 (2023). https://doi.org/10.1007/s12325-022-02386-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02386-w