Abstract
Introduction
This study aims to examine the medication prescriptions for hypertension in Tianjin.
Methods
Patients with hypertension in Tianjin were enrolled in this study. The patients’ ages ranged from 35 to 75 years. A questionnaire survey and physical examination were completed to collect clinical data. Thereafter, a statistical analysis of the medication prescriptions was conducted with different age groups and different grades of hypertension.
Results
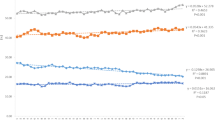
The results show that, in the total population, and for the young, middle-aged, and older groups, the proportions of single-drug use were 62.97%, 59.26%, 62.76%, and 63.49%, respectively, and the highest rate was for calcium channel blocker (CCB) use. The rates of the two drug classes were 24.51%, 29.63%, 25.13%, and 23.15%, respectively. The drug use rate of CCBs combined with angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor antagonists (ARBs) was the highest. The rates of the three drug classes were 4.08%, 4.94%, 4.36%, and 3.52%, respectively, and the highest was ACEI/ARB and CCB combined with diuretics. The rates of the four drug classes were low. Regarding the hypertension grade, in grade 1, grade 2, and grade 3, the rates of single-drug use were 63.53%, 62.69%, and 58.38%, respectively. The rates of the two drug classes were 24.62%, 23.97%, and 25.05%, while the rates of the three drug classes were 3.86%, 4.39%, and 5.34%, respectively.
Conclusion
The rate of single-drug use was high, and the rate of combined drug use in the youth group was slightly higher than in the middle-aged and older age groups. The combination of two drugs was common. In grades 2 and 3 hypertension, the rate of combined drug use remained low.




Similar content being viewed by others
References
Ab Majid NL, Omar MA, Khoo YY, Naidu BM, Yn JL, Hasani WS, Rifin HM, Abd Hamid HA, Lourdes TG, Yusoff MF. Prevalence, awareness, treatment and control of hypertension in the Malaysian population: findings from the National Health and Morbidity Survey 2006–2015. J Human Hypertens. 2018;32(8–9):617–24.
Diaconu CC, Dediu GN, Iancu MA. Drug-induced arterial hypertension—a frequently ignored cause of secondary hypertension: a review. Acta Cardiol. 2018;1:1–7.
Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, Harris KC, Nakhla M, Cloutier L, Gelfer M, et al. Hypertension Canada's 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34(5):506–25.
Skeete J, Connell K, Ordunez P, DiPette DJ. The American College of Cardiology/American Heart Association 2017 hypertension guideline: implications for incorporation in Latin America, the Caribbean, and other resource-limited settings. J Clin Hypertens. 2018;20(9):1342–9.
Ab Majid NL, Omar MA, Khoo YY, Naidu BM, Yn JL, Hasani WS, Rifin HM, Abd Hamid HA, Lourdes TG, Yusoff MF. Prevalence, Awareness, Treatment and Control of hypertension in the Malaysian population: findings from the National Health and Morbidity Survey 2006–2015. J Human Hypertens. 2018;32(8–9):617–24.
Li Y, Wang L, Feng X, Zhang M, Huang Z, Deng Q, Zhou M, Astell-Burt T, Wang L. Geographical variations in hypertension prevalence, awareness, treatment and control in China: findings from a nationwide and provincially representative survey. J Hypertens. 2018;36(1):178–87.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, Su M, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390(10112):2549–58.
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, Bahonar A, Chifamba J, Dagenais G, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–68.
Gąsowski J, Piotrowicz K, Messerli FH. Arterial hypertension after age 65: from epidemiology and pathophysiology to therapy Do we know where we stand. Kardiol Pol. 2018;76(4):723–30.
Hering D, Kucharska W, Chrostowska M, Narkiewicz K. Age-dependent sympathetic neural responses to ß1 selective beta-blockade in untreated hypertension-related tachycardia. Blood Press. 2018;27(3):158–65.
Ishida T, Akinori Oh, Hiroi S, Shimasaki Y, Tsuchihashi T. Current use of antihypertensive drugs in Japanese patients with hypertension: analysis by age group. Geriatr Gerontol Int. 2018;18(6):899–906.
Cuspidi C, Tadic M, Grassi G, Mancia G. Treatment of hypertension: The ESH/ESC guidelines recommendations. Pharmacol Res. 2018;128:315–21.
Peng S, Shen T, Liu J, Tomlinson B, Sun H, Chen X, Chan P, Kuang YaShu, Zheng L, et al. Uncontrolled hypertension increases with age in an older community-dwelling chinese population in Shanghai. Aging Dis. 2017;8(5):558–69.
Derington CG, et al. Trends in antihypertensive medication monotherapy and combination use among US adults, national health and nutrition examination survey 2005–2016. Hypertension. 2020;75:973–81.
Nowak R, Kucharska W, Boutouyrie P. Sympathetic nerve activity is independently linked to geometric and elastic properties of common carotid artery in resistant hypertension. J Hypertens. 2017;35:e76–e7777.
Matsukawa T, Mano T, Gotoh E, Ishii M. Elevated sympathetic nerve activity in patients with accelerated essential hypertension. J Clin Investig. 1993;92(1):25–8.
Yamada Y, Miyajima E, Tochikubo O, Matsukawa T, Ishii M. Age-related changes in muscle sympathetic nerve activity in essential hypertension. Hypertension. 1989;13(6 Pt 2):870–7.
Collins KJ. Age-related changes in autonomic control: the use of beta blockers in the treatment of hypertension. Cardiovasc Drugs Ther. 1991;4(Suppl 6):1257–62.
Kuyper LM, Khan NA. Atenolol vs nonatenolol β-blockers for the treatment of hypertension: a meta-analysis. Can J Cardiol. 2014;30(5 Suppl):S47–53.
Gonzalez MC, Cohen HW, Sealey JE, Laragh JH, Alderman MH. Enduring direct association of baseline plasma renin activity with all-cause and cardiovascular mortality in hypertensive patients. Am J Hypertens. 2011;24(11):1181–6.
Egan BM, Basile JN, Rehman SU, Davis PB, Grob CH III, Riehle JF, Walters CA, Lackland DT, Merali C, Sealey JE, Laragh JH. Plasma Renin test-guided drug treatment algorithm for correcting patients with treated but uncontrolled hypertension: a randomized controlled trial. Am J Hypertens. 2009;22(7):792–801.
Acknowledgements
Funding
This work was supported by the innovative demonstration project of Tianjin Hypertension and Coronary Heart Disease Prevention and Management Service Model and Department of Science and Technology of Tianjin city (15ZXHLSY00320) and the prevention and treatment of hypertension control target values of different risk stratification population and Department of Science and Technology of Tianjin city in Tianjin (16ZXMJSY00140).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Yingyi Zhang, Hua Yang, Ruiying Wang, Fumei Zhao, Ting Liu, Ying Zhang, Zhigang Guo and Hongliang Cong have nothing to disclose.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments and approved by the ethics committee of Tianjin Chest Hospital. All participants provided written informed consent to participate in the study.
Data Availability
All data generated or analyzed during this study are included in this published article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
This article is published with digital features to facilitate understanding of the article. You can access the digital features on the article’s associated Figshare page. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12793880.
Rights and permissions
About this article
Cite this article
Zhang, Y., Yang, H., Wang, R. et al. An Analysis of Medication Prescriptions for Hypertension in Urban and Rural Residents in Tianjin. Adv Ther 37, 4414–4426 (2020). https://doi.org/10.1007/s12325-020-01475-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01475-y