Abstract
Idiosyncratic drug-induced liver injury mimics acute and chronic liver disease. It is under recognized and underrecognised because of the lack of pathognomonic diagnostic serological markers. Its consequences may vary from being asymptomatic to self-limiting illness to severe liver injury leading to acute liver failure. Its incidence is likely to be more common in Asia than other parts of the world, mainly because of hepatotoxicity resulting from the treatment of tuberculosis disease and the ubiquitous use of traditional and complimentary medicines in Asian countries. This APASL consensus guidelines on DILI is a concise account of the various aspects including current evidence-based information on DILI with special emphasis on DILI due to antituberculosis agents and traditional and complementary medicine use in Asia.
Similar content being viewed by others
References
World Health Organization. Global tuberculosis report 2019:1–283
Saukkonen JJ, Cohn DL, Jasmer RM, et al. An official ATS statement: hepatotoxicity of antituberculosis therapy. Am J Respir Crit Care Med 2006;174:935–952.
World HealthOrganization. Traditional Medicine Strategy 2014–23. 2013.
Shen T, Liu Y, Shang J, et al. Incidence and etiology of drug-induced liver injury in Mainland China. Gastroenterology 2019;156:2230–2241.
Björnsson HK, Björnsson ES, Avula B, et al. Ashwagandha-induced liver injury: a case series from Iceland and the US drug-induced liver injury network. Liver Int 2020;40:825–829.
Sgro C, Clinard F, Ouazir K, et al. Incidence of drug-induced hepatic injuries: a French population-based study. Hepatology. 2002;36:451–455.
Bjornsson ES, Bergmann OM, Bjornsson HK, et al. Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013;144:1419–1425.
Suk KT, Kim DJ, Kim CH, et al. A prospective nationwide study of drug-induced liver injury in Korea. Am J Gastroenterol 2012;107:1380–1387.
Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott; 1999.
Aithal GP, Watkins PB, Andrade RJ, et al. Case definition and phenotype standardization in drug-induced liver injury. Clin Pharmacol Ther 2011;89:806–815.
Group GW. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490.
Moore TJ, Cohen MR, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998–2005. Arch Intern Med 2007;167:1752–1759.
Danan G, Benichou C. Causality assessment of adverse reactions to drugs—I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J Clin Epidemiol 1993;46:1323–1330.
Lucena MI, Andrade RJ, Kaplowitz N, et al. Phenotypic characterization of idiosyncratic drug-induced liver injury: the influence of age and sex. Hepatology 2009;49:2001–2009.
Chalasani N, Bonkovsky HL, Fontana R, et al. Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterology 2015;148:1340–1352.
Tostmann A, Boeree MJ, Aarnoutse RE, et al. Antituberculosis drug-induced hepatotoxicity: concise up-to-date review. J Gastroenterol Hepatol 2008;23:192–202.
Fountain FF, Tolley E, Chrisman CR, et al. Isoniazid hepatotoxicity associated with treatment of latent tuberculosis infection: a 7-year evaluation from a public health tuberculosis clinic. Chest 2005;128:116–123.
Bryant AE, Dreifuss FE. Valproic acid hepatic fatalities. III. US experience since 1986. Neurology 1996;46:465–469.
Cai Y, Yi J, Zhou C, et al. Pharmacogenetic study of drug-metabolising enzyme polymorphisms on the risk of anti-tuberculosis drug-induced liver injury: a meta-analysis. PLoS ONE 2012;7:e47769.
Nicoletti P, Devarbhavi H, Goel A, et al. Genome-wide association study (GWAS) to identify genetic risk factors that increase susceptibility to antituberculosis drug-induced liver injury (ATDILI). Hepatology 2017;66:Abstract-25.
Lucena MI, Molokhia M, Shen Y, et al. Susceptibility to amoxicillin-clavulanate-induced liver injury is influenced by multiple HLA class I and II alleles. Gastroenterology 2011;141:338–347.
Cirulli ET, Nicoletti P, Abramson K, et al. A missense variant in PTPN22 is a risk factor for drug-induced liver injury. Gastroenterology 2019;156(1707–1716):e2.
Zimmerman HJ. Effects of alcohol on other hepatotoxins. Alcohol Clin Exp Res 1986;10:3–15.
