Abstract
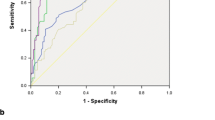
Biomarkers of blood lipid modification and oxidative stress have been associated with increased cardiovascular morbidity. We sought to determine whether these biomarkers were related to functional indices of stenosis severity among patients with stable coronary artery disease. We studied 197 consecutive patients with stable coronary artery disease due to single vessel disease. Fractional flow reserve (FFR) ≤ 0.80 was assessed as index of a functionally significant lesion. Serum levels of secretory phospholipase A2 (sPLA2) activity, secretory phospholipase A2 type IIA (sPLA2-IIA), myeloperoxydase (MPO), lipoprotein-associated phospholipase A2 (Lp-PLA2), and oxidized low-density lipoprotein (OxLDL) were assessed using commercially available assays. Patients with FFR > 0.8 had higher sPLA2 activity, sPLA2 IIA, and OxLDL levels than patients with FFR ≤ 0.8 (21.25 [16.03–27.28] vs 25.85 [20.58–34.63] U/mL, p < 0.001, 2.0 [1.5–3.4] vs 2.6 [2.0–3.4] ng/mL, p < 0.01; and 53.0 [36.0–71.0] vs 64.5 [50–89.25], p < 0.001 respectively). Patients with FFR > 0.80 had similar Lp-PLA2 and MPO levels versus those with FFR ≤ 0.8. sPLA2 activity, sPLA2 IIA significantly increased area under the curve over baseline characteristics to predict FFR ≤ 0.8 (0.67 to 0.77 (95 % confidence interval [CI]: 0.69–0.85) p < 0.01 and 0.67 to 0.77 (95 % CI: 0.69–0.84) p < 0.01, respectively). Serum sPLA2 activity as well as sPLA2-IIA level is related to functional characteristics of coronary stenoses in patients with stable coronary artery disease.




Similar content being viewed by others
Abbreviations
- sPLA2:
-
Secretory phospholipase A2 activity
- sPLA2-IIA:
-
Secretory phospholipase A2 activity type IIA
- MPO:
-
Myeloperoxydase
- Lp-PLA2:
-
Lipoprotein-associated phospholipase A2
- OxLDL:
-
Oxidized low-density lipoprotein
References
Libby, P., Ridker, P. M., & Hansson, G. K. (2009). Inflammation in atherosclerosis: from pathophysiology to practice. Journal of the American College of Cardiology, 54, 2129–2138.
Pratap, P., Gupta, S., & Berlowitz, M. (2012). Routine invasive versus conservative management strategies in acute coronary syndrome: time for a "hybrid" approach. Journal of Cardiovascular Translational Research, 5, 30–40.
Kolodgie, F. D., Burke, A. P., Skorija, K. S., Ladich, E., Kutys, R., Makuria, A. T., et al. (2006). Lipoprotein-associated phospholipase a2 protein expression in the natural progression of human coronary atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology, 26, 2523–2529.
Menschikowski, M., Hagelgans, A., & Siegert, G. (2006). Secretory phospholipase A2 of group IIA: Is it an offensive or a defensive player during atherosclerosis and other inflammatory diseases? Prostaglandins & Other Lipid Mediators, 79, 1–33.
Daugherty, A., Dunn, J. L., Rateri, D. L., & Heinecke, J. W. (1994). Myeloperoxidase, a catalyst for lipoprotein oxidation, is expressed in human atherosclerotic lesions. The Journal of Clinical Investigation, 94, 437–444.
Li, D., & Mehta, J. L. (2005). Oxidized LDL, a critical factor in atherogenesis. Cardiovascular Research, 68, 353–354.
Mallat, Z., Benessiano, J., Simon, T., Ederhy, S., Sebella-Arguelles, C., Cohen, A., et al. (2007). Circulating secretory phospholipase A2 activity and risk of incident coronary events in healthy men and women: the Epic–Norfolk study. Arteriosclerosis, Thrombosis, and Vascular Biology, 27, 1177–1183.
Koenig, W., Vossen, C. Y., Mallat, Z., Brenner, H., Benessiano, J., & Rothenbacher, D. (2009). Association between type II secretory phospholipase A2 plasma concentrations and activity and cardiovascular events in patients with coronary heart disease. European Heart Journal, 30, 2742–2748.
Mallat, Z., Lambeau, G., & Tedgui, A. (2010). Lipoprotein-associated and secreted phospholipases a in cardiovascular disease: roles as biological effectors and biomarkers. Circulation, 122, 2183–2200.
Hamilos, M., Muller, O., Cuisset, T., Ntalianis, A., Chlouverakis, G., Sarno, G., et al. (2009). Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation, 120, 1505–1512.
Ryan, T. J., Faxon, D. P., Gunnar, R. M., Kennedy, J. W., King, S. B., 3rd, Loop, F. D., et al. (1988). Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty). Circulation, 78, 486–502.
De Bruyne, B., & Sarma, J. (2008). Fractional flow reserve: a review: invasive imaging. Heart, 94, 949–959.
