Abstract
Objectives
Bronchiectasis continues to be a major cause of morbidity and mortality in developing countries. The purpose of this study is to present our experience in surgical treatment of patients with bronchiectasis during a 5-year period and their early- and late-term results.
Methods
Records of 48 patients who underwent surgical resection for bronchiectasis from April 2009 through March 2014 at Cardiothoracic Surgery Department of Gauhati Medical College Hospital were reviewed. Variables analyzed were age, sex, symptoms, etiology, extent, indication and type of operation, mortality, morbidity, and the result of surgical therapy.
Results
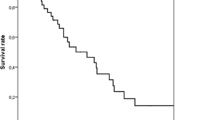
There were 42 (87.5 %) male and 6 (12.5 %) female patients with an average age of 33.7 years (range, 19–47 years). The indications for surgery were failure of conservative treatment in 21 patients (43.75 %), recurrent hemoptysis in 20 (41.66 %), destroyed lung in 5 (10.42 %), and endobronchial obstruction in 2 (4.17 %). Thirty-four patients (70.83 %) had complete resection with lobectomy, pneumonectomy, or bilateral lobectomy, and 14 (29.17 %) had incomplete resection with segmentectomy or lobectomy with segmentectomy. There were no perioperative deaths; complications occurred in 10 patients with a morbidity rate of 20.83 %. Follow-up data were obtained for 44 (91.66 %) of the patients for a mean of 9 months (range, 4 months to 3.5 years). The symptoms disappeared in 21 patients (47.43 %) and improved in 17 (38.64 %). Improvement of symptoms was observed more significantly in the patients undergoing complete resection.
Conclusions
Surgical resection for bronchiectasis obtains satisfactory long-term results with acceptable morbidity and mortality rates. When possible, complete resection should be performed.
Similar content being viewed by others
References
Balkanli K, Genç O, Dakak M, et al. Surgical management of bronchiectasis: analysis and short-term results in 238 patients. Eur J Cardiothorac Surg. 2003;24:699–702.
Ashour M, Al-Kattan KM, Jain SK, et al. Surgery for unilateral bronchiectasis: results and prognostic factors. Tuber Lung Dis. 1996;77:168–72.
Agasthian T, Deschamps C, Trastek VF, Allen MS, Pairolero PC. Surgical management of bronchiectasis. Ann Thorac Surg. 1996;62:976–80.
De Dominicis F, Andréjak C, Monconduit J, Merlusca G, Berna P. Surgery for bronchiectasis. Rev Pneumol Clin. 2012;68:91–100.
Mazières J, Murris M, Didier A, et al. Limited operation for severe multisegmental bilateral bronchiectasis. Ann Thorac Surg. 2003;75:382–7.
King PT, Holdsworth SR, Freezer NJ, Villanueva E, Holmes PW. Characterisation of the onset and presenting clinical features of adult bronchiectasis. Respir Med. 2006;100:2183–9.
Nicotra MB. Bronchiectasis. Semin Respir Infect. 1994;9:31–40.
Eren S, Esme H, Avci A. Risk factors affecting outcome and morbidity in the surgical management of bronchiectasis. J Thorac Cardiovasc Surg. 2007;134:392–8.
Fujimoto T, Hillejan L, Stamatis G. Current strategy for surgical management of bronchiectasis. Ann Thorac Surg. 2001;72:1711–5.
Stephen T, Thankachen R, Madhu AP, Neelakantan N, Shukla V, Korula RJ. Surgical results in bronchiectasis: analysis of 149 patients. Asian Cardiovasc Thorac Ann. 2007;15:290–6.
Javidan-Nejad C, Bhalla S. Bronchiectasis. Radiol Clin N Am. 2009;47:289–306.
Karakoc GB, Yilmaz M, Altintas DU, Kendirli SG. Bronchiectasis: still a problem. Pediatr Pulmonol. 2001;32:175–8.
Nicotra MB, Rivera M, Dale AM, Sheherd R, Carter R. Clinical, pathophysiologic, and microbiologic characterization of bronchiectasis in an aging cohort. Chest. 1995;108:955–61.
Kang EY, Miller RR, Muller NL. Bronchiectasis: comparison of preoperative thin-section CT and pathologic findings in resected specimens. Radiology. 1995;195:649–54.
Diederich S, Roos N, Thomas M, Peters PE. Diagnostic imaging in bronchiectases. Value of CT and HRCT. Radiologe. 1996;36:550–9.
Kutlay H, Cangir AK, Enon S, et al. Surgical treatment in bronchiectasis: analysis of 166 patients. Eur J Cardiothorac Surg. 2002;21:634–7.
Etiene T, Spiliopoulos A, Megevand R. Bronchiectasis: indication and timing for surgery. Ann Chir. 1993;47:729–35.
Giovannetti R, Alifano M, Stefani A, et al. Surgical treatment of bronchiectasis: early and long-term results. Interact Cardiovasc Thorac Surg. 2008;7:609–12.
Halezeroglu S, Keles M, Uysal A, et al. Factors affecting postoperative morbidity and mortality in destroyed lung. Ann Thorac Surg. 1997;64:1635–8.
Gursoy S, Ozturk AA, Ucveti A, Erbay AE. Surgical management of bronchiectasis: the indications and outcomes. Surg Today. 2010;40:26–30.
Acknowledgments
The authors sincerely thank our MCh students Dr. Ruprekha Das and Dr. Shaleen Prasad for their help in collecting the patient records and in preparation of this manuscript.
Conflict of interest
Authors declare that they have no competing interests.
Disclaimers
None.
Compliance with ethical standards
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study. This article does not contain any study with animals performed by any of the authors.
Funding and source of support
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baruah, N., Saikia, P.P., Goswami, A. et al. Surgical management of bronchiectasis: a 5-year review of a single center’s experience. Indian J Thorac Cardiovasc Surg 31, 213–217 (2015). https://doi.org/10.1007/s12055-015-0381-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-015-0381-6