Abstract
In this modern era, when access to healthcare services is improved, and awareness among the general population is enhanced, the presentation of mere septal abscess of the nose as a fatal complication is less common. Due to various lockdown restrictions in the COVID-19 scenario and fear to contract an infection, patients are presenting late to the health care setting for proper management. We treated an 11-year old child of complicated nasal septal abscess who responded well to aspiration of pus and medical treatment. Our patient is a rare case report who progressed from vestibulitis to septal abscess and further leading to sinusitis, orbital, and intracranial complications.
Similar content being viewed by others
Introduction
In the post-antibiotic era, nasal septal abscess (NSA) is a rare pathology causing complications. Moreover, in the growing child, wholly or partially destroyed septal cartilage as a complication of abscess formation can hinder the normal midface development [1]. It is the immune-compromised patients in which rapid intracranial extension of NSA usually occurs [2]. However, we hereby report a pediatric immunocompetent case of NSA as sequelae of vestibulitis leading to sinusitis, and further progressing to facial cellulitis, pre-septal cellulitis, and meningitis.
Case Report
An 11 year old male child was admitted to the otorhinolaryngology and head and neck department of our institute with the chief complaint of high-grade fever, swelling over the nose, and eyelids for 4 days (Fig. 1). The patient also complained of pain in and around the nose and both eyes. There was no associated history of nasal discharge, nasal obstruction, mouth breathing, cough, difficulty in breathing, or any decreased sense of smell. According to patient’s father, there was an initial onset of nasal swelling for which oral medication was taken from some local practitioner only due to COVID-19 restrictions, but no relief of symptoms was obtained; instead, swelling worsened further and involved both eyes. There was no history of nasal trauma, dental infection, and any significant past medical, surgical, and family history.
When the child visited the hospital, he was alert, conscious, and oriented to time, place, and person with no difficulty in breathing. The temperature on arrival was 102 °F orally, oxygen saturation of 99%, heart rate of 100 beats/min, respiratory rate of 20 breaths/min, and blood pressure of 104/90 mm Hg. No external deformity of the nose was appreciated on local examination, but the swelling, erythema, and blackish crusts more on the right alar region and tip was observed. The nose was tender on palpation, and slight boggy swelling was noted on the anterior nasal septum on right side. Ophthalmology opinion revealed swelling and erythema of eyelids and periorbital region, without any chemosis or conjunctival hemorrhage and fundus glow was present bilaterally but at that time, the child was uncooperative for bedside visual acuity and extraocular movements examination due to pain. Later all cranial nerve examinations was found to be normal.
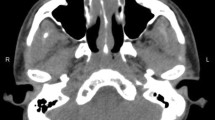
Due to this ongoing COVID-19 pandemic and patient presenting with fever, an immediate nasopharyngeal and oropharyngeal swab was also sent, which turned out to be negative. All routine blood investigations were done. The total leucocyte count was raised to 13,660cells/mm3 with a neutrophil differential count of 84%. The patient was sent for a contrast-enhanced computed tomography (CECT) Nose and paranasal sinuses (PNS) which was suggestive of a well defined oval hypodense collection with an average HU value of 25, measuring 24 × 21 × 15.5 mm in size with peripheral enhancement involving the anterior part of the septum (Fig. 2) along with marked fat stranding in subcutaneous tissue overlying the nose, nasion, and bilateral orbits. Moreover, mucosal thickening was seen in all the sinuses.
The diagnostic nasal endoscopy revealed swelling involving the anterior nasal septum on the right side only. The needle aspiration of about 2.5 ml pus was done which led to the resolution of septal swelling (Fig. 3) and was sent for culture sensitivity, which came out to be sterile because of ongoing antibiotic treatment. The child was started initially on intravenous ceftriaxone, metronidazole, paracetamol infusion, mupirocin local application, and oral ibuprofen.
After 4 h of admission, the child started developing features of meningismus such as headache, neck pain, projectile vomiting, photophobia, with already existing high-grade fever with no sign of altered sensorium. Then urgent MRI brain was done to rule out any intracranial complication. On a contrast MRI brain study, subtle meningeal enhancement was seen with meningitis suspicion (Fig. 4). There was no thrombus or filling defect in the cavernous sinus which ruled out its involvement. Overall findings were suggestive of NSA involving the cartilaginous part of the septum as sequelae of vestibulitis of the nose and mild to moderate acute pansinusitis with bilateral pre-septal cellulitis with suspicion of meningitis.
The pediatrics consultation was taken and was advised to shift to a pediatric intensive care unit (ICU) under the joint care of the otorhinolaryngology and pediatrics department for medical management. The empirical therapy of intravenous vancomycin (40 mg/kg/day), imipenem, mannitol, and fluconazole along with nasal oxy-xylometazoline drops was added. The child responded well to aspiration of pus and medical management and was discharged after full recovery in 14 days on oral antibiotic therapy for a week.
Discussion
NSA is defined as a collection of pus in the subperichondrial and subperiosteal plane of the septum. NSA occurs mostly in children with male predominance. The reason for this predominance could be explained that the mucoperichondrium and mucoperiosteum loosely adhere to the septum in children, and males are more involved in violent activities [3].
In about three-fourths of cases, the etiological agent is identified to be trauma followed by causes secondary to sinusitis, vestibulitis, dental pathologies with rare reporting of spontaneous cases [4]. Mostly NSA patients present with nasal obstruction with associated symptoms of pain, fever, malaise, headache, purulent nasal discharge, and delayed presentations can be cosmetic deformity of the nose such as saddle nose or any intracranial complication. According to the Korean case series, nasal obstruction is one of the initial, and nasal pain is the most common symptom reported in NSA [3]. The characteristic appearance of NSA on anterior rhinoscopy and diagnostic nasal endoscopy is septal swelling (bilateral > unilateral). The usual bilateral involvement can be credited to septal cartilage resorption as a consequence of ischemia and necrosis [1].