Bruno S, Maisonneuve P, Castellana P, et al. Incidence and risk factors for non-alcoholic steatohepatitis: prospective study of 5408 women enrolled in Italian tamoxifen chemoprevention trial. BMJ 2005;330:932.
Saphner T, Triest-Robertson S, Li H, et al. The association of nonalcoholic steatohepatitis and tamoxifen in patients with breast cancer. Cancer 2009;115:3189–195.
Wong WM, Wu PC, Yuen MF, et al. Antituberculosis drug-related liver dysfunction in chronic hepatitis B infection. Hepatology 2000;31:201–206.
Chalasani N, Bjornsson E. Risk factors for idiosyncratic drug-induced liver injury. Gastroenterology 2010;138:2246–2259.
Russo MW, Watkins PB. Are patients with elevated liver tests at increased risk of drug-induced liver injury? Gastroenterology 2004;126:1477–1480.
Sarma GR, Immanuel C, Kailasam S, et al. Rifampin-lnduced release of hydrazine from isoniazid: a possible cause of hepatitis during treatment of tuberculosis with regimens containing isoniazid and rifampin. Am Rev Respir Dis 1986;133:1072–1075.
Balzarini J, Lee CK, Herdewijn P, et al. Mechanism of the potentiating effect of ribavirin on the activity of 2’,3’-dideoxyinosine against human immunodeficiency virus. J Biol Chem 1991;266:21509–21514.
Mira JA, Macías J, Girón-González JA, et al. Incidence of and risk factors for severe hepatotoxicity of nelfinavir-containing regimens among HIV-infected patients with chronic hepatitis C. J Antimicrob Chemother 2006;58:140–146.
Navarro VJ, Barnhart H, Bonkovsky HL, et al. Liver injury from herbals and dietary supplements in the US drug-induced liver injury network. Hepatology 2014;60:1399–1408.
Bailey RL, Gahche JJ, Lentino CV, et al. Dietary supplement use in the United States, 2003–2006. J Nutr 2011;141:261–266.
Andrade RJ, Lucena MI, Fernandez MC, et al. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish registry over a 10-year period. Gastroenterology 2005;129:512–521.
Medina-Caliz I, Robles-Diaz M, Garcia-Munoz B, et al. Definition and risk factors for chronicity following acute idiosyncratic drug-induced liver injury. J Hepatol 2016;65:532–542.
Lee T, Lee YS, Yoon SY, et al. Characteristics of liver injury in drug-induced systemic hypersensitivity reactions. J Am Acad Dermatol 2013;69:407–415.
Devarbhavi H, Karanth D, Prasanna KS, et al. Drug-Induced liver injury with hypersensitivity features has a better outcome: a single-center experience of 39 children and adolescents. Hepatology 2011;54:1344–1350.
Devarbhavi H, Raj S, Aradya VH, et al. Drug-induced liver injury associated with stevens-Johnson syndrome/toxic epidermal necrolysis: patient characteristics, causes, and outcome in 36 cases. Hepatology 2016;63:993–999.
Knowles SR, Dewhurst N, Shear NH. Anticonvulsant hypersensitivity syndrome: an update. Expert Opin Drug Saf 2012;11:767–778.
Benichou C. Criteria of drug-induced liver disorders. Report of an international consensus meeting. J Hepatol 1990;11:272–276.
Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med 2006;354:731–739.
Licata A, Maida M, Cabibi D, et al. Clinical features and outcomes of patients with drug-induced autoimmune hepatitis: a retrospective cohort study. Dig Liver Dis 2014;46:1116–120.
Bjornsson E, Talwalkar J, Treeprasertsuk S, et al. Drug-induced autoimmune hepatitis: clinical characteristics and prognosis. Hepatology 2010;51:2040–2048.
Aithal PG, Day CP. The natural history of histologically proved drug induced liver disease. Gut 1999;44:731–735.
de Boer YS, Kosinski AS, Urban TJ, et al. Features of autoimmune hepatitis in patients with drug-induced liver injury. Clin Gastroenterol Hepatol 2017;15(103–112):e2.
Lucena MI, Kaplowitz N, Hallal H, et al. Recurrent drug-induced liver injury (DILI) with different drugs in the Spanish Registry: the dilemma of the relationship to autoimmune hepatitis. J Hepatol 2011;55:820–827.
