Abstract
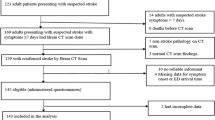
Timely thrombolytic treatment is paramount after acute ischemic stroke (AIS); however, a large proportion of patients experience substantial delays in presentation to hospital. This study evaluates the prevalence and risk factors in pre-hospital delays after AIS in central urban China. AIS patients from 66 hospitals in 13 major cities across Hubei Province, between October 1, 2014 and January 31, 2015 were interviewed and their medical records were reviewed to identify those who suffered pre-hospital delays. Bivariate and multivariate analyses were undertaken to determine the prevalence rates and the risk factors associated with pre-hospital delays. A total of 1835 patients were included in the analysis, with 69.3 % patients reportedly arrived at hospital 3 or more hours after onset and 55.3 % patients arrived 6 or more hours after onset. Factors associated with increased pre-hospital delays for 3 or more hours were as follows: patient had a history of stroke (odds ratio (OR), 1.319, P = 0.028), onset location was at home (OR, 1.573, P = 0.002), and patients rather than someone else noticed the symptom onset first (OR, 1.711; P < 0.001). In contrast, knowing someone who had suffered a stroke, considering any kind of the symptoms as severe, transferring from a community-based hospital factors, calling emergency number (120), and shorter distance from the onset place to the first hospital were independently associated with decreased pre-hospital delays. These findings indicate that pre-hospital delays after AIS are common in urban central China, and future intervention programs should be focused on public awareness of stroke and appropriate response.

Similar content being viewed by others
References
WHO (2015) Global status report on noncommunicable diseases 2014. Jan 19
Jauch EC, Stettler B (2015) Ischemic stroke. Available at: http://emedicine.medscape.com/article/1916852-overview. Accessed Jan 20
Wardlaw JM, Murray V, Berge E, del Zoppo GJ (2014) Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev 7, CD000213
Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329
Wahlgren N, Ahmed N, Davalos A, Hacke W, Millan M, Muir K, Roine RO, Toni D et al (2008) Thrombolysis with alteplase 3–4.5 h after acute ischaemic stroke (sits-istr): an observational study. Lancet 372:1303–1309
Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, Brott T, Frankel M et al (2004) Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-pa stroke trials. Lancet 363:768–774
Jin H, Zhu S, Wei JW, Wang J, Liu M, Wu Y, Wong LK, Cheng Y et al (2012) Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke 43:362–370
Lin CS, Tsai J, Woo P, Chang H (1999) Prehospital delay and emergency department management of ischemic stroke patients in taiwan, r.O.C. Prehosp Emerg Care 3:194–200
Srivastava AK, Prasad K (2001) A study of factors delaying hospital arrival of patients with acute stroke. Neurol India 49:272–276
Wang Y, Liao X, Zhao X, Wang DZ, Wang C, Nguyen-Huynh MN, Zhou Y, Liu L et al (2011) Using recombinant tissue plasminogen activator to treat acute ischemic stroke in china: analysis of the results from the chinese national stroke registry (cnsr). Stroke 42:1658–1664
Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, Kong LZ (2007) Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol 6:456–464
Fang J, Yan W, Jiang GX, Li W, Cheng Q (2011) Time interval between stroke onset and hospital arrival in acute ischemic stroke patients in shanghai, China. Clin Neurol Neurosurg 113:85–88
Chang KC, Tseng MC, Tan TY (2004) Prehospital delay after acute stroke in Kaohsiung, Taiwan. Stroke 35:700–704
Wester P, Radberg J, Lundgren B, Peltonen M (1999) Factors associated with delayed admission to hospital and in-hospital delays in acute stroke and TIA: a prospective, multicenter study. Seek- medical-attention-in-time study group. Stroke 30:40–48
Chen CH, Huang P, Yang YH, Liu CK, Lin TJ, Lin RT (2007) Pre-hospital and in-hospital delays after onset of acute ischemic stroke: a hospital-based study in southern Taiwan. Kaohsiung J Med Sci 23:552–559
Evenson KR, Foraker RE, Morris DL, Rosamond WD (2009) A comprehensive review of prehospital and in-hospital delay times in acute stroke care. Int J Stroke 4:187–199
Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS et al (2006) Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation 114:168–182
Williams LS, Bruno A, Rouch D, Marriott DJ (1997) Stroke patients’ knowledge of stroke. Influence on time to presentation. Stroke 28:912–915
Mandelzweig L, Goldbourt U, Boyko V, Tanne D (2006) Perceptual, social, and behavioral factors associated with delays in seeking medical care in patients with symptoms of acute stroke. Stroke 37:1248–1253
Geffner D, Soriano C, Perez T, Vilar C, Rodriguez D (2012) Delay in seeking treatment by patients with stroke: who decides, where they go, and how long it takes. Clin Neurol Neurosurg 114:21–25
Pandian JD, Kalra G, Jaison A, Deepak SS, Shamsher S, Padala S, Singh Y, Abraham G (2006) Factors delaying admission to a hospital-based stroke unit in india. J Stroke Cerebrovasc Dis 15:81–87
Lacy CR, Suh DC, Bueno M, Kostis JB (2001) Delay in presentation and evaluation for acute stroke: stroke time registry for outcomes knowledge and epidemiology (s.T.R.O.K.E.). Stroke 32:63–69
Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S (2000) Prehospital and emergency department delays after acute stroke: the genentech stroke presentation survey. Stroke 31:2585–2590
Rossnagel K, Jungehulsing GJ, Nolte CH, Muller-Nordhorn J, Roll S, Wegscheider K, Villringer A, Willich SN (2004) Out-of-hospital delays in patients with acute stroke. Ann Emerg Med 44:476–483
Maestroni A, Mandelli C, Manganaro D, Zecca B, Rossi P, Monzani V, Torgano G (2008) Factors influencing delay in presentation for acute stroke in an emergency department in Milan, Italy. Emerg Med J 25:340–345
Kim YS, Park SS, Bae HJ, Cho AH, Cho YJ, Han MK, Heo JH, Kang K et al (2011) Stroke awareness decreases prehospital delay after acute ischemic stroke in Korea. BMC Neurol 11:2
Menon SC, Pandey DK, Morgenstern LB (1998) Critical factors determining access to acute stroke care. Neurology 51:427–432
Rosamond WD, Gorton RA, Hinn AR, Hohenhaus SM, Morris DL (1998) Rapid response to stroke symptoms: the delay in accessing stroke healthcare (dash) study. Acad Emerg Med 5:45–51
Nedeltchev K, Arnold M, Brekenfeld C, Isenegger J, Remonda L, Schroth G, Mattle HP (2003) Pre- and in-hospital delays from stroke onset to intra-arterial thrombolysis. Stroke 34:1230–1234
Caruso D, Perez Akly M, Costantini PD, Fridman S, Esnaola MM (2015) Do elderly patients call 911 when presented with clinical scenarios suggestive of acute stroke? A cross-sectional study. Cerebrovasc Dis 39:87–93
Malek AM, Adams RJ, Debenham E, Boan AD, Kazley AS, Hyacinth HI, Voeks JH, Lackland DT (2014) Patient awareness and perception of stroke symptoms and the use of 911. J Stroke Cerebrovasc Dis 23:2362–2371
Wein TH, Staub L, Felberg R, Hickenbottom SL, Chan W, Grotta JC, Demchuk AM, Groff J et al (2000) Activation of emergency medical services for acute stroke in a nonurban population: The T.L.L. Temple foundation stroke project. Stroke 31:1925–1928
George MG, Tong X, McGruder H, Yoon P, Rosamond W, Winquist A, Hinchey J, Wall HK et al (2009) Paul coverdell national acute stroke registry surveillance—four states, 2005–2007. MMWR Surveill Summ 58:1–23
Mosley I, Nicol M, Donnan G, Patrick I, Dewey H (2007) Stroke symptoms and the decision to call for an ambulance. Stroke 38:361–366
(2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis, 25:457–507
Kleindorfer DO, Lindsell CJ, Broderick JP, Flaherty ML, Woo D, Ewing I, Schmit P, Moomaw C et al (2006) Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: do poorer patients have longer delays from 911 call to the emergency department? Stroke 37:1508–1513
Turan TN, Hertzberg V, Weiss P, McClellan W, Presley R, Krompf K, Karp H, Frankel MR (2005) Clinical characteristics of patients with early hospital arrival after stroke symptom onset. J Stroke Cerebrovasc Dis 14:272–277
Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS et al (2007) Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. J Cardiovasc Nurs 22:326–343
Zerwic J, Hwang SY, Tucco L (2007) Interpretation of symptoms and delay in seeking treatment by patients who have had a stroke: exploratory study. Heart Lung 36:25–34
Gargano JW, Wehner S, Reeves MJ (2011) Presenting symptoms and onset-to-arrival time in patients with acute stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 20:494–502
Smith MA, Doliszny KM, Shahar E, McGovern PG, Arnett DK, Luepker RV (1998) Delayed hospital arrival for acute stroke: the Minnesota stroke survey. Ann Intern Med 129:190–196
Acknowledgments
The authors thank the Stroke Quality Control Center of Hubei Province and the Preventive Medicine Association of Hubei Province for supporting. The authors also thank all study participants who have been involved and contributed to the procedure of data collection.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Sources of Funding
This project was funded by the Stroke Quality Control Center of Hubei Province and the Preventive Medicine Association of Hubei Province. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional information
Novelty and Significance
1. What is new?
• The current large, cross-sectional study of 66 hospitals located in 13 major cities indicates that pre-hospital delays for AIS patients are relatively common in Hubei province, central urban China.
• Multivariate analyses show that a multitude of factors influence the delays. Patients with previous stroke, patients’ symptoms occurred at home, and patients rather than someone else noticed the symptoms first had a higher risk of delays.
2. What is relevant?
• Based on the risk factors, intervention programs, which emphasize comprehensive education of awareness of stroke and appropriate response (calling emergency number), should be implemented and critically evaluated.
3. Summary
Pre-hospital delays after AIS are common in urban central China, and future intervention programs should be focused on public awareness of stroke and appropriate response.
Zuxun Lu (zuxunlu@yahoo.com) is the first corresponding author.
Rights and permissions
About this article
Cite this article
Zhou, Y., Yang, T., Gong, Y. et al. Pre-hospital Delay after Acute Ischemic Stroke in Central Urban China: Prevalence and Risk Factors. Mol Neurobiol 54, 3007–3016 (2017). https://doi.org/10.1007/s12035-016-9750-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-9750-4