Abstract
Background
Psychometric hepatic encephalopathy score (PHES) needs local standardization.
Aims
This study aimed at standardizing PHES for Turkish patients and compare them with German norms; to determine minimal hepatic encephalopathy (mHE) prevalence with two different methods [PHES battery and Critical Flicker Frequency (CFF)] and to assess whether sub-tests of the battery can be used for screening for mHE.
Methods
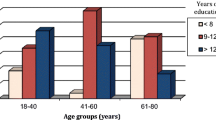
Healthy volunteers (n = 816; 400 male) and cirrhotics (n = 124; 58 male) were included. For mHE diagnosis PHES score threshold was set at ≤ − 5 points and that of CFF at < 39 Hz. For comparing German and Turkish norms, datasets were combined. Multiple backward procedure was applied to assess effects of age, sex and education on single tests of the battery. Receiver operating characteristic (ROC) curves were created for assessing diagnostic capabilities of subtests of the battery.
Results
PHES norms for Turks were developed. MHE prevalence in compensated cirrhotics was 29.8% and 27.4% with PHES and CFF tests, respectively, with low compatibility (kappa coefficient 0.389); mHE prevalence decreased to 16% when both tests were combined. Turks performed worse vs Germans in the digit symbol (DS) and serial dotting (SD) subtests but performed better in other subtests. In ROC analyzes of subtests, the combination of DS + SD tests achieved an AUROC of 0.974 versus PHES.
Conclusions
Use of two methods for diagnosing mHE is important for research purposes. From a clinical perspective, sensitivity with acceptable specificity may suffice for screening instruments for mHE. Combined use of DS and SD subtests of the PHES battery appears suitable for this purpose.





Similar content being viewed by others
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology 2014;60(2):715–735
Ridola L, Cardinale V, Riggio O. The burden of minimal hepatic encephalopathy: from diagnosis to therapeutic strategies. Ann Gastroenterol 2018;31(2):151–164
Morgan MY, Amodio P, Cook NA, Jackson CD, Kircheis G, Lauridsen MM, et al. Qualifying and quantifying minimal hepatic encephalopathy. Metab Brain Dis 2016;31(6):1217–1229
Groeneweg M, Quero JC, De Bruijn I, Hartmann IJ, Essink-bot ML, Hop WC, et al. Subclinical hepatic encephalopathy impairs daily functioning. Hepatology 1998;28(1):45–49
Agrawal S, Umapathy S, Dhiman RK. Minimal hepatic encephalopathy impairs quality of life. J Clin Exp Hepatol 2015;5(Suppl 1):S42–S48
Schomerus H, Hamster W. Quality of life in cirrhotics with minimal hepatic encephalopathy. Metab Brain Dis 2001;16(1–2):37–41
Wein C, Koch H, Popp B, Oehler G, Schauder P. Minimal hepatic encephalopathy impairs fitness to drive. Hepatology 2004;39(3):739–745
Bajaj JS, Ananthakrishnan AN, McGinley EL, Hoffman RG, Brasel KJ. Deleterious effect of cirrhosis on outcomes after motor vehicle crashes using the nationwide inpatient sample. Am J Gastroenterol 2008;103(7):1674–1681
Kircheis G, Knoche A, Hilger N, Manhart F, Schnitzler A, Schulze H, et al. Hepatic encephalopathy and fitness to drive. Gastroenterology 2009;137(5):1706–1715 (e1–e9)
Das A, Dhiman RK, Saraswat VA, Verma M, Naik SR. Prevalence and natural history of subclinical hepatic encephalopathy in cirrhosis. J Gastroenterol Hepatol 2001;16(5):531–535
Romero-Gomez M, Boza F, Garcia-Valdecasas MS, Garcia E, Aguilar-Reina J. Subclinical hepatic encephalopathy predicts the development of overt hepatic encephalopathy. Am J Gastroenterol 2001;96(9):2718–2723
Amodio P, Del Piccolo F, Marchetti P, Angeli P, Iemmolo R, Caregaro L, et al. Clinical features and survivial of cirrhotic patients with subclinical cognitive alterations detected by the number connection test and computerized psychometric tests. Hepatology 1999;29(6):1662–1667
Ampuero J, Simon M, Montoliu C, Jover R, Serra MA, Cordoba J, et al. Minimal hepatic encephalopathy and critical flicker frequency are associated with survival of patients with cirrhosis. Gastroenterology 2015;149(6):1483–1489