Rodrigues S, Lopes S, Magro F, et al. Autoimmune hepatitis and anti-tumor necrosis factor alpha therapy: a single center report of 8 cases. World J Gastroenterol 2015;21:7584–7588.
Perdices EV, Medina-Caliz I, Hernando S, et al. Hepatotoxicity associated with statin use: analysis of the cases included in the Spanish Hepatotoxicity Registry. Rev Esp Enferm Dig 2014;106:246–254.
Larrey D. Epidemiology and individual susceptibility to adverse drug reactions affecting the liver. Semin Liver Dis 2002;22:145–155.
Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 2018;15:11–20.
Dawwas MF, Aithal GP. End-stage methotrexate-related liver disease is rare and associated with features of the metabolic syndrome. Aliment Pharmacol Ther 2014;40:938–948.
Raja K, Thung SN, Fiel MI, et al. Drug-induced steatohepatitis leading to cirrhosis: long-term toxicity of amiodarone use. Semin Liver Dis 2009;29:423–438.
Miyake K, Hayakawa K, Nishino M, et al. Effects of oral 5-fluorouracil drugs on hepatic fat content in patients with colon cancer. Acad Radiol 2005;12:722–727.
Andrade RJ, Lucena MI, Kaplowitz N, et al. Outcome of acute idiosyncratic drug-induced liver injury: long-term follow-up in a hepatotoxicity registry. Hepatology 2006;44:1581–1588.
Robles-Diaz M, Garcia-Cortes M, Medina-Caliz I, et al. The value of serum aspartate aminotransferase and gamma-glutamyl transpetidase as biomarkers in hepatotoxicity. Liver Int 2015;35:2474–2482.
Temple R. Hy’s law: predicting serious hepatotoxicity. Pharmacoepidemiol Drug Saf 2006;15:241–243.
Chalasani N, Fontana RJ, Bonkovsky HL, et al. Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008;135:1924–1934 ((1934 e1–4)).
Horsley-Silva JL, Dow EN, Menias CO, et al. Docetaxel induced sclerosing cholangitis. Dig Dis Sci 2015;60:3814–3816.
Ludwig J, Kim CH, Wiesner RH, et al. Floxuridine-induced sclerosing cholangitis: an ischemic cholangiopathy? Hepatology 1989;9:215–218.
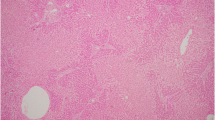
Ramachandran R, Kakar S. Histological patterns in drug-induced liver disease. J Clin Pathol 2009;62:481–492.
Kleiner DE, Chalasani NP, Lee WM, et al. Hepatic histological findings in suspected drug-induced liver injury: systematic evaluation and clinical associations. Hepatology 2014;59:661–670.
Arimone Y, Bégaud B, Miremont-Salamé G, et al. Agreement of expert judgment in causality assessment of adverse drug reactions. Eur J Clin Pharmacol 2005;61:169–173.
Aithal GP, Rawlins MD, Day CP. Accuracy of hepatic adverse drug reaction reporting in one English health region. BMJ 1999;319:1541.
Benichou C, Danan G, Flahault A. Causality assessment of adverse reactions to drugs—II. An original model for validation of drug causality assessment methods: case reports with positive rechallenge. J Clin Epidemiol 1993;46:1331–1336.
Chalasani NP, Hayashi PH, Bonkovsky HL, et al. ACG clinical guideline: the diagnosis and management of idiosyncratic drug-induced liver injury. Am J Gastroenterol 2014;109:950–966.
Andrade RJ, Aithal GP, Björnsson ES, et al. EASL clinical practice guidelines: drug-induced liver injury. J Hepatol. 2019;70:1222–1261.
Maria VA, Victorino RM. Development and validation of a clinical scale for the diagnosis of drug-induced hepatitis. Hepatology 1997;26:664–669.
Lucena MI, Camargo R, Andrade RJ, et al. Comparison of two clinical scales for causality assessment in hepatotoxicity. Hepatology. 2001;33:123–130.
Tillmann HL, Suzuki A, Barnhart HX, et al. Tools for causality assessment in drug-induced liver disease. Curr Opin Gastroenterol. 2019;35:183–190.
Rockey DC, Seeff LB, Rochon J, et al. Causality assessment in drug-induced liver injury using a structured expert opinion process: comparison to the Roussel-Uclaf causality assessment method. Hepatology. 2010;51:2117–2126.
