Abstract
Purpose of Review
The purpose of this review will be to provide both a historical and recent review of the role of the kinetic chain for the overhead athlete. The kinetic chain concept will then be applied to clinical exercise modifications and integrations for prevention and treatment of shoulder injury.
Recent Findings
The primary conclusion reached through this review is the important role the lower extremity, trunk, and scapular region play in the development of optimal terminal segment acceleration in the overhead throwing and serving motion. Failure of any links in the kinetic chain has implications for shoulder and elbow injury in the overhead athlete. Modifications of traditional shoulder exercises emphasizing activation of the scapular stabilizers and core musculature alongside concomitant rotator cuff activation are recommended and supported in EMG research.
Summary
Future research is needed to further identify risk factors and rehabilitation and prevention strategies and key clinical tests for the overhead athlete. The goal is to elucidate the important role the kinetic chain plays in both performance enhancement and injury prevention for the overhead athlete. Understanding the key role all segments of the kinetic chain play in the complex biomechanical segmental rotations required for high-level throwing and serving will assist clinicians who work with overhead athletes.







Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Kibler WB. Clinical biomechanics of the elbow in tennis: implications for evaluation and diagnosis. Med Sci Sports Exerc. 1994;26(10):1203–6.
Hanavan EP. A mathematical model of the human body: Wright-Patterson Air Force Base; 1964. (AMRL-TR-64–102)
Davies GJ. A compendium of isokinetics in clinical usage. LaCrosse: S & S Publishing; 1992.
Bunn J. Scientific principles of coaching. Englewood Cliffs: Prentice-Hall; 1972.
Plagenhoef S. Patterns of human movement. Englewood Cliffs: Prentice-Hall; 1971.
Marshall RN, Elliot BC. Long-axis rotation: the missing link in proximal-to-distal segmental sequencing. J Sports Sci. 2000;18:247–54.
Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implication of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit’. Br J Sports Med. 2013;47:877–85.
Sciascia A, Thigpen C, Namdari S. Kinetic chain abnormalities in the athletic shoulder. Sports Med Arthrosc Rev. 2012;20:16–21.
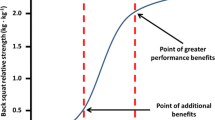
Seroyer ST, Nho SJ, Bah BR et al. The kinetic chain in overhead pitching: its potential role for performance enhancement and injury prevention.
Garrison CJ, Arnold A, Macko MJ, Conway JE. Baseball players diagnosed with ulnar collateral ligament tears demonstrate decreased balance compared to healthy controls. J Orthop Sports Phys Ther. 2013;43:752–8.
• Chalmers PN, Wimmer MA, Verma NN, Cole BJ, Romeo AA, Cvetanovich GL, et al. The relationship between pitching mechanics and injury: a review of current concepts. Sports Health. 2017;9:216–21. https://doi.org/10.1177/1941738116686545The purpose of this study was to describe the relationship between pitching mechanics and injury. The study conducted a comprehensive review of the literature available in terms of biomechanical and clinical evidence surrounding pitching motion analysis between 1983 and 2016. This study found that altered knee flexion at ball release, early trunk rotation, loss of shoulder rotational range of motion, increased elbow flexion at ball release, high pitch velocity, and increased pitcher fatigue correlated to shoulder and elbow injury. Level of Evidence: Level 5.
Robb AJ, Fleisig G, Wilk KE, et al. Passive range of motion of the hips and their relationship with pitching biomechanics and ball velocity in professional baseball pitchers. Am J Sports Med. 2010;38(12). https://doi.org/10.1177/0363546510375535.
• Chu SK, Jayabalan P, Kibler WB. The kinetic chain revisited: new concept on throwing. PM R. 2016;8:S69–77 The purpose of this article was to review the biomechanics of the overhead throwing motion, the role of the kinetic chain in throwing, and the clinical evaluation and management of abnormal throwing mechanics and related injury. Understanding the proper mechanics of the overhead throwing motion and the role of the kinetic chain in throwing is important when evaluating overhead throwing athletes. When evaluating an overhead throwing athlete, observation of overhead throwing mechanics and examination of the kinetic chain and shoulder should be performed. Level of evidence: Level 5.