The most common cause of NSA is aerobic bacteria to be specific; Staphylococcus aureus accounts for the majority of cases in adults and Haemophilus influenza in the pediatric population [4]. In the literature, the complications of NSA are categorized into: local, systemic, orbital, and cranial [3]. In the present case, local complications of sinusitis, vestibulitis, facial cellulitis, orbital complication of pre-septal cellulitis, and cranial complications of meningitis were observed.
These types of cases can progress from NSA to necrotizing fascitis stage and cavernous sinus thrombosis, as reported by Swaminath et al., if the further delay in management occurs. The intracranial extension can be via the perineural sheath, lymphatics, and hematogenous route [5]. Even retrograde infection from sinusitis and orbital cellulitis to NSA has been evident in the literature. The infection can travel to and fro due to the valve-less nature of the facial venous system [6].
An appropriate and timely radiological investigation is required in NSA cases. CECT nose and PNS’s role is not only for diagnosis but also for ruling out any complication or the suspicion of rhinosinusitis, granulomatous diseases, sarcoma, or lymphoma in spontaneous cases [7]. It is to be noted that NSA has a characteristic appearance on CT examination as a cystic collection of fluid with thin rim enhancement involving the nasal septum [8]. The typical fat stranding is seen in facial cellulitis, but gas on radiography points towards the necrotizing fascitis stage [5]. MRI brain with contrast is undeniably beneficial in the preliminary investigations of suspicious intracranial extension and can avoid lethal complications.
Early diagnosis and immediate surgical intervention are necessary along-with parenteral antibiotic treatment. Simple needle aspiration has a role only for the diagnosis of an abscess and reducing pressure symptoms but is not sufficient for NSA management, and proper incision and drainage are required to prevent recollection. Apart from Killian`s incision, horizontal longitudinal or L shaped incision are other options [2]. The drainage of abscess bilaterally is required only if septal cartilage is intact, and pus is collected on both sides, but usually, partial destruction of cartilage is present to allow common cavity and drainage by single incision [9]. Bilateral nasal packing is required postoperatively for a minimum 48 h with the controversial role of Penrose drain. As few studies like Canty and Berkowitz [10] and Kwak et al. [3] reported no benefit of Penrose drain concerning to re-accumulation of fluid. But in our case, only the anterior nasal septum was involved on one side without septal cartilage destruction and simple aspiration gave good results without recurrence.
Conclusion
NSA is itself an infrequent pathology in today’s scenario and complicated NSA cases are rare. It should be taken into consideration that NSA can be atraumatic with no history of nasal obstruction, but a lack of prompt diagnosis can land up the patient in life-threatening complications. Due to the COVID-19 pandemic, people are apprehensive of reporting to a hospital because of the social stigma of contracting an infection, and further restriction of movement is making the situation worse.
References
Alshaikh N, Lo S (2011) Nasal septal abscess in children: from diagnosis to management and prevention. Int J Pediatr Otorhinolaryngol 75(6):737–744. https://doi.org/10.1016/j.ijporl.2011.03.010
Adnane C, Adouly T, Taali L et al (2015) Unusual Spontaneous Nasal Septal Abscess. J Case Rep Stud 3:302. https://doi.org/10.15744/2348-9820.3.302
Kwak KH, Lee J, Lim EJ, Park JH, Kim SH, Kim TH. Nasal Septal Abscess: Clinical Analysis of 6 Cases. Journal of Clinical Otolaryngology. 2015; 26:213-218. https://doi.org/10.35420/jcohns.2015.26.2.213
Hyo Y, Fukushima H, Harada T, Hara H (2018) Nasal septal abscess caused by anaerobic bacteria of oral flora. Auris Nasus Larynx 46:147–150. https://doi.org/10.1016/j.anl.2018.05.014
Swaminath D, Narayanan R, Orellana-Barrios MA, Temple B (2014) Necrotizing fasciitis of the nose complicated with cavernous sinus thrombosis. Case Rep Infect Dis. https://doi.org/10.1155/2014/914042
Fatima SN, Sarwar F, Khan (2018) Nasal septal abscess as a sequela of orbital cellulitis: an uncommon presentation. SAGE Open Med Case Rep 6:2050313X18778726. https://doi.org/10.1177/2050313X18778726
Nwosu JN, Nnadede PC (2015) Nasalseptal hematoma/abscess: management and outcome in a tertiary hospital of a developing country. Patient Preference Adher 9:1017–1021. https://doi.org/10.2147/PPA.S85184
Debnam JM, Gillenwater AM, Ginsberg LE (2007) Nasal septal abscess in patients with immunosuppression. Am J Neuroradiol 28:1878–1879. https://doi.org/10.3174/ajnr.a0708
Shapiro RS (1978) Nasal septal abscess. CMA 119(11):1321–1323
Canty PA, Berkowitz RG (1996) Hematoma and abscess of the nasal septum in children. Arch Otolaryngol Head Neck Surg 122(12):1373–1376. https://doi.org/10.1001/archotol.1996.01890240079017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The study has not received funding from any organization or institution and does not involve any potential conflict of interest (financial and non-financial).
Ethical Approval
Procedure performed in the study was in accordance with the ethical standards of the institution and with the 1964 Helsinki declaration and its later amendments.
Informed Consent
Informed consent was obtained from patient’s guardian in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maan, A.S., Kaur, G., Arora, R. et al. An Unusual Case of a Pediatric Nasal Septal Abscess with Life-Threatening Complications in COVID-19 Pandemic. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 2795–2798 (2022). https://doi.org/10.1007/s12070-020-02264-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02264-3