Takikawa H, Onji M. A proposal of the diagnostic scale of drug-induced liver injury. Hepatol Res. 2005;32:250–251.
Takikawa H, Onji M, Takamori Y, et al. Proposal of diagnostic criteria for drug-induced liver injury revised by the DDW-J 2004 workshop. Kanzo. 2005;46:85–90.
Kanayama A, Arima Y, Yamagishi T, et al. Epidemiology of domestically acquired hepatitis E virus infection in Japan: assessment of the nationally reported surveillance data, 2007–2013. J Med Microbiol 2015;64:752–758.
Hanatani T, Sai K, Tohkin M, et al. A detection algorithm for drug-induced liver injury in medical information databases using the Japanese diagnostic scale and its comparison with the council for international organizations of medical sciences/the roussel uclaf causality assessment method scale. Pharmacoepidemiol Drug Saf 2014;23:984–988.
Whritenour J, Ko M, Zong Q, et al. Development of a modified lymphocyte transformation test for diagnosing drug-induced liver injury associated with an adaptive immune response. J Immunotoxicol 2017;14:31–38.
Fontana RJ, Hayashi PH, Gu J, et al. Idiosyncratic drug-induced liver injury is associated with substantial morbidity and mortality within 6 months from onset. Gastroenterology 2014;147(96–108):e4.
Hunt CM. Mitochondrial and immunoallergic injury increase risk of positive drug rechallenge after drug-induced liver injury: a systematic review. Hepatology 2010;52:2216–2222.
Hunt CM, Papay JI, Stanulovic V, et al. Drug rechallenge following drug-induced liver injury. Hepatology 2017;66:646–654.
Papay JI, Clines D, Rafi R, et al. Drug-induced liver injury following positive drug rechallenge. Regul Toxicol Pharmacol 2009;54:84–90.
Sharma SK, Singla R, Sarda P, et al. Safety of 3 different reintroduction regimens of antituberculosis drugs after development of antituberculosis treatment-induced hepatotoxicity. Clin Infect Dis 2010;50:833–839.
Ataç G, Sevim T, Törün T, et al. The management of anti-tuberculosis drug-induced hepatotoxicity. Int J Tuberc Lung Dis 2001;5:65–69.
Powles T, Bracarda S, Chen M, et al. Characterisation of liver chemistry abnormalities associated with pazopanib monotherapy: a systematic review and meta-analysis of clinical trials in advanced cancer patients. Eur J Cancer 2015;51:1293–1302.
Daly AK, Donaldson PT, Bhatnagar P, et al. HLA-B*5701 genotype is a major determinant of drug-induced liver injury due to flucloxacillin. Nat Genet 2009;41:816–819.
Aithal GP. Of potions, poisons, polygonum and pre-emptive polymorphism. Hepatology 2019;70:8–10.
Kaliyaperumal K, Grove JI, Delahay RM, et al. Pharmacogenomics of drug-induced liver injury (DILI): molecular biology to clinical applications. J Hepatol 2018;69:948–957.
Aithal GP. Pharmacogenetic testing in idiosyncratic drug-induced liver injury: current role in clinical practice. Liver Int 2015;35:1801–1808.
Lohse AW, Chazouilleres O, Dalekos G, et al. EASL clinical practice guidelines: autoimmune hepatitis. J Hepatol 2015;63:971–1004.
Alvarez F, Berg PA, Bianchi FB, et al. International Autoimmune Hepatitis Group report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol 1999;31:929–938.
https://c-path.org/critical-path-institute-receives-regulatory-support-for-liver-injury-biomarker/
Church RJ, Kullak-Ublick GA, Aubrecht J, et al. Candidate biomarkers for the diagnosis and prognosis of drug-induced liver injury: an international collaborative effort. Hepatology 2019;69:760–773.
Bjornsson E, Olsson R. Outcome and prognostic markers in severe drug-induced liver disease. Hepatology 2005;42:481–489.
Robles-Diaz M, Lucena MI, Kaplowitz N, et al. Use of Hy’s law and a new composite algorithm to predict acute liver failure in patients with drug-induced liver injury. Gastroenterology 2014;147:109–118.
Olsson R, Wiholm B-E, Sand C, et al. Liver damage from flucloxacillin, cloxacillin and dicloxacillin. J Hepatol 1992;15:154–161.
