Abstract
Introduction
Although low-density lipoprotein cholesterol (LDL-C) is the primary lipid target for coronary heart disease (CHD) risk reduction, high-density lipoprotein cholesterol (HDL-C) and triglycerides (TG) have also emerged as CHD risk factors. The objective of this study was to evaluate attainment of lipid goals and normal levels following lipid-modifying therapy (LMT) and its predictors in a representative sample of Chinese patients from Hong Kong.
Methods
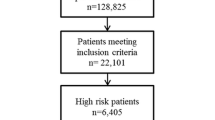
Using longitudinal data collected from patient medical records, the study identified 706 patients who initiated LMT from January 2004 to December 2006 and had full lipid panels 12 months before and after therapy. LDL-C goals and normal levels of HDL-C and TG were defined according to the National Cholesterol Education Program Adult Treatment Panel 3 guidelines. Patients with previous CHD, diabetes, and 10-year CHD risk > 20% were classified as high risk. Multiple logistic regressions evaluated predictors of normal lipid-level attainment.
Results
Among 706 patients (mean age 64.6 years, 58.6% male), 71.7% had elevated LDL-C, 32.4% had low HDL-C, and 24.9% had elevated TG before LMT. Despite therapy (91.2% statins only), 22.7% had elevated LDL-C, 31.9% had low HDL-C, 12.3% had elevated TG, and 13.9% had multiple abnormal lipid levels. The strongest predictors of attaining ≥ 2 normal lipid levels included male gender (odds ratio [OR]: 2.11 [1.12 to 4.01]), diabetes (OR: 0.43 [0.23 to 0.78]), obesity (OR: 0.91 [0.86 to 0.97]), and CHD risk > 20% (OR: 0.33 [0.15 to 0.71]).
Conclusions
Current approaches to lipid management in Hong Kong, primarily using statins, considerably improve attainment of LDL-C goal. However, a large proportion of patients do not achieve normal HDL-C levels and control of multiple lipid parameters remains poor. Patients could benefit from a more comprehensive approach to lipid management that treats all three lipid risk factors, as suggested in clinical guidelines.
Similar content being viewed by others

References
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421.
British Cardiac Society, British Hypertension Society, Diabetes UK, HEART UK, Primary Care Cardiovascular Society, Stroke Association. JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005;91(Suppl. 5):v1–52.
Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14(Suppl. 2):S1–113.
Chirovsky DR, Fedirko V, Cui Y, Sazonov V, Barter P. Prospective studies on the relationship between high-density lipoprotein cholesterol and cardiovascular risk: a systematic review. Eur J Cardiovasc Prev Rehabil. 2009;16:404–423.
Prospective Studies Collaboration; Lewington S, Whitlock G, Clark R, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370:1829–1839.
Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a metaanalysis of population-based prospective studies. J Cardiovasc Risk. 1996;3:213–219.
Abdel-Maksoud M, Sazonov V, Gutkin SW, Hokanson JE. Effects of modifying triglycerides and triglyceride-rich lipoproteins on cardiovascular outcomes. J Cardiovasc Pharmacol. 2008;51:331–351.
Singh IM, Shishehbor MH, Ansell BJ. High-density lipoprotein as a therapeutic target: a systematic review. JAMA. 2007;298:786–798.
Haffner SM, American Diabetes Association. Dyslipidemia management in adults with diabetes. Diabetes Care. 2004;27(Suppl. 1):S68–S71.
Rodbard HW, Blonde L, Braithwaite SS, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract. 2007;13(Suppl. 1):1–68.
Nichols GA, Ambegaonkar BM, Sazonov V, Brown JB. Frequency of obtaining national cholesterol education program adult treatment panel III goals for all major serum lipoproteins after initiation of lipid altering therapy. Am J Cardiol. 2009;104:1689–1694.
Van Ganse E, Laforest L, Burke T, Phatak H, Souchet T. Mixed dyslipidemia among patients using lipidlowering therapy in French general practice: an observational study. Clin Ther. 2007;29:1671–1681.
Lozano JV, Pallares V, Cea-Calvo L, et al. Serum lipid profiles and their relationship to cardiovascular disease in the elderly: the PREVICTUS study. Curr Med Res Opin. 2008;24:659–670.
Cheng CW, Woo KS, Chan JC, Tomlinson B, You JH. Association between adherence to statin therapy and lipid control in Hong Kong Chinese patients at high risk of coronary heart disease. Br J Clin Pharmacol. 2004;58:528–535.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239.
Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1991;121(Pt 2):293–298.
Ghandehari H, Kamal-Bahl S, Wong ND. Prevalence and extent of dyslipidemia and recommended lipid levels in US adults with and without cardiovascular comorbidities: the National Health and Nutrition Examination Survey 2003–2004. Am Heart J. 2008;156:112–119.
Birjmohun RS, Hutten BA, Kastelein JJ, Stroes ES. Efficacy and safety of high-density lipoprotein cholesterol-increasing compounds: a meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2005;45:185–197.
Guyton JR, Bays HE. Safety considerations with niacin therapy. Am J Cardiol. 2007;99:22–31C.
Maccubbin D, Koren MJ, Davidson M, et al. Flushing profile of extended-release niacin/laropiprant versus gradually titrated niacin extended-release in patients with dyslipidemia with and without ischemic cardiovascular disease. Am J Cardiol. 2009;104:74–81.
Bays HE, Shah A, Lin J, et al. Efficacy and tolerability of extended-release niacin/laropiprant in dyslipidemic patients with metabolic syndrome. J Clin Lipidol. 2010;4:515–521.
Canner PL, Berge KG, Wenger NK, et al. Fifteen year mortality in Coronary Drug Project patients: long-term benefit with niacin. J Am Coll Cardiol. 1986;8:1245–1255.
Carlson LA, Rosenhamer G. Reduction of mortality in the Stockholm Ischaemic Heart Disease Secondary Prevention Study by combined treatment with clofibrate and nicotinic acid. Acta Med Scand. 1988;223:405–418.
Clofibrate and niacin in coronary heart disease. JAMA. 1975;231:360–381.
Brown BG, Zhao XQ, Chait A, et al. Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. N Engl J Med. 2001;345:1583–1592.
AIM-HIGH Investigators; Boden WE, Probstfield JL, Anderson T, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365:2255–2267.
Frick MH, Elo O, Haapa K, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987;317:1237–1245.
Manninen V, Tenkanen L, Koskinen P, et al. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study. Implications for treatment. Circulation. 1992;85:37–45.
Robins SJ, Collins D, Wittes JT, et al. Relation of gemfibrozil treatment and lipid levels with major coronary events: VA-HIT: a randomized controlled trial. JAMA. 2001;285:1585–1591.
Keech A, Simes RJ, Barter P, et al. Effects of longterm fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005;366:1849–1861.
The BIP Study Group. Secondary prevention by raising HDL cholesterol and reducing triglycerides in patients with coronary artery disease: the Bezafibrate Infarction Prevention (BIP) study. Circulation. 2000;102:21–27.
Meade T, Zuhrie R, Cook C, Cooper J. Bezafibrate in men with lower extremity arterial disease: randomised controlled trial. BMJ. 2002;325:1139.
ACCORD Study Group; Ginsberg HN, Elam MB, Lovato LC, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362:1563–1574.
Harris WS. N-3 fatty acids and serum lipoproteins: human studies. Am J Clin Nutr. 1997;65(Suppl.):1645–1654S.
Kush D, Hu DY, Ye P, et al. Flushing profile of extended-release niacin/laropiprant at initiation of therapy in Asian lipid clinic patients. Cardiology. 2009;114:192–198.
Lee ZS, Critchley JA, Chan JC, et al. Obesity is the key determinant of cardiovascular risk factors in the Hong Kong Chinese population: crosssectional clinic-based study. Hong Kong Med J. 2000;6:13–23.
Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–2716.
McNeill AM, Rosamond WD, Girman CJ, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005;28:385–390.
Rutter MK, Meigs JB, Sullivan LM, D’Agostino RB Sr, Wilson PW. C-reactive protein, the metabolic syndrome, and prediction of cardiovascular events in the Framingham Offspring Study. Circulation. 2004;110:380–385.
Author information
Authors and Affiliations
Corresponding author
Additional information
To view enhanced content go to www.advancesintherapy.com
Rights and permissions
About this article
Cite this article
Ambegaonkar, B., Chirovsky, D., Tse, H.F. et al. Attainment of Normal Lipid Levels Among Patients on Lipid-Modifying Therapy in Hong Kong. Adv Therapy 29, 427–441 (2012). https://doi.org/10.1007/s12325-012-0017-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-012-0017-9