• Kantrowitz DE, Trofa DP, Woode R, et al. Athletic hip injury in Major League Baseball pitchers associated with ulnar collateral ligament tear. Orthorp J Sports Med. 2018. https://doi.org/10.1177/2325967118800704The purpose of this study was to determine whether professional baseball pitchers who underwent UCL reconstruction (UCLR) had an increased incidence of hip or groin injuries 4 years before or after surgery. There were 247 subjects who are MLB players at the time of study and underwent UCLR between 2005 and 2017. As a result of this study, MLB pitchers who required UCLR sustained a higher frequency of proximal lower extremity injury both before and after surgery. Hip mobility and core strengthening may help reduce elbow injury in baseball players. Level of evidence: Cohort study, level 3.
• Culiver A, Garrison CJ, Creed KM, et al. Correlation among Y-balance test-lower quarter composite scores, hip musculoskeletal characteristics, and pitching kinematics in NCAA division I baseball pitchers. J Sports Rehabil. 2019;28:432–7 The aim of this study was to evaluate the relationship between UE and LE kinematics during the pitching motion, Y balance test-lower quarter (YBT-LQ) score, hip ROM, and hip strength. Nineteen healthy male Division I baseball pitchers were measured for their hip IR and ER ROM, hip abduction strength, and YBT-LQ scores. They found that YBT-LQ’s score had low to moderate correlation with decreased stride length which may increase the risk of shoulder and elbow injury. Level of evidence: Cross-sectional study, Level 4.
• Tocci NX, Howell DR, Sugimoto D, Dawkins C, Whited A, Bae D. The effect of stride length and lateral pelvic tilt on elbow torque in youth baseball pitchers. J Appl Biomech. 2017;33:339–46 The aim of this study was to investigate the effect of pitching mechanics on peak elbow varus torque in healthy youth pitchers. There were 18 male pitchers between the ages of 12–18 years. Participants threw 3 fastballs and 3 changeups each. Each motion was analyzed using motion analysis in order to calculate the torques about the elbow during each pitch. The result from this study indicates that greater stride length and lesser lateral pelvic tilt are associated with greater elbow torque in youth pitchers for both fastballs and changeups. Also, there is positive correlation between ball velocity and elbow torque. Level of evidence: Cross-sectional analysis, Level 4.
• Laudner KG, Wong R, Mister K. The influence of lumbopelvic control on shoulder and elbow kinetic s in elite baseball pitchers. J Should Elbow Surg. 2019;28:330–224 The purpose of this study was to determine the strength of the relationships between lumbopelvic control and upper extremity pitching kinetics in baseball pitchers. Forty-three baseball pitchers (age, 20.1 ± 2.3 years) participated in this study. All participants were asymptomatic and had no any recent upper or lower extremity injury (within 3 months) or any history of surgery. Participants were measured for lumbopelvic control and pitching kinetics to test the relationship between lumbopelvic control and upper extremity pitching kinematics. This study showed that a relationship exists between lumbopelvic control of the drive leg and both shoulder horizontal torque and elbow valgus torque during the throwing motion. Leve of evidence: Basic Science study, level 5.
• Myrick KM, Pallone AS, Feinn RS. Trunk muscle endurance, flexibility, stride foot balance, and contralateral trunk lean in collegiate baseball pitchers. J Strength Cond Res. 2019;33(10):2641–7 The aim of this study was to examine the correlation between trunk muscle endurance and flexibility, and stride foot balance with contralateral lean during pitching. Ten male Division I collegiate baseball pitchers between the ages of 18 and 21 were recruited for participation in this study. There was no significant relationship identified between trunk muscle endurance and flexibility, and stride foot balance with contralateral lean. Level of evidence: Level 4.
Kibler WB, Chandler J. Baseball and tennis. In: Griffin LY, editor. Rehabilitation of the injured knee. St. Louism MO: Mosby; 1995. p. 219–26.
Groppel JL. High tech tennis. 2nd ed. Champaign: Human Kinetics; 1992.
Van Gheluwe B, Hebbelinck M. Muscle actions and ground reaction forces in tennis. Int J Sport Biomech. 1986;2:88–99.
Elliott BC, Marshall RN, Noffal GJ. Contributions of upper limb segment rotations during the power serve in tennis. J Appl Biomech. 1995;11:433–42.
Elliott B, Fleisig GS, Nicholls R, Escamilla R. Technique effects on upper limb loading in the tennis serve. J Sci Med Sport. 2003;6(1):76–87.
Kovacs M, Ellenbecker TS. An 8-stage model for evaluating the tennis serve: implications for performance enhancement and injury prevention. Sports Health. 2011;3(6):504–13.
Davies GJ, Ellenbecker TS. Scientific and clinical rationale for utilization of a total arm strength rehabilitation program for shoulder and elbow overuse injuries. LaCrosse: APTA Orthopaedic Section, Home Study Course; 1993.
