Abstract
Background
Non-alcoholic steatohepatitis (NASH) is a progression of non-alcoholic fatty liver disease. The increasing burden of NASH has become a major concern of public health in greater China. This study aimed to characterize the epidemiology, disease burden, and treatment of NASH in greater China to better inform national disease management and delivery of health services.
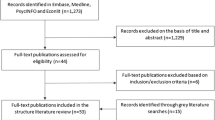
Methods
We conducted a systematic review searching four English databases (Web of Science, PubMed, Medline, and Cochrane Central) and three Chinese databases (CNKI, Wanfang, and VIP). We identified articles published from database inception to October 10, 2020 which reported NASH epidemiology, disease burden, and/or intervention in Chinese adults.
Results
Of 44,115 articles retrieved, 33 were eligible for inclusion. Overall prevalence of NASH ranged from 2.4 to 6.1% in greater China, with a more substantial burden among males, the aged, and those in Hong Kong and Taiwan. Most NASH patients suffered from several comorbidities, including obesity, diabetes, and cardiovascular conditions. PNPLA3 rs738409 G allele and haptoglobin 2–2 genotype drove the fibrosis progression in NASH. Increasingly prevalent cases of cirrhosis and hepatocellular carcinoma caused a higher NASH-related mortality. Compared with normal population, NASH patients experienced markedly poorer quality of life and heavier costs.
Conclusion
This is the first comprehensive overview of NASH among Chinese population that revealed an overwhelming impact of social and healthcare burden associated with the condition. Further high-quality studies are needed to improve the understanding and management of NASH in greater China.


Similar content being viewed by others
Abbreviations
- CHB:
-
Chronic hepatitis B
- CVD:
-
Cardiovascular disease
- GD:
-
Gallbladder disease
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- Hp:
-
Haptoglobin
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- PROs:
-
Patient-reported outcomes
- QoL:
-
Quality of life
- T2DM:
-
Type 2 diabetes mellitus
References
Argo CK, Northup PG, Al-Osaimi AM, Caldwell SH. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J Hepatol 2009;51(2):371–379
Perumpail BJ, Khan MA, Yoo ER, Cholankeril G, Kim D, Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol 2017;23(47):8263–8276
Ekstedt M, Nasr P, Kechagias S. Natural History of NAFLD/NASH. Curr Hepatol Rep 2017;16(4):391–397
Corte CD, Ferrari F, Villani A, Nobili V. Epidemiology and Natural History of NAFLD. J Med Biochem 2015;34(1):13–17
Zhou F, Zhou J, Wang W, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: a systematic review and meta-analysis. Hepatology 2019;70(4):1119–1133
Povsic M, Wong OY, Perry R, Bottomley J. A structured literature review of the epidemiology and disease burden of non-alcoholic steatohepatitis (NASH). Adv Ther 2019;36(7):1574–1594
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151(4):264–269
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25(9):603–605
Higgins JP, Altman DG, Gotzsche PC, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928
Moons KGM, Wolff RF, Riley RD, et al. PROBAST: a tool to assess risk of bias and applicability of prediction model studies: explanation and elaboration. Ann Intern Med 2019;170(1):W1-w33
Zeng X, Zhang Y, Kwong JS, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 2015;8(1):2–10
Wang D, Wang L, Wang Z, Chen S, Ni Y, Jiang D. Higher non-HDL-cholesterol to HDL-cholesterol ratio linked with increased nonalcoholic steatohepatitis. Lipids Health Dis 2018;17(1):67
Tampi RP, Wong VW, Wong GL, et al. Modelling the economic and clinical burden of non-alcoholic steatohepatitis in East Asia: data from Hong Kong. Hepatol Res 2020;50(9):1024–1031