Quero JC, Hartmann IJ, Meulstee J, Hop WC, Schalm SW. The diagnosis of subclinical hepatic encephalopathy in patients with cirrhosis using neuropsychological tests and automated electroencephalogram analysis. Hepatology 1996;24(3):556–560
Groeneweg M, Moerland W, Quero JC, Hop WC, Krabbe PF, Schalm SW. Screening of subclinical hepatic encephalopathy. J Hepatol 2000;32(5):748–753
Lee Y, Kim C, Suk KT, Choi HC, Bang CS, Yoon JH, et al. Differences in cognitive function between patients with viral and alcoholic compensated liver cirrhosis. Metab Brain Dis 2016;31(2):369–376
Weissenborn K, Ennen JC, Schomerus H, Ruckert N, Hecker H. Neuropsychological characterization of hepatic encephalopathy. J Hepatol 2001;34(5):768–773
Lauridsen MM, Thiele M, Kimer N, Vilstrup H. The continuous reaction times method for diagnosing, grading, and monitoring minimal/covert hepatic encephalopathy. Metab Brain Dis 2013;28(2):231–234
Bajaj JS, Hafeezullah M, Franco J, Varma RR, Hoffmann RG, Knox JF, et al. Inhibitory control test for the diagnosis of minimal hepatic encephalopathy. Gastroenterology 2008;135(5):1591–1600 (e1)
Bajaj JS, Thacker LR, Heuman D, Fuchs M, Sterling RK, Sanyal AJ, et al. The Stroop smartphone application is a short and valid method to screen for minimal hepatic encephalopathy. Hepatology 2013;58(3):1122–1132
Kircheis G, Wettstein M, Timmermann L, Schnitzler A, Haussinger D. Critical flicker frequency for quantification of low-grade hepatic encephalopathy. Hepatology 2002;35(2):357–366
Bajaj JS, Cordoba J, Mullen KD, Amodio P, Shawcross DL, Butterworth RF, et al. Review article: the design of clinical trials in hepatic encephalopathy—an International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) consensus statement. Aliment Pharmacol Ther 2011;33(7):739–747
Haussinger D, Laubenberger J, vom Dahl S, Ernst T, Bayer S, Langer M, et al. Proton magnetic resonance spectroscopy studies on human brain myo-inositol in hypo-osmolarity and hepatic encephalopathy. Gastroenterology 1994;107(5):1475–1480
Singhal A, Nagarajan R, Hinkin CH, Kumar R, Sayre J, Elderkin-Thompson V, et al. Two-dimensional MR spectroscopy of minimal hepatic encephalopathy and neuropsychological correlates in vivo. J Magn Reson Imaging 2010;32(1):35–43
Razek AA, Abdalla A, Ezzat A, Megahed A, Barakat T. Minimal hepatic encephalopathy in children with liver cirrhosis: diffusion-weighted MR imaging and proton MR spectroscopy of the brain. Neuroradiology 2014;56(10):885–891
Schomerus H, Hamster W. Neuropsychological aspects of portal-systemic encephalopathy. Metab Brain Dis 1998;13(4):361–377
Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology 2002;35(3):716–721
Amodio P, Campagna F, Olianas S, Iannizzi P, Mapelli D, Penzo M, et al. Detection of minimal hepatic encephalopathy: normalization and optimization of the Psychometric Hepatic Encephalopathy Score. A neuropsychological and quantified EEG study. J Hepatol 2008;49(3):346–353
Romero Gomez M, Cordoba J, Jover R, del Olmo J, Fernandez A, Flavia M, et al. Normality tables in the Spanish population for psychometric tests used in the diagnosis of minimal hepatic encephalopathy. Med Clin (Barc) 2006;127(7):246–249
Wunsch E, Koziarska D, Kotarska K, Nowacki P, Milkiewicz P. Normalization of the psychometric hepatic encephalopathy score in Polish population. A prospective, quantified electroencephalography study. Liver Int 2013;33(9):1332–1340
Seo YS, Yim SY, Jung JY, Kim CH, Kim JD, Keum B, et al. Psychometric hepatic encephalopathy score for the detection of minimal hepatic encephalopathy in Korean patients with liver cirrhosis. J Gastroenterol Hepatol 2012;27(11):1695–1704
Duarte-Rojo A, Estradas J, Hernandez-Ramos R, Ponce-de-Leon S, Cordoba J, Torre A. Validation of the psychometric hepatic encephalopathy score (PHES) for identifying patients with minimal hepatic encephalopathy. Dig Dis Sci 2011;56(10):3014–3023
Romero-Gomez M, Cordoba J, Jover R, del Olmo JA, Ramirez M, Rey R, et al. Value of the critical flicker frequency in patients with minimal hepatic encephalopathy. Hepatology 2007;45(4):879–885
