Abstract
Segment 7 is considered an unfavorable portion for laparoscopic hepatectomy because of technical difficulties in exposure and controlling bleeding. We compared intermittent Pringle with continuous half-Pringle maneuver in laparoscopic liver resections of tumors in segment 7. A retrospective analysis was conducted in a total of 36 consecutive patients with tumors in segment 7 undergoing laparoscopic liver resections between July 2011 and February 2016 (16 in the Pringle group versus 20 in the half-Pringle group). The two groups were well matched in baseline characteristics. The operative time (274.5 ± 34.3 versus 237.6 ± 41.8 min), overall declamping time (28.4 ± 8.6 versus 2.3 ± 2.5 min), and ischemic duration (69.7 ± 16.5 versus 52.7 ± 13.2 min) were significantly longer in the Pringle group (P < 0.05). The amount of intraoperative blood loss (612.5 ± 222.3 versus 417.4 ± 163.8 mL) and transfusion (335.2 ± 58.7 versus 224.8 ± 76.2 mL) was significantly greater in the Pringle group (P < 0.05). The Pringle group was associated with significantly lower postoperative albumin and higher C-reactive protein levels on postoperative days 1, 3, and 7 (P < 0.05). Laparoscopic hepatectomy for tumors in segment 7 can be performed safely and effectively with successful exposure of surgical field and proper hepatic blood flow occlusion. Continuous half-Pringle maneuver offers the advantages of less operative time and blood loss, less injury, and better recovery.


Similar content being viewed by others
References
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver From Segment I to VIII. Ann Surg 256(6):959–964. https://doi.org/10.1097/SLA.0b013e31825ffed3
Coles SR, Besselink MG, Serin KR, Alsaati H, Di Gioia P, Samim M, Pearce NW, Abu Hilal M (2015) Total laparoscopic management of lesions involving liver segment 7. Surg Endosc 29(11):3190–3195. https://doi.org/10.1007/s00464-014-4052-2
Okuda Y, Honda G, Kurata M, Kobayashi S, Sakamoto K, Takahashi K (2014) A safe and valid procedure for pure laparoscopic partial hepatectomy of the most posterosuperior area: the top of segment 7. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2014.11.021
Zhang Y, Yang H, Chen Y, et al (2015) Totally laparoscopic associating liver tourniquet and portal ligation for staged hepatectomy via anterior approach for cirrhotic hepatocellular carcinoma. J Am Coll Surgeons. https://doi.org/10.1016/j.jamcollsurg.2015.04.016
Zhang Y, Yang H, Deng X, et al (2015) Intermittent Pringle manoeuvre versus continuous hemihepatic vascular inflow occlusion using extra-glissonian approach in laparoscopic liver resection. Surg Endosc. https://doi.org/10.1007/s00464-015-4276-9
Hepp J, Couinaud C (1956) Approach to and use of the left hepatic duct in reparation of the common bile duct. Presse Med 64(41):947–948
Xiang L, Le Xiao JL, Chen J, Fan Y, Zheng S (2015) Safety and feasibility of laparoscopic hepatectomy for hepatocellular carcinoma in the posterosuperior liver segments. World J Surg 39(5):1202–1209. https://doi.org/10.1007/s00268-015-2946-3
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Twaij A, Pucher PH, Sodergren MH, Gall T, Darzi A, Jiao LR (2014) Laparoscopic vs open approach to resection of hepatocellular carcinoma in patients with known cirrhosis: systematic review and meta-analysis. World J Gastroenterol 20(25):8274–8281. https://doi.org/10.3748/wjg.v20.i25.8274
Fuks D, Cauchy F, Ftériche S, Nomi T, Schwarz L, Dokmak S, et al (2015) Laparoscopy decreases pulmonary complications in patients undergoing major liver resection: a propensity score analysis. Ann Surg. https://doi.org/10.1097/SLA.0000000000001140
Siniscalchi A, Ercolani G, Tarozzi G, Gamberini L, Cipolat L, Pinna AD, Faenza S (2014) Laparoscopic versus open liver resection: differences in intraoperative and early postoperative outcome among cirrhotic patients with hepatocellular carcinoma—a retrospective observational study. HPB Surg 2014:1–7. https://doi.org/10.1155/2014/871251
Yamashita Y, Ikeda T, Kurihara T, Yoshida Y, Takeishi K, Itoh S et al (2014) Long-term favorable surgical results of laparoscopic hepatic resection for hepatocellular carcinoma in patients with cirrhosis: a single-center experience over a 10-year period. J Am Coll Surg 219(6):1117–1123. https://doi.org/10.1016/j.jamcollsurg.2014.09.003
Yoon S, Kim K, Jung D, Yu A, Lee S (2014) Oncological and surgical results of laparoscopic versus open liver resection for HCC less than 5 cm: case-matched analysis. Surg Endosc 29(9):2628–2634. https://doi.org/10.1007/s00464-014-3980-1
Ahn KS, Kang KJ, Kim YH, Kim TS, Lim TJ (2014) A propensity score-matched case-control comparative study of laparoscopic and open liver resection for hepatocellular carcinoma. J Laparoendosc Adv Surg Tech A 24(12):872–877. https://doi.org/10.1089/lap.2014.0273
