Abstract
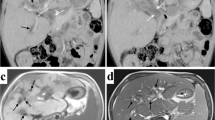
Liver cirrhosis due to secondary sclerosing cholangitis caused by Langerhans cell histiocytosis (LCH) has a poor prognosis, and liver transplantation is the definitive treatment. However, the optimal timing has not been established. We report a 2-year-old girl with LCH-related liver cirrhosis who successfully underwent liver transplantation before progressing to severe liver dysfunction. Physical examination revealed a tumor on her palate. Biopsy was performed, and a diagnosis of LCH was established, together with hepatomegaly, splenomegaly, and rashes. Percutaneous liver biopsy before treatment revealed extreme fibrosis and absence of LCH cells. After beginning chemotherapy, she experienced several delays in treatment and dose reductions because of unacceptable bone marrow suppression, worsening liver dysfunction, and cholangitis. However, tumor shrinkage was observed in both magnetic resonance imaging and BRAF V600E mutant allele titers in her plasma. Given the good treatment response, liver transplantation was conducted. The postoperative course was uneventful, and chemotherapy was resumed 34 days after liver transplantation. Subsequent maintenance treatment was completed with no severe adverse effects. To prevent perioperative complications due to exacerbation of liver dysfunction and possible discontinuation of chemotherapy, liver transplantation should be considered before development of end-stage liver failure, provided that the original disease is well controlled.



Similar content being viewed by others
References
The French Langerhans’ Cell Histiocytosis Study Group. A multicentre retrospective survey of Langerhans’ cell histiocytosis: 348 cases observed between 1983 and 1993 The French Langerhans’ Cell Histiocytosis study group. Arch Dis Child. 1996;75(1):17–24.
Roy C, Silverman A, Alaguille D. Diseases of the liver: prolonged obstructive jaundice including calculous and non calculous gallbladder conditions pediatric clinical gastroenterology St Louis. Missouri. 1995;11(5):636–83.
Zandi P, Panis Y, Debray D, Bernard O, Houssin D. Pediatric liver transplantation for Langerhans’ cell histiocytosis. Hepatology. 1995;21(1):129–33.
Kudo K, Toki T, Kanezaki R, Tanaka T, Kamio T, Sato T, et al. BRAFV600E-positive cells as molecular markers of bone marrow disease in pediatric Langerhans cell histiocytosis. Haematologica. 2022;107(7):1719–25.
Morimoto A, Shioda Y, Imamura T, Kudo K, Kawaguchi H, Sakashita K, et al. Intensified and prolonged therapy comprising cytarabine, vincristine and prednisolone improves outcome in patients with multisystem Langerhans cell histiocytosis: results of the Japan Langerhans Cell histiocytosis study group-02 protocol study. Int J Hematol. 2016;104(1):99–109.
https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm
Braier J, Ciocca M, Latella A, de Davila MG, Drajer M, Imventarza O. Cholestasis, sclerosing cholangitis, and liver transplantation in Langerhans cell histiocytosis. Med Pediatr Oncol. 2002;38(3):178–82.
Ziogas IA, Kakos CD, Wu WK, Montenovo MI, Matsuoka LK, Zarnegar-Lumley S, et al. Liver transplantation for langerhans cell histiocytosis: a US population-based analysis and systematic review of the literature. Liver Transpl. 2021;27(8):1181–90. https://doi.org/10.1002/lt.25995.
Newell KA, Alonso EM, Kelly SM, Rubin CM, Thistlethwaite JR Jr, Whitington PF. Association between liver transplantation for Langerhans cell histiocytosis, rejection, and development of posttransplant lymphoproliferative disease in children. J Pediatr. 1997;131:98–104.
Hadzic N, Pritchard J, Webb D, Portmann B, Heaton ND, Rela M, et al. Recurrence of Langerhans cell histiocytosis in the graft after pediatric liver transplantation. Transplantation. 2000;70(5):815–9.
Tfifha M, Kamoun T, Mama N, Mestiri S, Hassayoun S, Zouari N, et al. Childhood sclerosing cholangitis associations in a Tunisian tertiary care hospital: a many-faced disease. Turk J Pediatr. 2019;61:905–14.
Melendez HV, Dhawan A, Mieli-Vergani G, Rela M, Heaton ND, Pritchard J, et al. Liver transplantation for Langerhans’ cell histiocytosis-a case report and literature review. Transplantation. 1996;62(8):1167–71. Accessed 5 April 2022.
Murakami M, Onishi S, Ohya Y, Kawabata S, Isono K, Sugawara Y, et al. Langerhans cell histiocytosis confined to extrahepatic bile duct causing sclerosing cholangitis in child: a case report. Surg Case Rep. 2020;6(1):137. https://doi.org/10.1186/s40792-020-00899-6.
Honda R, Ohno Y, Iwasaki T, Okudaira S, Okada M, Kamitamari A, et al. Langerhans’ cell histiocytosis after living donor liver transplantation: report of a case. Liver Transpl. 2005;11(11):1435–8.
Al Salloom AA, Almalki ST, Almana H, Burdelski M. Diabetes insipidus and sclerosing cholangitis in a child may be a clue to the diagnosis of Langerhans’ cell histiocytosis: a case report. Int J Health Sci (Qassim). 2013;7(2):248–51.
Rajwal SR, Stringer MD, Davison SM, Gerrard M, Glaser A, Tanner MS, et al. Use of basiliximab in pediatric liver transplantation for Langerhans cell histiocytosis. Pediatr Transplant. 2003;7(3):247–51.
Badalian-Very G, Vergilio JA, Degar BA, MacConail LE, Brandner B, Calicchio ML, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116(11):1919–23.
Kobayashi M, Tojo A. Langerhans cell histiocytosis in adults: advances in pathophysiology and treatment. Cancer Sci. 2018;109:3707–13.
Héritier S, Emile JF, Barkaoui MA, Thomas C, Fraitag S, Boudjemaa S, et al. BRAF mutation correlates with high-risk Langerhans cell histiocytosis and increased resistance to first-line therapy. J Clin Oncol. 2016;34(25):3023–30.
Milne P, Bigley V, Bacon CM, Néel A, McGovern N, Bomken S, et al. Hematopoietic origin of Langerhans cell histiocytosis and Erdheim-Chester disease in adults. Blood. 2017;130(2):167–75.
Cui L, Zhang L, Ma HH, Wang CJ, Wang D, Lian HY, et al. Circulating cell-free BRAFV600E during chemotherapy is associated with prognosis of children with Langerhans cell histiocytosis. Haematologica. 2020;105(9):e444-447.
Schwentner R, Kolenová A, Jug G, Schnöller T, Ahlmann M, Meister B, et al. Longitudinal assessment of peripheral blood BRAFV600E levels in patients with Langerhans cell histiocytosis. Pediatr Res. 2019;85(6):856–64.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Watakabe, M., Fukuoka, K., Ihara, Y. et al. Optimal timing of liver transplantation for liver cirrhosis caused by sclerosing cholangitis in a patient with Langerhans cell histiocytosis: a case report. Int J Hematol 117, 759–764 (2023). https://doi.org/10.1007/s12185-022-03500-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03500-y