Ellenbecker TS, Davies GJ. Closed kinetic chain exercise. A comprehensive guide to multiple joint exercises. Champaign: Human Kinetics Publishers; 2001.
Priest JD, Nagel DA. Tennis shoulder. Am J Sports Med. 1976;4(1):28–42.
Priest JD, Braden V, Gerberich SG. The elbow and tennis, part 1: an analysis of players with and without pain. Phys Sportsmed. 1980;8(4):80–91.
Strizak AM, Gleim GW, Sapega A, Nicholas JA. Hand and forearm strength and its relation to tennis. Am J Sports Med. 1983;11(4):234–9. https://doi.org/10.1177/036354658301100410.
Alizadehkhaiyat O, Fisher AC, Kemp GJ, Vishwanathan K, Frostick SP. Upper limb muscle imbalance in tennis elbow: a functional and electromyographic assessment. J Orthop Res. 2007;25(12):1651–7. https://doi.org/10.1002/jor.20458.
Lucado AM, Kolber KJ, Cheng MS, Echternach JL. Upper extremity strength characteristics in female recreational tennis players with and without lateral epicondylalgia. J Orthop Sports Phys Ther. 2012;42(12):1025–31. https://doi.org/10.2519/jospt.2012.4095.
Day JM, Bush H, Nitz AJ, UHL TL. Scapular muscle performance in individuals with lateral epicondylalgia. J Orthop Sports Phy Ther. 2015;45(5):414–24.
Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325–37.
Kibler WB, Uhl TL, Maddux JW, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elb Surg. 2002;11:550–6.
• Plummer HA, Sum JC, Pozzi F, Varghese R, Michener LA. Observational scapular dyskinesis: known-group validity in patients with and without shoulder pain. J Orthop Sports Phys Ther. 2017;47(8):530–7. https://doi.org/10.2519/jospt.2017.7268The aim of this study was to characterize the prevalence of scapular dyskinesis in participants with shoulder pain as compared with a matched control group without shoulder pain on prevalence of scapular dyskinesis. The scapular dyskinesis test (SDT) was performed to participants (n= 135), 67 with shoulder pain and 68 healthy controls in this study. There were no significant differences for scapular dyskinesis prevalence between the shoulder pain group and the control group. As a result of this study, the scapular dyskinesis assessed with the SDT is not more prevalent in those with shoulder pain. Scapular dyskinesis may represent normal movement variability. Level of evidence: Cross-sectional analysis, Level 4.
• Hickey D, Solvig V, Cavalheri V, Harrold M, Mckenna L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis. Br J Sports Med. 2018;52(2):102–10. https://doi.org/10.1136/bjsports-2017-097559The purpose of this study was to determine whether the presence of scapular dyskinesis in asymptomatic athletes increases the risk of developing shoulder pain by systematic review and meta-analysis. Five studies were included with a total of 419 athletes. They found 35% of athletes who have scapular dyskinesis presented with shoulder pain, which is more frequent than athletes who have shoulder pain without scapular dyskinesis. Athletes with scapular dyskinesis have the greater risk of developing shoulder pain than those without scapular dyskinesis. Level of evidence: Systemic Review, Meta-Analysis; Level 1.
Rabin A, Irrgang JJ, Fitzgerald KG, Eubanks A. The intertester reliability of the scapular assistance test. J Orthop Sports Phys Ther. 2006;36(9):653–60.
• Kibler WB, Sciascia AD. Disorders of the Scapula and their role in shoulder injury. Springer 2017. Level of evidence: Book, Author opinion; Level 5.
United States Tennis Association High Performance Profile. www.usta.com
Ellenbecker TS, Windler G, Dines D, Renstrom P. Musculoskeletal profile of tennis players on the ATP World Tour: results of a 9 year screening program. J Med Sci Tennis. 20(3):94–106.
Ellenbecker TS. Musculoskeletal testing of elite junior tennis players. Aspetar Sports Med J. 2014:548–56.
• Rice RP, Roach KE, Waltz B, Kirk-Sanchez NJ, Ellenbecker TS, Raya M. Side to side asymmetries of the hip and core are associated with back injuries in elite and professional tennis players. J Orthop Sports Phys Ther. 2018;48(1):A-57 The purpose of this study was to investigate the relationship between trunk and lower quarter screening tests and musculoskeletal injuries. The results of this study are consistent with previous research. Adolescent athletes and tennis players may be at increased risk of injuries due to risk factors including mobility, stability, and flexibility deficits. Level of evidence: cross-sectional analysis; Level 4.