Estes C, Chan HLY, Chien RN, et al. Modelling NAFLD disease burden in four Asian regions-2019-2030. Aliment Pharmacol Ther 2020;51(8):801–811
Estes C, Anstee QM, Arias-Loste MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J Hepatol 2018;69(4):896–904
Xun YH, Fan JG, Zang GQ, et al. Suboptimal performance of simple noninvasive tests for advanced fibrosis in Chinese patients with nonalcoholic fatty liver disease. J Dig Dis 2012;13(11):588–595
Yu C, Xu C, Xu L, Yu J, Miao M, Li Y. Serum proteomic analysis revealed diagnostic value of hemoglobin for nonalcoholic fatty liver disease. J Hepatol 2012;56(1):241–247
Xia MF, Bian H, Zhu XP, et al. Serum folic acid levels are associated with the presence and severity of liver steatosis in Chinese adults. Clin Nutr 2018;37(5):1752–1758
Qiao ZP, Zheng KI, Zhu PW, et al. Lower levels of plasma NT-proBNP are associated with higher prevalence of NASH in patients with biopsy-proven NAFLD. Nutr Metab Cardiovasc Dis 2020;30(10):1820–1825
Pang J, Xu W, Zhang X, et al. Significant positive association of endotoxemia with histological severity in 237 patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther 2017;46(2):175–182
Bian H, Zhu X, Xia M, et al. Impact of type 2 diabetes on nonalcoholic steatohepatitis and advanced fibrosis in patients with nonalcoholic fatty liver disease. Endocr Pract 2020;26(4):444–453
Zhou J, Liu J, Sheng H, et al. Haptoglobin 2–2 genotype is associated with more advanced disease in subjects with non-alcoholic steatohepatitis: a retrospective study. Adv Ther 2019;36(4):880–895
Tai CM, Huang CK, Tu HP, Hwang JC, Chang CY, Yu ML. PNPLA3 genotype increases susceptibility of nonalcoholic steatohepatitis among obese patients with nonalcoholic fatty liver disease. Surg Obes Relat Dis 2015;11(4):888–894
Liew PL, Lee WJ, Lee YC, Wang HH, Wang W, Lin YC. Hepatic histopathology of morbid obesity: concurrence of other forms of chronic liver disease. Obes Surg 2006;16(12):1584–1593
Tai CM, Huang CK, Tu HP, et al. Interactions of a PPARGC1A variant and a PNPLA3 variant affect nonalcoholic steatohepatitis in severely obese taiwanese patients. Medicine (Baltimore) 2016;95(12):e3120
Liew PL, Lee WJ, Wang W, et al. Fatty liver disease: predictors of nonalcoholic steatohepatitis and gallbladder disease in morbid obesity. Obes Surg 2008;18(7):847–853
Tan CH, Al-Kalifah N, Ser KH, Lee YC, Chen JC, Lee WJ. Long-term effect of bariatric surgery on resolution of nonalcoholic steatohepatitis (NASH): an external validation and application of a clinical NASH score. Surg Obes Relat Dis 2018;14(10):1600–1606
Tan CH, Al-Kalifah N, Lee WJ, Ser KH, Lee YC, Chen JC. HSCRP as surrogate marker in predicting long term effect of bariatric surgery on resolution of non-alcoholic steatohepatitis. Asian J Surg 2019;42(1):203–208
Wang Q, You H, Ou X, et al. Non-obese histologically confirmed NASH patients with abnormal liver biochemistry have more advanced fibrosis. Hepatol Int 2019;13(6):766–776
Zain SM, Mohamed R, Mahadeva S, et al. A multi-ethnic study of a PNPLA3 gene variant and its association with disease severity in non-alcoholic fatty liver disease. Hum Genet 2012;131(7):1145–1152
Liu L, Li P, Mi Y, Liu Y, Liu Y, Zhang P. Thyroid-stimulating hormone is associated with nonalcoholic steatohepatitis in patients with chronic hepatitis B. Medicine (Baltimore) 2019;98(46):e17945
Du T, Sun X, Yuan G, et al. Sex differences in the impact of nonalcoholic fatty liver disease on cardiovascular risk factors. Nutr Metab Cardiovasc Dis 2017;27(1):63–69
Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 2018;15(1):11–20