Björnsson E, Davidsdottir L. The long-term follow-up after idiosyncratic drug-induced liver injury with jaundice. J Hepatol 2009;50:511–517.
Hayashi PH, Fontana RJ. Clinical features, diagnosis, and natural history of drug-induced liver injury. In: Seminars in liver disease. Thieme Medical Publishers 2014.
Devarbhavi H, Dierkhising R, Kremers WK, et al. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol 2010;105:2396–2404.
Prakash A, Jarvis B. Leflunomide: a review of its use in active rheumatoid arthritis. Drugs 1999;58:1137–1164.
Bohan TP, Helton E, McDonald I, et al. Effect of l-carnitine treatment for valproate-induced hepatotoxicity. Neurology 2001;56:1405–1409.
Lheureux PE, Hantson P. Carnitine in the treatment of valproic acid-induced toxicity. Clin Toxicol (Phila) 2009;47:101–111.
Chan Y-C, Tse M, Lau FL. Two cases of valproic acid poisoning treated with l-carnitine. Hum Exp Toxicol 2007;26:967–969.
Glatstein M, Rino PB, de Pinho S, et al. Levocarnitine for the treatment of valproic acid-induced hyperammonemic encephalopathy in children: the experience of a large, Tertiary Care Pediatric Hospital and a Poison Center. Am J Ther 2019;26:e344–e349.
Health NIo. Livertox: clinical and research information on drug-induced liver injury. Nih. gov https://www.livertox/nih.gov 2017.
Lee WM, Hynan LS, Rossaro L, et al. Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Gastroenterology 2009;137:856–864.
Borlak J, van Bömmel F, Berg T. N-Acetylcysteine and prednisolone treatment improved serum biochemistries in suspected flupirtine cases of severe idiosyncratic liver injury. Liver Int 2018;38:365–376.
Elliott TR, Symes T, Kannourakis G, et al. Resolution of norfloxacin-induced acute liver failure after N-acetylcysteine therapy: further support for the use of NAC in drug-induced ALF? BMJ Case Rep 2016;6:2015-213189.
Zhao Z, Bao L, Yu X, et al. Acute vanishing bile duct syndrome after therapy with cephalosporin, metronidazole, and clotrimazole: a case report. Medicine 2017;96:e8009.
Danica J, Irena H, Davor R, et al. Vanishing bile duct syndrome associated with azithromycin in a 62-year-old man. Basic Clin Pharmacol Toxicol 2010;106:62–65.
Doherty GJ, Duckworth AM, Davies SE, et al. Severe steroid-resistant anti-PD1 T-cell checkpoint inhibitor-induced hepatotoxicity driven by biliary injury. ESMO Open 2017;2:e000268.
Kurokawa K, Hara M, Iwakami S-I, et al. Cholestatic liver injury induced by pembrolizumab in a patient with lung adenocarcinoma. Intern Med 2019;58:3283–3287.
Wree A, Dechêne A, Herzer K, et al. Steroid and ursodesoxycholic acid combination therapy in severe drug-induced liver injury. Digestion 2011;84:54–59.
Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol 2013;169:1071–1080.
Darnell EP, Mooradian MJ, Baruch EN, et al. Immune-related adverse events (irAEs): diagnosis, management, and clinical pearls. Curr Oncol Rep 2020;22:39.
Czaja AJ. Drug-induced autoimmune-like hepatitis. Dig Dis Sci 2011;56:958–976.
Nishida N, Kudo M. Liver damage related to immune checkpoint inhibitors. Hepatol Int 2019;13:248–252.
Ostapowicz G, Fontana RJ, Schiodt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med 2002;137:947–954.
Serper M, Wolf MS, Parikh NA, et al. Risk factors, clinical presentation, and outcomes in overdose with acetaminophen alone or with combination products: results from the acute liver failure study group. J Clin Gastroenterol 2016;50:85.
Hillman L, Gottfried M, Whitsett M, et al. Clinical features and outcomes of complementary and alternative medicine induced acute liver failure and injury. Am J Gastroenterol 2016;111:958–965.
Reuben A, Koch DG, Lee WM. Drug-induced acute liver failure: results of a US multicenter, prospective study. Hepatology 2010;52:2065–2076.
