Abstract
Background
Current guidelines have limited consensus on the approach to portal venous thrombosis (PVT) in cirrhotic patients. While there is rising interest in direct oral anticoagulants (DOACs) use for PVT, current evidence is limited by small sample size and lack of comparisons to traditional anticoagulants. Thus, a network meta-analysis was conducted to compare the use of DOACs with traditional anticoagulants.
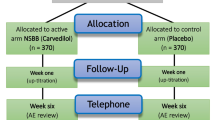
Methods
Medline and Embase were searched for articles about anticoagulation use in cirrhotic patients with nontumorous PVT for articles on DOACs, warfarin, low-molecular weight heparin (LMWH) or antithrombin III. A network analysis was conducted using risk ratios (RR) with surface under the cumulative ranking curve (SUCRA). A single-arm meta-analysis was used to summarize the outcomes of DOAC treatment.
Results
A total of 10 articles were included in the study. 79.5% (CI 38.8–95.9) of DOACs patients achieved complete or partial recanalization and 9.80% (CI 4.50–20.0) experienced a bleeding event. DOACs were superior to LMWH (RR 2.299, CI 1.037–5.093, p = 0.040), warfarin (RR 1.762, CI 1.017–3.053, p = 0.043) and no treatment (RR 3.489, CI 1.394–8.733, p = 0.008) in complete recanalization. For partial recanalization, while DOACs were not superior to any treatment, they had the highest probability in achieving partial recanalization in SUCRA analysis. Bleeding risk and mortality were similar compared to other treatments.
Conclusion
The network analysis supports the use of DOACs in cirrhotic patients, with significant rates of complete recanalization compared to other treatments without increasing bleeding risk. DOACs can potentially be considered for nontumorous PVT in cirrhosis.





Similar content being viewed by others
Data availability
All data are available from Medline and Embase databases.
Abbreviations
- DOACs:
-
Direct oral anticoagulants
- PVT:
-
Portal vein thrombosis
- LMWH:
-
Low-molecular weight heparin
- CRNMB:
-
Clinically relevant non-major bleeding
- RR:
-
Risk Ratio
- SUCRA:
-
Surface under the cumulative ranking curve
- JBI:
-
Joanna Briggs Institute
References
Tsochatzis EA, Senzolo M, Germani G, Gatt A, Burroughs AK. Systematic review: portal vein thrombosis in cirrhosis. Aliment Pharmacol Ther 2010;31(3):366–374
Northup PG, Garcia-Pagan JC, Garcia-Tsao G, et al. Vascular liver disorders, portal vein thrombosis, and procedural bleeding in patients with liver disease: 2020 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2020. https://doi.org/10.1002/hep.31646
Søgaard KK, Horváth-Puhó E, Grønbaek H, Jepsen P, Vilstrup H, Sørensen HT. Risk of venous thromboembolism in patients with liver disease: a nationwide population-based case-control study. Am J Gastroenterol 2009;104(1):96–101
Tripodi A, Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med 2011;365(2):147–156
Muciño-Bermejo J, Carrillo-Esper R, Uribe M, Méndez-Sánchez N. Coagulation abnormalities in the cirrhotic patient. Ann Hepatol 2013;12(5):713–724
Hirsh J, Fuster V, Ansell J, Halperin JL. American Heart Association/American College of Cardiology foundation guide to Warfarin therapy. Circulation 2003;107(12):1692–1711
Sevestre MA, Belizna C, Durant C, et al. Compliance with recommendations of clinical practice in the management of venous thromboembolism in cancer: the CARMEN study. J Mal Vasc 2014;39(3):161–168
Marchocki Z, Norris L, Toole S, Gleeson N, Saadeh FA. Patients’ experience and compliance with extended low molecular weight heparin prophylaxis post-surgery for gynecological cancer: a prospective observational study. Int J Gynecol Cancer 2019. https://doi.org/10.1136/ijgc-2019-000284
Yeh Calvin H, Hogg K, Weitz JI. Overview of the new oral anticoagulants. Arterioscler Thromb Vasc Biol 2015;35(5):1056–1065
Mulder FI, Bosch FTM, Young AM, et al. Direct oral anticoagulants for cancer-associated venous thromboembolism: a systematic review and meta-analysis. Blood 2020;136(12):1433–1441
López-López JA, Sterne JAC, Thom HHZ, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ 2017;359:j5058
Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016;149(2):315–352
Priyanka P, Kupec JT, Krafft M, Shah NA, Reynolds GJ. Newer oral anticoagulants in the treatment of acute portal vein thrombosis in patients with and without cirrhosis. Int J Hepatol 2018;2018:8432781
Weinberg EM, Palecki J, Reddy KR. Direct-acting oral anticoagulants (DOACs) in cirrhosis and cirrhosis-associated portal vein thrombosis. Semin Liver Dis 2019;39(2):195–208
