Abstract
Lymph node (LN) targeting through interstitial drainage of nanoparticles (NPs) is an attractive strategy to stimulate a potent immune response, as LNs are the primary site for lymphocyte priming by antigen presenting cells (APCs) and triggering of an adaptive immune response. NP size has been shown to influence the efficiency of LN-targeting and retention after subcutaneous injection. For clinical translation, biodegradable NPs are preferred as carrier for vaccine delivery. However, the selective “size gate” for effective LN-drainage, particularly the kinetics of LN trafficking, is less well defined. This is partly due to the challenge in generating size-controlled NPs from biodegradable polymers in the sub-100-nm range. Here, we report the preparation of three sets of poly(lactic-co-glycolic)-b-poly(ethylene-glycol) (PLGA-b-PEG) NPs with number average diameters of 20-, 40-, and 100-nm and narrow size distributions using flash nanoprecipitation. Using NPs labeled with a near-infrared dye, we showed that 20-nm NPs drain rapidly across proximal and distal LNs following subcutaneous inoculation in mice and are retained in LNs more effectively than NPs with a number average diameter of 40-nm. The drainage of 100-nm NPs was negligible. Furthermore, the 20-nm NPs showed the highest degree of penetration around the paracortex region and had enhanced access to dendritic cells in the LNs. Together, these data confirmed that small, size-controlled PLGA-b-PEG NPs at the lower threshold of about 30-nm are most effective for LN trafficking, retention, and APC uptake after s.c. administration. This report could inform the design of LN-targeted NP carrier for the delivery of therapeutic or prophylactic vaccines.

Similar content being viewed by others
References
Trevaskis, N. L.; Kaminskas, L. M.; Porter, C. J. H. From sewer to saviour-targeting the lymphatic system to promote drug exposure and activity. Nat. Rev. Drug Discov. 2015, 14, 781–803.
Willard-Mack, C. L. Normal structure, function, and histology of lymph nodes. Toxicol. Pathol. 2006, 34, 409–424.
Wilson, N. S.; El-Sukkari, D.; Belz, G. T.; Smith, C. M.; Steptoe, R. J.; Heath, W. R.; Shortman, K.; Villadangos, J. A. Most lymphoid organ dendritic cell types are phenotypically and functionally immature. Blood 2003, 102, 2187–2194.
Swartz, M. A.; Hubbell, J. A.; Reddy, S. T. Lymphatic drainage function and its immunological implications: From dendritic cell homing to vaccine design. Semin. Immunol. 2008, 20, 147–156.
Tostanoski, L. H.; Chiu, Y.-C.; Gammon, J. M.; Simon, T.; Andorko, J. I.; Bromberg, J. S.; Jewell, C. M. Reprogramming the local lymph node microenvironment promotes tolerance that is systemic and antigen specific. Cell Rep. 2016, 16, 2940–2952.
Supsersaxo, A.; Hein, W. R.; Steffen, H. Effect of molecular weight on the lymphatic absorption of water-soluble compounds following subcutaneous administration. Pharm. Res. 1990, 7, 167–169.
Oussoren, C.; Storm, G. Liposomes to target the lymphatics by subcutaneous administration. Adv. Drug Deliv. Rev. 2001, 50, 143–156.
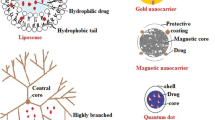
Kaminskas, L. M.; Porter, C. J. H. Targeting the lymphatics using dendritic polymers (dendrimers). Adv. Drug Deliv. Rev. 2011, 63, 890–900.
Reddy, S. T.; Rehor, A.; Schmoekel, H. G.; Hubbell, J. A.; Swartz, M. A. In vivo targeting of dendritic cells in lymph nodes with poly(propylene sulfide) nanoparticles. J. Control. Release 2006, 112, 26–34.