Muller, O., Mangiacapra, F., Ntalianis, A., Verhamme, K. M., Trana, C., Hamilos, M., et al. (2011). Long-term follow-up after fractional flow reserve-guided treatment strategy in patients with an isolated proximal left anterior descending coronary artery stenosis. JACC Cardiovasc Interv., 4, 1175–1182.
Kuroda, J., & Sadoshima, J. (2010). NADPH oxidase and cardiac failure. Journal of Cardiovascular Translational Research, 3, 314–320.
Parenica, J., Nemec, P., Tomandl, J., Ondrasek, J., Pavkova-Goldbergova, M., Tretina, M., et al. (2012). Prognostic utility of biomarkers in predicting of one-year outcomes in patients with aortic stenosis treated with transcatheter or surgical aortic valve implantation. PloS One, 7, e48851.
Pijls, N. H., De Bruyne, B., Peels, K., Van der Voort, P. H., Bonnier, H. J., Bartunek, J. K. J. J., et al. (1996). Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. The New England Journal of Medicine, 334, 1703–1708.
De Bruyne, B., Pijls, N. H., Bartunek, J., Kulecki, K., Bech, J. W., De Winter, H., et al. (2001). Fractional flow reserve in patients with prior myocardial infarction. Circulation, 104, 157–162.
Pijls, N. H., Van Gelder, B., Van der Voort, P., Peels, K., Bracke, F. A., Bonnier, H. J., et al. (1995). Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation, 92, 3183–3193.
Wijns, W., Kolh, P., Danchin, N., Di Mario, C., Falk, V., Folliguet, T., et al. (2010). Guidelines on myocardial revascularization. European Heart Journal, 31, 2501–2555.
Tonino, P. A., De Bruyne, B., Pijls, N. H., Siebert, U., Ikeno, F., Van’ t Veer, M., FAME Study Investigators, et al. (2009). Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. The New England Journal of Medicine, 360, 213–224.
Pijls, N. H., van Schaardenburgh, P., Manoharan, G., Boersma, E., Bech, J. W., van't Veer, M., et al. (2007). Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the defer study. Journal of the American College of Cardiology, 49, 2105–2111.
Puymirat, E., Peace, A., Mangiacapra, F., Conte, M., Ntarladimas, Y., Bartunek, J., et al. (2012). Long-term clinical outcome after fractional flow reserve-guided percutaneous coronary revascularization in patients with small-vessel disease. Circulation. Cardiovascular Interventions, 5, 62–68.
De Bruyne, B., Pijls, N. H., Kalesan, B., Barbato, E., Tonino, P. A., Piroth, Z., et al. (2012). Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. The New England Journal of Medicine, 367, 991–1001.
Melikian, N., De Bondt, P., Tonino, P., De Winter, O., Wyffels, E., Bartunek, J., et al. (2010). Fractional flow reserve and myocardial perfusion imaging in patients with angiographic multivessel coronary artery disease. JACC. Cardiovascular Interventions, 3, 307–314.
Beller, G. A., & Heede, R. C. (2011). SPECT imaging for detecting coronary artery disease and determining prognosis by noninvasive assessment of myocardial perfusion and myocardial viability. Journal of Cardiovascular Translational Research, 4, 416–424.
Ragosta, M. (2011). Techniques for phenotyping coronary artery disease in the cardiac catheterization laboratory for applications in translational research. Journal of Cardiovascular Translational Research, 4, 385–392.
Eshtehardi, P., Luke, J., McDaniel, M. C., & Samady, H. (2011). Intravascular imaging tools in the cardiac catheterization laboratory: comprehensive assessment of anatomy and physiology. Journal of Cardiovascular Translational Research, 4, 393–403.
Shaw, L. J., Berman, D. S., Maron, D. J., Mancini, G. B., Hayes, S. W., Hartigan, P. M., et al. (2008). Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: Results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (courage) trial nuclear substudy. Circulation, 117, 1283–1291.
Gibbons, R. J. (2008). Noninvasive diagnosis and prognosis assessment in chronic coronary artery disease: stress testing with and without imaging perspective. Circulation. Cardiovascular Imaging, 1, 257–269. discussion 269.
Casella, G., Leibig, M., Schiele, T. M., Schrepf, R., Seelig, V., Stempfle, H. U., et al. (2004). Are high doses of intracoronary adenosine an alternative to standard intravenous adenosine for the assessment of fractional flow reserve? American Heart Journal, 148, 590–595.
De Luca, G., Venegoni, L., Iorio, S., Giuliani, L., & Marino, P. (2011). Effects of increasing doses of intracoronary adenosine on the assessment of fractional flow reserve. JACC. Cardiovascular Interventions, 4, 1079–1084.
Conflict of Interest
Emanuel Valentin is an employee of Aterovax.
Funding Sources
Meijer Foundation for Cardiac Research, Aalst, Belgium
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muller, O., Ntalianis, A., Wijns, W. et al. Association of Biomarkers of Lipid Modification with Functional and Morphological Indices of Coronary Stenosis Severity in Stable Coronary Artery Disease. J. of Cardiovasc. Trans. Res. 6, 536–544 (2013). https://doi.org/10.1007/s12265-013-9468-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-013-9468-x