Ellenbecker TS, Ellenbecker GA, et al. Descriptive profile of hip rotation range of motion in elite tennis players and professional baseball pitchers. Am J Sports Med. 2007;35(8):1371–6. https://doi.org/10.1177/0363546507300260.
• Cheatham SW, Shimamura, Kolber MJ. Difference in hip range of motion among collegiate pitchers when compared to youth and professional baseball pitcher data. J Can Chiropr Assoc. 2016;60(3):233–40 The purpose of this study was to measure passive hip internal (IR) and external rotation (ER) range of motion (ROM) in collegiate baseball pitchers and compare with published youth and professional values. Measures were taken on the bilateral hips of 29 participants (mean age 20.0 ± 1.4, range 18–22 years). Results identified no significant differences between the stance and stride hip in collegiate right-handed pitchers for IR (p= 0.22, ES 0.23) and ER (p= .08, ES = 0.25). There was no significant difference in left-handed pitchers for IR (p= 0.80, ES = 0.11) and ER (p= 0.56, ES = 0.15). When comparing youth with collegiate, IR increased in the stance (2°) and stride (5°) hip, and an increase in the stance (5°) and stride (5°) hip were present for ER as well. From collegiate to professional, IR increased in the stance (4°) and stride (3°) hip whereas a decrease in the stance (9°) and stride (12°) hip was present for ER. The data suggests an increase in passive ROM from youth to collegiate and a decrease from collegiate to professional level. Level of evidence: cross-sectional study; Level 4.
• Oliver GD, Weimar WH. Hip and shoulder range of motion in youth baseball pitchers. J Strength Cond Res. 2016;30(10):2823–7. https://doi.org/10.1519/JSC.0000000000000796The purpose of this study was to measure and evaluate bilateral hip and throwing shoulder rotation PROM in youth baseball pitchers, to determine if there is any correlation between the throwing shoulder and stance hip rotation PROM. Twenty-six youth baseball pitchers were recruited and measured for bilateral hip and shoulder PROM. The youth baseball pitchers in this study displayed similar PROM patterns as collegiate and professional baseball pitchers. Youth baseball pitchers in this study presented strong relationships between hip and shoulder PROM. Level of evidence: case-controlled study; Level 3.
McCulloch PC, Patel JK, Ramkumar PN. Asymmetric hip rotation in professional baseball pitchers. Orthop J Sports Med. 2014;2(2). https://doi.org/10.1177/2325967114521575.
Wilk KE, Yenchak AJ, et al. The advanced throwers ten exercise program: a new exercise series for enhanced dynamic shoulder control in the overhead throwing athlete. Phys Sports Med. 2011;39(2). https://doi.org/10.3810/psm.2011.11.1943.
Myers NL, Toonstra JL, Smith JS, et al. Sustained isometric shoulder contraction on muscular strength and endurance: a randomized clinical trial. Int J Sports Phys Ther. 2015;10(7):1015–25.
DeMay K, Danneels L, Cagnie B, et al. Kinetic chain influences on upper and lower trapezius muscle activation during eight variations of a scapular retraction exercises in overhead athletes. J Sci Med Sport. 2013;16:65–70.
DeMay K, Danneels L, Cagnie B, et al. Conscious correction of scapular orientation in overhead athletes performing selected shoulder rehabilitation exercises: the effect on trapezius muscle activation measured by surface electromyography. J Orthop Sports Phys Ther. 2013;43(1):3–10.
• Staker JL, Evans AJ, Jacobs LE, et al. The effect of tactile and verbal guidance during scapulothoracic exercises: an EMG and kinematic investigation. J Electromyogr Kinesiol. 2019. https://doi.org/10.1016/j.jelekin.2019.07.004The purpose of this study was to determine if clinician guidance changes scapulothoracic muscle activity and kinematics compared with unguided shoulder exercises with electromyographic (EMG) sensors placed on serratus anterior, upper, and lower trapezius. The study found that verbal and tactile guidance during exercises significantly increases shoulder muscle activity and improves lower trapezius/upper trapezius muscle recruitment. Level of evidence: case-controlled study; Level 3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Todd S. Ellenbecker & Ryoki Aoki declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Injuries in Overhead Athletes
Rights and permissions
About this article
Cite this article
Ellenbecker, T.S., Aoki, R. Step by Step Guide to Understanding the Kinetic Chain Concept in the Overhead Athlete. Curr Rev Musculoskelet Med 13, 155–163 (2020). https://doi.org/10.1007/s12178-020-09615-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-020-09615-1