Reddy, S. T.; van der Vlies, A. J.; Simeoni, E.; Angeli, V.; Randolph, G. J.; O’Neil, C. P.; Lee, L. K.; Swartz, M. A.; Hubbell, J. A. Exploiting lymphatic transport and complement activation in nanoparticle vaccines. Nat. Biotechnol. 2007, 25, 1159–1164.
Mottram, P. L.; Leong, D.; Crimeen-Irwin, B.; Gloster, S.; Xiang, S. D.; Meanger, J.; Ghildyal, R.; Vardaxis, N.; Plebanski, M. Type 1 and 2 immunity following vaccination is influenced by nanoparticle size: Formulation of a model vaccine for respiratory syncytial virus. Mol. Pharm. 2007, 4, 73–84.
Fifis, T.; Gamvrellis, A.; Crimeen-Irwin, B.; Pietersz, G. A.; Li, J.; Mottram, P. L.; McKenzie, I. F.; Plebanski, M. Size-dependent immunogenicity: Therapeutic and protective properties of nano-vaccines against tumors. J. Immunol. 2004, 173, 3148–3154.
Kumar, S.; Anselmo, A. C.; Banerjee, A.; Zakrewsky, M.; Mitragotri, S. Shape and size-dependent immune response to antigen-carrying nanoparticles. J. Control. Release 2015, 220, 141–148.
Manolova, V.; Flace, A.; Bauer, M.; Schwarz, K.; Saudan, P.; Bachmann, M. F. Nanoparticles target distinct dendritic cell populations according to their size. Eur. J. Immunol. 2008, 38, 1404–1413.
Randolph, G. J.; Angeli, V.; Swartz, M. A. Dendritic-cell trafficking to lymph nodes through lymphatic vessels. Nat. Rev. Immunol. 2005, 5, 617–628.
Li, X. R.; Sloat, B. R.; Yanasarn, N.; Cui, Z. R. Relationship between the size of nanoparticles and their adjuvant activity: Data from a study with an improved experimental design. Eur. J. Pharm. Biopharm. 2011, 78, 107–116.
Chaney, E. J.; Tang, L.; Tong, R.; Cheng, J. J.; Boppart, S. A. Lymphatic biodistribution of polylactide nanoparticles. Mol. Imaging 2010, 9, 153–162.
Rao, D. A.; Forrest, M. L.; Alani, A. W. G.; Kwon, G. S.; Robinson, J. R. Biodegradable PLGA based nanoparticles for sustained regional lymphatic drug delivery. J. Pharm. Sci. 2010, 99, 2018–2031.
Zheng, S. S.; Qin, T.; Lu, Y.; Huang, Y. F.; Luo, L.; Liu, Z. G.; Bo, R. N.; Hu, Y. L.; Liu, J. G.; Wang, D. Y. Maturation of dendritic cells in vitro and immunological enhancement of mice in vivo by pachyman-and/or OVA-encapsulated poly(D, L-lactic acid) nanospheres. Int. J. Nanomedicine 2018, 13, 569–583.
Zhang, W. F.; Wang, L. Y.; Liu, Y.; Chen, X. M.; Liu, Q.; Jia, J. L.; Yang, T. Y.; Qiu, S. H.; Ma, G. H. Immune responses to vaccines involving a combined antigen-nanoparticle mixture and nanoparticle-encapsulated antigen formulation. Biomaterials 2014, 35, 6086–6097.
Maldonado, R. A.; LaMothe, R. A.; Ferrari, J. D.; Zhang, A. H.; Rossi, R. J.; Kolte, P. N.; Griset, A. P.; O’Neil, C.; Altreuter, D. H.; Browning, E. et al. Polymeric synthetic nanoparticles for the induction of antigen-specific immunological tolerance. Proc. Natl. Acad. Sci. USA 2015, 112, E156–E165.
Johnson, B. K.; Prud’homme, R. K. Mechanism for rapid self-assembly of block copolymer nanoparticles. Phys. Rev. Lett. 2003, 91, 118302.