Goldbecker A, Weissenborn K, Hamidi Shahrezaei G, Afshar K, Rumke S, Barg-Hock H, et al. Comparison of the most favoured methods for the diagnosis of hepatic encephalopathy in liver transplantation candidates. Gut 2013;62(10):1497–1504
Dhiman RK, Kurmi R, Thumburu KK, Venkataramarao SH, Agarwal R, Duseja A, et al. Diagnosis and prognostic significance of minimal hepatic encephalopathy in patients with cirrhosis of liver. Dig Dis Sci 2010;55(8):2381–2390
American Association for the Study of Liver Diseases, European Association for the Study of the Liver. Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. J Hepatol 2014;61(3):642–659
Kircheis G, Hilger N, Haussinger D. Value of critical flicker frequency and psychometric hepatic encephalopathy score in diagnosis of low-grade hepatic encephalopathy. Gastroenterology 2014;146(4):961–969
Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983;148(3):839–843
Bajaj JS, Etemadian A, Hafeezullah M, Saeian K. Testing for minimal hepatic encephalopathy in the United States: an AASLD survey. Hepatology 2007;45(3):833–834
Schomerus H, Weissenborn K, Hamster W, RuÈckert N, Hecker H. PSE-Syndrom-Test Swets Test Services. Frankfurt: Swets & Zeitlinger; 1999
Riggio O, Ridola L, Pasquale C, Pentassuglio I, Nardelli S, Moscucci F, et al. A simplified psychometric evaluation for the diagnosis of minimal hepatic encephalopathy. Clin Gastroenterol Hepatol 2011;9(7):613–616 (e1)
Campagna F, Montagnese S, Ridola L, Senzolo M, Schiff S, De Rui M, et al. The animal naming test: an easy tool for the assessment of hepatic encephalopathy. Hepatology 2017;66(1):198–208
Barbosa M, Marinho C, Mota P, Cotter J. Minimal hepatic encephalopathy: the reality beyond our eyes. Acta Med Port 2015;28(4):480–485
Torlot FJ, McPhail MJ, Taylor-Robinson SD. Meta-analysis: the diagnostic accuracy of critical flicker frequency in minimal hepatic encephalopathy. Aliment Pharmacol Ther 2013;37(5):527–536
Funding
The Critical Flicker Frequency device was kindly provided by ASSOS Pharmaceuticals throughout the study. We did not receive any financial support for conducting the study.
Author information
Authors and Affiliations
Contributions
CY, FG and KW contributed to the study design. BO, OK, IK, CO, CK, AC, FOO, BKÖ contributed to acquisition of data, BO, CO, HH, FG, KW and CY contributed to data analysis, interpretation of data, drafting of the manuscript, BO, OK, HH, GG, MA, FG, OO, KW, CY contributed to revising of the manuscript. All authors have seen and approved the last version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Burak Ozbas, Onur Keskin, Hartmut Hecker, Irfan Karahan, Cansu Ozbas, Cagdas Kalkan, Aysun Kartal, Fatih Oguz Onder, Burcu Kahveci Oncu, Genco Gencdal, Murat Akyildiz, Fulya Gunsar, Ramazan Idilman, Karin Weissenborn, Omer Ozutemiz, Cihan Yurdaydin declare no competing interests.
Ethics approval
The study was approved by the University of Ankara Medical School Ethics Committee. The experiments conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Informed consent
Informed consent was obtained from patients, prior to their participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12072_2021_10207_MOESM2_ESM.docx
Comparison of the psychometric hepatic encephalopathy scores in German and Turkish healthy populations by applying German and Turkish norms to both populations. No significant differences were found between the populations when Turkish norms were applied, but 142 of 785 subjects classified as normal with Turkish norms would be classified as out of norm if the Hannover Scores were applied (DOCX 51 kb)
Rights and permissions
About this article
Cite this article
Özbaş, B., Keskin, O., Hecker, H. et al. Determination of Turkish norms of psychometric tests for diagnosing minimal hepatic encephalopathy and proposal of a high sensitive screening test battery. Hepatol Int 15, 1442–1455 (2021). https://doi.org/10.1007/s12072-021-10207-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10207-5