Adam R, Karam V, Cailliez V, et al 2018 annual report of the European Liver Transplant Registry (ELTR)—50-year evolution of liver transplantation. Transpl Int 2018;31:1293–1317.
Saliba F, Camus C, Durand F, et al. Albumin dialysis with a noncell artificial liver support device in patients with acute liver failure: a randomized, controlled trial. Ann Intern Med 2013;159:522–531.
Larsen FS, Schmidt LE, Bernsmeier C, et al. High-volume plasma exchange in patients with acute liver failure: an open randomised controlled trial. J Hepatol 2016;64:69–78.
Chiew AL, Gluud C, Brok J, et al. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst Rev 2018;2:Cd003328.
Stravitz RT, Sanyal AJ, Reisch J, et al. Effects of N-acetylcysteine on cytokines in non-acetaminophen acute liver failure: potential mechanism of improvement in transplant-free survival. Liver International 2013;33:1324–1331.
Singh S, Hynan LS, Lee WM, et al. Improvements in hepatic serological biomarkers are associated with clinical benefit of intravenous N-acetylcysteine in early stage non-acetaminophen acute liver failure. Dig Dis Sci 2013;58:1397–1402.
Kortsalioudaki C, Taylor RM, Cheeseman P, et al. Safety and efficacy of N-acetylcysteine in children with non-acetaminophen-induced acute liver failure. Liver Transpl 2008;14:25–30.
Squires RH, Dhawan A, Alonso E, et al. Intravenous N-acetylcysteine in pediatric patients with nonacetaminophen acute liver failure: a placebo-controlled clinical trial. Hepatology 2013;57:1542–1549.
Hunt CM, Forster JK, Papay JI, et al. Evidence-based liver chemistry monitoring in drug development. Pharm Med 2009;23:149–158.
Boelsterli UA. Chapter 21—mechanisms underlying the hepatotoxicity of nonsteroidal antiinflammatory drugs. In: Kaplowitz N, DeLeve LD, editors. Drug-induced liver disease. 3rd ed. Boston: Academic Press; 2013. p. 343–367.
Björnsson ES. Drug-induced liver injury: an overview over the most critical compounds. Arch Toxicol 2015;89:327–334.
Ribas A, Hodi FS, Callahan M, et al. Hepatotoxicity with combination of vemurafenib and ipilimumab. N Engl J Med 2013;368:1365–1366.
Dara L, Liu ZX, Kaplowitz N. Mechanisms of adaptation and progression in idiosyncratic drug induced liver injury, clinical implications. Liver Int 2016;36:158–165.
Navarro VJ, Khan I, Björnsson E, et al. Liver injury from herbal and dietary supplements. Hepatology 2017;65:363–373.
Li C, Rao T, Chen X, et al. HLA-B* 35: 01 allele is a potential biomarker for predicting polygonum multiflorum-induced liver injury in humans. Hepatology 2019;70:346–357.
Zhang L, Niu M, Wei A-W, et al. Risk profiling using metabolomic characteristics for susceptible individuals of drug-induced liver injury caused by Polygonum multiflorum. Arch Toxicol 2020;94:245–256.
Aiso M, Takikawa H, Tsuji K, et al. Analysis of 307 cases with drug-induced liver injury between 2010 and 2018 in Japan. Hepatol Res 2019;49:105–110.
Dai N, Yu Y-C, Ren T-H, et al. Gynura root induces hepatic veno-occlusive disease: a case report and review of the literature. World J Gastroenterol WJG 2007;13:1628.
Helmy A. updates in the pathogenesis and therapy of hepatic sinusoidal obstruction syndrome. Aliment Pharmacol Ther 2006;23:11–25.
Xiao X, Tang J, Mao Y, et al. Guidance for the clinical evaluation of traditional Chinese medicine-induced liver injuryIssued by China Food and Drug Administration. Acta Pharm Sin B 2019;9:648.
Yu Y-c, Mao Y-m, Chen C-w, et al. CSH guidelines for the diagnosis and treatment of drug-induced liver injury. Hepatol Int 2017;11:221–241.
Xia Q, Zhao Y, Lin G, et al. Pyrrolizidine alkaloid-protein adducts: potential non-invasive biomarkers of pyrrolizidine alkaloid-induced liver toxicity and exposure. Chem Res Toxicol 2016;29:1282–1292.