Saad, W. S.; Prud’homme, R. K. Principles of nanoparticle formation by flash nanoprecipitation. Nano Today 2016, 11, 212–227.
Xiang, S. D.; Scholzen, A.; Minigo, G.; David, C.; Apostolopoulos, V.; Mottram, P. L.; Plebanski, M. Pathogen recognition and development of particulate vaccines: Does size matter?. Methods 2006, 40, 1–9.
Harrell, M. I.; Iritani, B. M.; Ruddell, A. Lymph node mapping in the mouse. J. Immunol. Methods 2008, 332, 170–174.
Reddy, S. T.; Berk, D. A.; Jain, R. K.; Swartz, M. A. A sensitive in vivo model for quantifying interstitial convective transport of injected macromolecules and nanoparticles. J. Appl. Physiol. 2006, 101, 1162–1169.
Tomura, M.; Hata, A.; Matsuoka, S.; Shand, F. H. W.; Nakanishi, Y.; Ikebuchi, R.; Ueha, S.; Tsutsui, H.; Inaba, K.; Matsushima, K. et al. Tracking and quantification of dendritic cell migration and antigen trafficking between the skin and lymph nodes. Sci. Rep. 2014, 4, 6030.
Thomas, S. N.; Schudel, A. Overcoming transport barriers for interstitial-, lymphatic-, and lymph node-targeted drug delivery. Curr. Opin. Chem. Eng. 2015, 7, 65–74.
Sixt, M.; Kanazawa, N.; Selg, M.; Samson, T.; Roos, G.; Reinhardt, D. P.; Pabst, R.; Lutz, M. B.; Sorokin, L. The conduit system transports soluble antigens from the afferent lymph to resident dendritic cells in the T cell area of the lymph node. Immunity 2005, 22, 19–29.
Roozendaal, R.; Mempel, T. R.; Pitcher, L. A.; Gonzalez, S. F.; Verschoor, A.; Mebius, R. E.; von Andrian, U. H.; Carroll, M. C. Conduits mediate transport of low-molecular-weight antigen to lymph node follicles. Immunity 2009, 30, 264–276.
Phan, T. G.; Grigorova, I.; Okada, T.; Cyster, J. G. Subcapsular encounter and complement-dependent transport of immune complexes by lymph node B cells. Nat. Immunol. 2007, 8, 992–1000.
Kang, S.; Ahn, S.; Lee, J.; Kim, J. Y.; Choi, M.; Gujrati, V.; Kim, H.; Kim, J.; Shin, E. C.; Jon, S. Effects of gold nanoparticle-based vaccine size on lymph node delivery and cytotoxic T-lymphocyte responses. J. Control. Release 2017, 256, 56–67.
Kim, H.; Uto, T.; Akagi, T.; Baba, M.; Akashi, M. Amphiphilic poly(amino acid) nanoparticles induce size-dependent dendritic cell maturation. Adv. Funct. Mater. 2010, 20, 3925–3931.
Hirosue, S.; Kourtis, I. C.; van der Vlies, A. J.; Hubbell, J. A.; Swartz, M. A. Antigen delivery to dendritic cells by poly(propylene sulfide) nanoparticles with disulfide conjugated peptides: Cross-presentation and T cell activation. Vaccine 2010, 28, 7897–7906.
Jiang, H.; Wang, Q.; Sun, X. Lymph node targeting strategies to improve vaccination efficacy. J. Control. Release 2017, 267, 47–56.
Acknowledgements
This work was funded by support from the National Institutes of Health (Nos. R01-AI114609 and T32-OD11089) and NSF GRFP (No. DGE1746891). Partial support was received from the University of Florida Emerging Pathogens Institute.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Howard, G.P., Verma, G., Ke, X. et al. Critical size limit of biodegradable nanoparticles for enhanced lymph node trafficking and paracortex penetration. Nano Res. 12, 837–844 (2019). https://doi.org/10.1007/s12274-019-2301-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12274-019-2301-3