Centers for Disease Control and Prevention. Progress in hepatitis B prevention through universal infant vaccination–China, 1997–2006. Morb Mortal Wkly Rep 2007;56(18):441–445
Liu L, Li P, Mi YQ, Liu YG, Liu YQ, Zhang P. Thyroid-stimulating hormone is associated with nonalcoholic steatohepatitis in patients with chronic hepatitis B. Medicine 2019. https://doi.org/10.1097/MD.0000000000017945
Xiong J, Wang J, Huang J, Sun W, Wang J, Chen DF. Non-alcoholic steatohepatitis-related liver cirrhosis is increasing in China: a ten-year retrospective study. Clinics 2015;70(8):563–568
He YF, Yang G. On the death due to nonalcoholic fatty liver disease in Lanshi community of Foshan City. JCM 2013;11(06):4–6
Younossi ZM, Stepanova M, Lawitz EJ, et al. Patients with nonalcoholic steatohepatitis experience severe impairment of health-related quality of life. Am J Gastroenterol 2019;114(10):1636–1641
Younossi ZM, Stepanova M, Anstee QM, et al. Reduced patient-reported outcome scores associate with level of fibrosis in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol 2019;17(12):2552–2560
Chitturi S, Wong VW, Chan WK, et al. The asia-pacific working party on non-alcoholic fatty liver disease guidelines 2017-part 2: management and special groups. J Gastroenterol Hepatol 2018;33(1):86–98
Yen FS, Yang YC, Hwu CM, et al. Liver-related long-term outcomes of thiazolidinedione use in persons with type 2 diabetes. Liver Int 2020;40(5):1089–1097
Harrison SA, Wong VW, Okanoue T, et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: results from randomized phase III STELLAR trials. J Hepatol 2020;73(1):26–39
European Association for the Study of the L, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64(6):1388–1402
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American association for the study of liver diseases. Hepatology 2018;67(1):328–357
Gao X, Fan JG, Study Group of L, Metabolism CSoE. Diagnosis and management of non-alcoholic fatty liver disease and related metabolic disorders: consensus statement from the study group of liver and metabolism, Chinese society of endocrinology. J Diabetes 2013;5(4):406–415
Lall CG, Aisen AM, Bansal N, Sandrasegaran K. Nonalcoholic fatty liver disease. Am J Roentgenol 2008;190(4):993–1002
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64(1):73–84
Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol 2015;13(4):643–654
Younossi ZM, Tampi R, Priyadarshini M, Nader F, Younossi IM, Racila A. Burden of illness and economic model for patients with nonalcoholic steatohepatitis in the United States. Hepatology 2019;69(2):564–572
Review T, LaBrecque DR, Abbas Z, et al. World gastroenterology organisation global guidelines: nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. J Clin Gastroenterol 2014;48(6):467–473
Filozof C, Goldstein BJ, Williams RN, Sanyal A. Non-alcoholic steatohepatitis: limited available treatment options but promising drugs in development and recent progress towards a regulatory approval pathway. Drugs 2015;75(12):1373–1392
Younossi ZM. Review article: current management of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis. Aliment Pharmacol Ther 2008;28(1):2–12
Sayiner M, Koenig A, Henry L, Younossi ZM. Epidemiology of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis in the United States and the rest of the world. Clin Liver Dis 2016;20(2):205–214
Phisalprapa P, Supakankunti S, Charatcharoenwitthaya P, et al. Cost-effectiveness analysis of ultrasonography screening for nonalcoholic fatty liver disease in metabolic syndrome patients. Medicine (Baltimore) 2017;96(17):e6585
Hashimoto E, Tokushige K. Prevalence, gender, ethnic variations, and prognosis of NASH. J Gastroenterol 2011;46(Suppl 1):63–69