Scatton O, Brustia R, Belli G, Pekolj J, Wakabayashi G, Gayet B (2015) What kind of energy devices should be used for laparoscopic liver resection? Recommendations from a systematic review. J Hepatobiliary Pancreat Sci 22(5):327–334. https://doi.org/10.1002/jhbp.213
Otsuka Y, Kaneko H, Cleary SP, Buell JF, Cai X, Wakabayashi G (2015) What is the best technique in parenchymal transection in laparoscopic liver resection? Comprehensive review for the clinical question on the 2nd International Consensus Conference on Laparoscopic Liver Resection. J Hepatobiliary Pancreat Sci 22(5):363–370. https://doi.org/10.1002/jhbp.216
Si-Yuan FU, Yee LW, Li G-G, Qing-he T, Ai-jun LI, Ze-ya PAN et al (2011) A prospective randomized controlled trial to compare Pringle maneuver, hemihepatic vascular inflow occlusion, and main portal vein inflow occlusion in partial hepatectomy. Am J Surg 201(1):62–69. https://doi.org/10.1016/j.amjsurg.2009.09.029
Ni J-s, Lau WY, Yang Y, Pan Z-Y, Wang Z-g, Liu H, Wu M-c, Zhou W-p (2013) A prospective randomized controlled trial to compare Pringle maneuver, hemihepatic vascular inflow occlusion, and main portal vein inflow occlusion in partial hepatectomy. J Gastrointest Surg 17(8):1414–1421. https://doi.org/10.1007/s11605-013-2236-z
Liang G, Wen T, Yan L, Li BO, Wu G, Yang J, Lu B, Chen Z, Liao Z, Ran S, Yu Z (2009) A prospective randomized comparison of continuous hemihepatic with intermittent total hepatic inflow occlusion in hepatectomy for liver tumors. Hepato-Gastroenterology 56(91-92):745–750
Figueras J, Lopez-Ben S, Llado L, Rafecas A, Torras J, Ramos E et al (2003) Hilar dissection versus the “glissonean” approach and stapling of the pedicle for major hepatectomies: a prospective, randomized trial. Ann Surg 238(1):111–119. https://doi.org/10.1097/01.SLA.0000074981.02000.69
Chen YJ, Zhen ZJ, Chen HW, Lai ECH, Deng FW, Li QH, Lau WY (2014) Laparoscopic liver resection under hemihepatic vascular inflow occlusion using the lowering of hilar plate approach. Hepatobiliary Pancreat Dis Int 13(5):508–512. https://doi.org/10.1016/S1499-3872(14)60293-9
Herman P, Jaime K¨g, Lupinacci R, Coelho F, Perini M (2013) Laparoscopic bisegmentectomy 6 and 7 using a Glissonian approach and a half-Pringle maneuver. Surg Endosc 27(5):1840–1841. https://doi.org/10.1007/s00464-012-2681-x
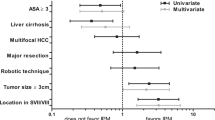
Tranchart H, Gaillard M, Chirica M, Ferretti S, Perlemuter G, Naveau S, Dagher I (2014) Multivariate analysis of risk factors for postoperative complications after laparoscopic liver resection. Surg Endosc 29(9):2538–2544. https://doi.org/10.1007/s00464-014-3965-0
Mizuguchi T, Kawamoto M, Nakamura Y, Meguro M, Hui TT, Hirata K (2015) New technique of extracorporeal hepatic inflow control for pure laparoscopic liver resection. Surg Laparosc Endosc Percutan Tech 25(1):e16–e20. https://doi.org/10.1097/SLE.0b013e3182a4c0f4
Jiang G-Q, Chen P, Qian J-J, Yao J, Wang X-D, Jin S-J, Bai DS (2014) Perioperative advantages of modified laparoscopic vs open splenectomy and azygoportal disconnection. World J Gastroenterol 20(27):9146–9153. https://doi.org/10.3748/wjg.v20.i27.9146
Muscari A, Collini A, Fabbri E, Giovagnoli M, Napoli C, Rossi V et al (2014) Changes of liver enzymes and bilirubin during ischemic stroke: mechanisms and possible significance. BMC Neurol 14:122
Dagher I, Gayet B, Tzanis D, Tranchart H, Fuks D, Soubrane O, Han HS, Kim KH, Cherqui D, O’Rourke N, Troisi RI, Aldrighetti L, Bjorn E, Abu Hilal M, Belli G, Kaneko H, Jarnagin WR, Lin C, Pekolj J, Buell JF, Wakabayashi G (2014) International experience for laparoscopic major liver resection. J Hepatobiliary Pancreat Sci 21(10):732–736. https://doi.org/10.1002/jhbp.140
Xu H, Liu F, Li H, Wei Y, Li B (2017) Outcomes following laparoscopic versus open major hepatectomy: a meta-analysis. Scand J Gastroenterol 7:1–8
Funding
This study was supported by grants from Health Department of Sichuan Province, China, No. 130134 and Doctor Funding of Sichuan Academy of Medical Sciences.
Author information
Authors and Affiliations
Contributions
Yu Zhang and Xiangyu Lu have contributed equally to this work; Yu Zhang, Jian Xu, and Hongji Yang designed the study; Xiangyu Lu, Xiaofan Deng, Chen Kai, and Yunfei Chen collected the patient’s clinical data; Jian Xu analyzed the data and wrote the paper.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Zhang, Y., Lu, X., Xu, J. et al. Intermittent Pringle Versus Continuous Half-Pringle Maneuver for Laparoscopic Liver Resections of Tumors in Segment 7. Indian J Surg 80, 146–153 (2018). https://doi.org/10.1007/s12262-018-1721-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1721-8