Scaglione F. New oral anticoagulants: comparative pharmacology with vitamin K antagonists. Clin Pharmacokinet 2013;52(2):69–82
Nagaoki YA, Hiroshi A, Daijyo K, Teraoka Y, Shinohara F, Nakamura Y, Hatooka M, Morio K, Nakahara T, Kawaoka T, Tsuge M, Hiramatsu A, Imamura M, Kawakami Y, Ochi H, Chayama K. Efficacy and safety of edoxaban for treatment of portal vein thrombosis following danaparoid sodium in patients with liver cirrhosis. Hepatol Res 2018;48(1):51–58
Hanafy ASA-E, Sherief A-E, Dawoud MM. Randomized controlled trial of rivaroxaban versus warfarin in the management of acute non-neoplastic portal vein thrombosis. Vasc Pharmacol 2019;113:86–91
Ai MHD, Wei G, Tan XP, Xu L, Xu C, Zhang Q, Zhang Y, Li J. Efficacy and safety study of direct-acting oral anticoagulants for the treatment of chronic portal vein thrombosis in patients with liver cirrhosis. Eur J Gastroenterol Hepatol 2020;32:1395–1400
Naymagon LT, Douglas T, Zubizarreta N, Moshier E, Mascarenhas J, Schiano T. Safety, efficacy, and long-term outcomes of anticoagulation in cirrhotic portal vein thrombosis. Dig Dis Sci 2020. https://doi.org/10.1007/s10620-020-06695-4
Qi X, De Stefano V, Li H, Dai J, Guo X, Fan D. Anticoagulation for the treatment of portal vein thrombosis in liver cirrhosis: a systematic review and meta-analysis of observational studies. Eur J Intern Med 2015;26(1):23–29
Loffredo L, Pastori D, Farcomeni A, Violi F. Effects of anticoagulants in patients with cirrhosis and portal vein thrombosis: a systematic review and meta-analysis. Gastroenterology 2017;153(2):480-487.e481
Mohan BP, Aravamudan VM, Khan SR, Ponnada S, Asokkumar R, Adler DG. Treatment response and bleeding events associated with anticoagulant therapy of portal vein thrombosis in cirrhotic patients: systematic review and meta-analysis. Ann Gastroenterol 2020;33(5):521–527
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6(7):e1000097–e1000097
Zuily S, Cohen H, Isenberg D, et al. Use of direct oral anticoagulants in patients with thrombotic antiphospholipid syndrome: Guidance from the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost 2020;18(9):2126–2137
Hopewell S, McDonald S, Clarke MJ, Egger M. Grey literature in meta-analyses of randomized trials of health care interventions. Cochrane Database Systematic Rev 2007. https://doi.org/10.1002/14651858.MR000010.pub3
McKenzie JE, Brennan SE, Ryan RE, Thomson HJ, Johnston RV, Thomas J. Defining the Criteria for Including Studies and how they will be Grouped for the Synthesis. In Cochrane Handbook for Systematic Reviews of Interventions. New Jersey: Wiley; 2019. p 33–65
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14(1):135
Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005;3(4):692–694
Kaatz S, Ahmad D, Spyropoulos AC, Schulman S, Anticoagulation tSoCo. Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost 2015;13(11):2119–2126
White IR. Network meta-analysis. Stand Genom Sci 2015;15(4):951–985
White IR, Barrett JK, Jackson D, Higgins JPT. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods 2012;3(2):111–125
Tonin FS, Rotta I, Mendes AM, Pontarolo R. Network meta-analysis: a technique to gather evidence from direct and indirect comparisons. Pharm Pract (Granada) 2017;15(1):943–943
Shim SA-O, Yoon BA-O, Shin IA-O, Bae JA-O. Network meta-analysis: application and practice using Stata. Epidemiol Health 2017;39: e2017047 (2092-7193 (Electronic))
Salanti G, Ades AE, Ioannidis JPA, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 2011;64:163–171 (1878-5921 (Electronic))
Schwarzer G, Chemaitelly H, Abu-Raddad LJ, Rücker G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods 2019;10(3):476–483
Northup PG, Garcia-Pagan JC, Garcia-Tsao G, et al. Vascular liver disorders, portal vein thrombosis, and procedural bleeding in patients with liver disease: 2020 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2020;73:366–413
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898
Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag 2014;3(3):123–128
Zhou TS, Xin S, Zhou T, Li Y, Chen X, Cheng B, Gao Y. Efficacy and safety of nadroparin calcium-warfarin sequential anticoagulation in portal vein thrombosis in cirrhotic patients: a randomized controlled trial. Clin Transl Gastroenterol 2020;11(9): e00228
Hidaka HK, Shigehiro K, Sato T, Katsushima S, Izumi N, Igura T, Asahara S, Notsumata K, Osaki Y, Tsuji K, Kawanaka H, Akahoshi T, Hirota S, Matsutani S. Antithrombin III for portal vein thrombosis in patients with liver disease: a randomized, double-blind, controlled trial. Hepatol Res 2018;48(3):E107–E116