Wang Y, Wang Z, Gao M, et al. Efficacy and safety of magnesium isoglycyrrhizinate injection in patients with acute drug-induced liver injury: a phase II trial. Liver Int 2019;39:2102–2111.
Zhu Y, Niu M, Chen J, et al. Hepatobiliary and pancreatic: comparison between Chinese herbal medicine and Western medicine-induced liver injury of 1985 patients. J Gastroenterol Hepatol 2016;31:1476–1482.
Medina-Caliz I, Garcia-Cortes M, Gonzalez-Jimenez A, et al. Herbal and dietary supplement-induced liver injuries in the Spanish DILI registry. Clin Gastroenterol Hepatol 2018;16:1495–1502.
Devarbhavi H. Ayurvedic and herbal medicine-induced liver injury: It is time to wake up and take notice. Indian J Gastroenterol 2018;37(1):5–7. https://doi.org/10.1007/s12664-018-0820-6 ((Epub 2018 Feb 8)).
Pandey M, Rastogi S, Rawat A. Indian traditional ayurvedic system of medicine and nutritional supplementation. Evidence-Based Complementary and Alternative Medicine 2013;2013:376327. https://doi.org/10.1155/2013/376327.
Rudra S, Kalra A, Kumar A, et al. Utilization of alternative systems of medicine as health care services in India: evidence on AYUSH care from NSS 2014. PLoS ONE 2017;12:e0176916.
Devarbhavi H, Joseph T, Kumar NS, et al. Causes, clinical features, outcomes and predictors of mortality from a nationwide prospective study of drug-induced liver injury. Hepatology 2019;70:1219A.
Devarbhavi H, Choudhury AK, Sharma MK, et al. Drug-induced acute-on-chronic liver failure in Asian patients. Am J Gastroenterol 2019;114:929–937.
Philips CA, Paramaguru R, Joy AK, et al. Clinical outcomes, histopathologic patterns and chemical analysis of ayurveda and herbal medicine associated with severe liver injury—a single center experience from South India. Indian J Gastroenterol 2018;37:9–17.
Philips CA, Paramaguru R, Augustine P, et al. A Single-center experience on outcomes of complementary and alternative medicine use among patients with cirrhosis. Hepatol Commun 2019;3:1001–1012.
Chauhan A, Semwal DK, Mishra SP, et al. Ayurvedic research and methodology: present status and future strategies. Ayu 2015;36:364.
Hayashi PH, Barnhart HX, Fontana RJ, et al. Reliability of causality assessment for drug, herbal and dietary supplement hepatotoxicity in the Drug-Induced Liver Injury Network (DILIN). Liver Int 2015;35:1623–1632.
Danan G, Teschke R. RUCAM in drug and herb induced liver injury: the update. Int J Mol Sci 2016;17:14.
Philips CA, Augustine P, Rajesh S, et al. Complementary and alternative medicine-related drug-induced liver injury in Asia. J Clin Transl Hepatol 2019;7:263.
Agarwal VK, McHutchison JG, Hoofnagle JH, et al. Important elements for the diagnosis of drug-induced liver injury. Clin Gastroenterol Hepatol 2010;8:463–470.
Teschke R, Bahre R. Severe hepatotoxicity by Indian ayurvedic herbal products: a structured causality assessment. Ann Hepatol 2009;8:258–266.
Andrade RJ, Robles-Díaz M. Diagnostic and prognostic assessment of suspected drug-induced liver injury in clinical practice. Liver Int 2020;40:6–17.
Hayashi PH, Rockey D, Fontana RJ, et al. Death and liver transplantation within two years of onset of drug-induced liver injury. Hepatology 2017;23:29283.
Grewal P, Ahmad J. Severe liver injury due to herbal and dietary supplements and the role of liver transplantation. World J Gastroenterol 2019;25:6704.
Andrade RJ. Landscape of liver injury from herbal and dietary supplements in Europe, Latin America, and Asia. Clin Liver Dis 2019;14:49.
Philips CA, Rajesh S, George T, et al. Outcomes and toxicology of herbal drugs in alcoholic hepatitis—a single center experience from India. J Clin Transl Hepatol 2019;7:329.
Patwardhan B. Ayurvedic drugs in case: claims, evidence, regulations and ethics. J Ayurveda Integr Med 2016;7:135.