Leung CM, Lai LS, Wong WH, et al. Non-alcoholic fatty liver disease: an expanding problem with low levels of awareness in Hong Kong. J Gastroenterol Hepatol 2009;24(11):1786–1790
Xu R, Tao A, Zhang S, Deng Y, Chen G. Association between patatin-like phospholipase domain containing 3 gene (PNPLA3) polymorphisms and nonalcoholic fatty liver disease: a HuGE review and meta-analysis. Sci Rep 2015;5:9284
Seko Y, Sumida Y, Tanaka S, et al. Development of hepatocellular carcinoma in Japanese patients with biopsy-proven non-alcoholic fatty liver disease: association between PNPLA3 genotype and hepatocarcinogenesis/fibrosis progression. Hepatol Res 2017;47(11):1083–1092
Koo BK, Joo SK, Kim D, et al. Additive effects of PNPLA3 and TM6SF2 on the histological severity of non-alcoholic fatty liver disease. J Gastroenterol Hepatol 2018;33(6):1277–1285
Kozlitina J, Smagris E, Stender S, et al. Exome-wide association study identifies a TM6SF2 variant that confers susceptibility to nonalcoholic fatty liver disease. Nat Genet 2014;46(4):352–356
Liu YL, Reeves HL, Burt AD, et al. TM6SF2 rs58542926 influences hepatic fibrosis progression in patients with non-alcoholic fatty liver disease. Nat Commun 2014;5:4309
Dongiovanni P, Petta S, Maglio C, et al. Transmembrane 6 superfamily member 2 gene variant disentangles nonalcoholic steatohepatitis from cardiovascular disease. Hepatology 2015;61(2):506–514
Sookoian S, Castano GO, Scian R, et al. Genetic variation in transmembrane 6 superfamily member 2 and the risk of nonalcoholic fatty liver disease and histological disease severity. Hepatology 2015;61(2):515–525
Eguchi Y, Wong G, Lee EI, Akhtar O, Lopes R, Sumida Y. Epidemiology of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in Japan: a focused literature review. JGH Open 2020;4(5):808–817
Sanyal AJ, Martin AL, Cadarette SM, et al. A systematic literature review of the epidemiology and economic burden associated with non-alcoholic steatohepatitis. J Hepatol 2016;64:S475
Okanoue T, Umemura A, Yasui K, Itoh Y. Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis in Japan. J Gastroen Hepatol 2011;26:153–162
Sporea I, Jurchis A, Sirli R, Bota S, Sendroiu M. Can transient elastography be a reliable method for assessing liver fibrosis in non alcoholic steatohepatitis (NASH)? Med Ultrason 2013;15(2):106–110
Fan JG, Wei L, Zhuang H, National Workshop on Fatty L, Alcoholic Liver Disease CSoHCMA, Fatty Liver Disease Expert Committee CMDA. Guidelines of prevention and treatment of nonalcoholic fatty liver disease (2018, China). J Dig Dis 2019;20(4):163–173
Yu Y, Cai JJ, She ZG, Li HL. Insights into the epidemiology, pathogenesis, and therapeutics of nonalcoholic fatty liver diseases. Adv Sci 2019 https://doi.org/10.1002/advs.201801585
Funding
Not available.
Author information
Authors and Affiliations
Contributions
HZ, YG, QL, CU, and HH conceived the research project, coordinated the contributors, and revised drafts of the manuscript. HZ, YG, and QL participated in the study selection and data extraction. YG and QL revised drafts of the manuscript and contributed to data analysis. HZ developed the search strategy, searched the databases, and contributed to the revision of the manuscript. ZR, YL and DY served as scientific advisors.
Corresponding author
Ethics declarations
Conflict of interest
Huimin Zou, Ying Ge, Qing Lei, Carolina Oi Lam Ung, Zhen Ruan, Yunfeng Lai, Dongning Yao, Hao Hu declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zou, H., Ge, Y., Lei, Q. et al. Epidemiology and disease burden of non-alcoholic steatohepatitis in greater China: a systematic review. Hepatol Int 16, 27–37 (2022). https://doi.org/10.1007/s12072-021-10286-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10286-4