Bergère ME-P, Domitille E-P, Boillot O, Valette PJ, Guillaud O, Chambon-Augoyard C, Dumortier J. Portal vein thrombosis and liver cirrhosis: Long-term anticoagulation is effective and safe. Clin Res Hepatol Gastroenterol 2019;43(4):395–402
Chung JWK, Gi H, Lee JH, Ok KS, Jang ES, Jeong SH, Kim JW. Safety, efficacy, and response predictors of anticoagulation for the treatment of nonmalignant portal-vein thrombosis in patients with cirrhosis: a propensity score matching analysis. Clin Mol Hepatol 2014;20(4):384–391
Caracciolo GG, Garcovich M, Zocco MA, Ainora ME, Roccarina D, Annicchiarico BE, Ponziani FR, Siciliano M, Gasbarrini A. Clinical outcome of partial portal vein thrombosis in cirrhotic patients: To observe or to treat? Digest Liver Dis 2013;45:S171
Walker CA, Martens J, Laryea M, Ramaraju GA, Levstik MA, Melaragno J. Evaluation of the efficacy of apixaban use for the treatment of portal vein thrombosis in patients with cirrhosis. Hepatology 2019;70:265A
Almarshad F, Alaklabi A, Bakhsh E, Pathan A, Almegren M. Use of direct oral anticoagulants in daily practice. Am J Blood Res 2018;8(4):57–72
Chen A, Stecker E, Bruce AW. Direct oral anticoagulant use: a practical guide to common clinical challenges. J Am Heart Assoc 2020;9(13): e017559
Burnett AE, Mahan CE, Vazquez SR, Oertel LB, Garcia DA, Ansell J. Guidance for the practical management of the direct oral anticoagulants (DOACs) in VTE treatment. J Thromb Thrombolysis 2016;41(1):206–232
Mort JF, Davis JPE, Mahoro G, Stotts MJ, Intagliata NM, Northup PG. Rates of bleeding and discontinuation of direct oral anticoagulants in patients with decompensated cirrhosis. Clin Gastroenterol Hepatol 2021;19(7):1436–1442
Senzolo M, Garcia-Tsao G, García-Pagán JC. Current knowledge and management of portal vein thrombosis in cirrhosis. J Hepatol 2021;75(2):442–453
Ballestri S, Capitelli M, Fontana MC, et al. Direct oral anticoagulants in patients with liver disease in the era of non-alcoholic fatty liver disease global epidemic: a narrative review. Adv Ther 2020;37(5):1910–1932
Hernández RZ, Dalmau LMR, Aguilar MC, et al. Cost-effectiveness of direct oral anticoagulants versus vitamin K antagonist in atrial fibrillation: a study protocol using Real-World Data from Catalonia (FantasTIC Study). Medicine 2020;99(36): e22054
Walter E, Voit M, Eichhober G. Cost-effectiveness analysis of apixaban compared to other direct oral anticoagulants for prevention of stroke in Austrian atrial fibrillation patients. Expert Rev Pharmacoecon Outcomes Res 2021;21(2):265–275
Funding
This study receives no external funding. There are no funding interests to declare.
Author information
Authors and Affiliations
Contributions
CHN and DJHT should be considered joint first author. MDM and CHN act as the joint submission guarantor. All authors approve the final version of the manuscript, including the authorship list and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Conceptualization and Design: CHN, FZW, NC, DQH, YYD, AJS, MDM. Acquisition of Data: CHN, DJHT, KRYN, JX. Analysis and Interpretation of Data: CHN, NS. Writing—original draft: CHN, DJHT, KRYN, NS, JX, FZW, NC. Writing—review and editing: DQH, YYD, AJS, MDM.
Corresponding authors
Ethics declarations
Conflict of interest
Arun J. Sanyal: Dr Sanyal is President of Sanyal Biotechnology and has stock options in Genfit, Akarna, Tiziana, Indalo, Durect and Galmed. He has served as a consultant to Astra Zeneca, Nitto Denko, Enyo, Ardelyx, Conatus, Nimbus, Amarin, Salix, Tobira, Takeda, Jannsen, Gilead, Terns, Birdrock, Merck, Valeant, Boehringer‐Ingelheim, Lilly, Hemoshear, Zafgen, Novartis, Novo Nordisk, Pfizer, Exhalenz and Genfit. He has been an unpaid consultant to Intercept, Echosens, Immuron, Galectin, Fractyl, Syntlogic, Affimune, Chemomab, Zydus, Nordic Bioscience, Albireo, Prosciento, Surrozen and Bristol Myers Squibb. His institution has received grant support from Gilead, Salix, Tobira, Bristol Myers, Shire, Intercept, Merck, Astra Zeneca, Malinckrodt, Cumberland and Novartis. He receives royalties from Elsevier and UptoDate. Remaining authors have no conflicts of interest to declare.
Animal research (ethics)
Not applicable.
Consent to participate (ethics)
Not applicable.
Consent to publish (ethics)
Not applicable.
Plant reproducibility
Not applicable.
Clinical Trials Registration
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ng, C.H., Tan, D.J.H., Nistala, K.R.Y. et al. A network meta-analysis of direct oral anticoagulants for portal vein thrombosis in cirrhosis. Hepatol Int 15, 1196–1206 (2021). https://doi.org/10.1007/s12072-021-10247-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10247-x