Tweed CD, Wills GH, Crook AM, et al. Liver toxicity associated with tuberculosis chemotherapy in the REMoxTB study. BMC Med 2018;16:46.
Singanayagam A, Sridhar S, Dhariwal J, et al. A comparison between two strategies for monitoring hepatic function during antituberculous therapy. Am J Respir Crit Care Med 2012;185:653–659.
Devarbhavi H, Singh R, Patil M, et al. Outcome and determinants of mortality in 269 patients with combination anti-tuberculosis drug-induced liver injury. J Gastroenterol Hepatol 2013;28:161–167.
Devarbhavi H, Patil M, Reddy VV, et al. Drug-induced acute liver failure in children and adults: results of a single-centre study of 128 patients. Liver Int 2018;38:1322–9.
Devarbhavi H. Acute liver failure induced by anti-infectious drugs: causes and management. Curr Hepatol Rep 2017;16:276–285.
Treeprasertsuk S, Huntrakul J, Ridtitid W, et al. The predictors of complications in patients with drug-induced liver injury caused by antimicrobial agents. Aliment Pharmacol Ther 2010;31:1200–1207.
Rathi C, Pipaliya N, Patel R, et al. Drug induced liver injury at a tertiary hospital in india: etiology, clinical features and predictors of mortality. Ann Hepatol 2017;16:442–450.
Sarda P, Sharma SK, Mohan A, et al. Role of acute viral hepatitis as a confounding factor in antituberculosis treatment induced hepatotoxicity. Indian J Med Res 2009;129:64–67.
Nahid P, Dorman SE, Alipanah N, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America clinical practice guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis 2016;63:e147–e195.
Udomsinprasert W, Chanhom N, Suvichapanich S, et al. Leukocyte telomere length as a diagnostic biomarker for anti-tuberculosis drug-induced liver injury. Sci Rep 2020;10:1–8.
Li Y, Ren Q, Wu D, et al. Combined 5‐hydroxymethylcytosine content of human leucocyte antigen‐B and human leucocyte antigen‐DQB1 as novel biomarker for anti‐tuberculosis drug‐induced liver injury. Basic Clin Pharmacol Toxicol 2020;127:234–240
Nicoletti P, Devarbhavi H, Goel A, et al. Genetic risk factors in drug-induced liver injury due to isoniazid-containing anti-tuberculosis drug regimens. Clin Pharmacol Ther 2020. https://doi.org/10.1002/cpt.2100. Online ahead of print.
Ormerod LP, Skinner C, Wales J. Hepatotoxicity of antituberculosis drugs. Thorax 1996;51:111–113.
Thompson NP, Caplin ME, Hamilton MI, et al. Anti-tuberculosis medication and the liver: dangers and recommendations in management. Eur Respir J 1995;8:1384–1348.
Rettenbacher MA, Baumgartner S, Eder-Ischia U, et al. Association between antipsychotic-induced elevation of liver enzymes and weight gain: a prospective study. J Clin Psychopharmacol 2006;26:500–503.
Bessone F, Dirchwolf M, Rodil MA, et al. Review article: drug-induced liver injury in the context of nonalcoholic fatty liver disease—a physiopathological and clinical integrated view. Aliment Pharmacol Ther 2018;48:892–913.
Tarantino G, Conca P, Basile V, et al. A prospective study of acute drug-induced liver injury in patients suffering from non-alcoholic fatty liver disease. Hepatol Res 2007;37:410–415.
Lammert C, Imler T, Teal E, et al. Patients with chronic liver disease suggestive of nonalcoholic fatty liver disease may be at higher risk for drug-induced liver injury. Clin Gastroenterol Hepatol 2019;17:2814–2015.
Sulkowski MS, Thomas DL, Mehta SH, et al. Hepatotoxicity associated with nevirapine or efavirenz-containing antiretroviral therapy: role of hepatitis C and B infections. Hepatology 2002;35:182–189.
Rutherford A, Davern T, Hay JE, et al. Influence of high body mass index on outcome in acute liver failure. Clin Gastroenterol Hepatol 2006;4:1544–1549.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Devarbhavi, H., Aithal, G., Treeprasertsuk, S. et al. Drug-induced liver injury: Asia Pacific Association of Study of Liver consensus guidelines. Hepatol Int 15, 258–282 (2021). https://doi.org/10.1007/s12072-021-10144-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10144-3