Abstract
Background
The aim of this study was to compare the therapeutic effects of non-navigated freehand minimally invasive aspiration and conservative medical care in patients with deep supratentorial intracerebral hemorrhage (ICH).
Methods
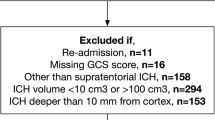
We analyzed data from a prospective multicenter cohort study. Propensity score matching was performed to adjust for possible confounding factors. A total of 122 patients with first-onset deep supratentorial ICH with a volume ≥ 20 ml were enrolled. All patients were followed up at 30 days, 90 days, and 1 year. The mortality rate, functional outcomes, complications, and treatment costs were compared between the two groups.
Results
After propensity score matching, 122 patients with a mean age of 56.0 years were included, 77.9% of whom were male. The median ICH volumes were 45.5 ml in the surgery group and 48.0 ml in the conservative group. The mortality rate at 30 days was significantly lower in the surgery group than in the conservative group (P = 0.0127). There were no significant differences in functional outcomes at the 90-day and 1-year follow-ups between the two groups (P > 0.05). There was no significant difference in complications, including recurrent bleeding (6.6% vs. 4.9%), pulmonary infection (57.4% vs. 41.0%), deep venous thrombosis (9.8% vs. 11.5%), heart failure (1.6% vs. 6.6%), and cerebral infarction (4.9% vs. 3.3%), between the two groups.
Discussion
For deep supratentorial ICH, non-navigated freehand minimally invasive aspiration was safe and reduced short-term mortality but did not effectively improve long-term functional outcomes.


Similar content being viewed by others
Data Availability
Research data are not shared because of ethical restrictions.
References
Sheth KN. Spontaneous intracerebral hemorrhage. N Engl J Med. 2022;387(17):1589–96.
Greenberg SM, Ziai WC, Cordonnier C, Dowlatshahi D, Francis B, Goldstein JN, et al. Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53(7):e282–361.
Hanley DF, Thompson RE, Muschelli J, Rosenblum M, McBee N, Lane K, et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol. 2016;15(12):1228–37.
Hanley DF, Thompson RE, Rosenblum M, Yenokyan G, Lane K, McBee N, et al. Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet. 2019;393(10175):1021–32.
Ironside N, Chen CJ, Dreyer V, Christophe B, Buell TJ, Connolly ES. Location-specific differences in hematoma volume predict outcomes in patients with spontaneous intracerebral hemorrhage. Int J Stroke. 2020;15(1):90–102.
de Oliveira Manoel AL. Surgery for spontaneous intracerebral hemorrhage. Crit Care. 2020;24(1):45.
Pan J, Chartrain AG, Scaggiante J, Spiotta AM, Tang Z, Wang W, et al. A compendium of modern minimally invasive intracerebral hemorrhage evacuation techniques. Oper Neurosurg (Hagerstown). 2020;18(6):710–20.
Zhao Z, Xiao J, Wang J, Meng X, Li C, Xin T, et al. Individualized CT image-guided free-hand catheter technique: a new and reliable method for minimally invasive evacuation of basal ganglia hematoma. Front Neurosci. 2022;16: 947282.
Wang D, Wang W, Wang A, Zhao X. Association of severity and prognosis with elevated homocysteine levels in patients with intracerebral hemorrhage. Front Neurol. 2020;11: 571585.
Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(7):2032–60.
Gong C, Boulis N, Qian J, Turner DE, Hoff JT, Keep RF. Intracerebral hemorrhage-induced neuronal death. Neurosurgery. 2001;48(4) 875–883. https://doi.org/10.1097/00006123-200104000-00037
Mould WA, Carhuapoma JR, Muschelli J, Lane K, Morgan TC, McBee NA, et al. Minimally invasive surgery plus recombinant tissue-type plasminogen activator for intracerebral hemorrhage evacuation decreases perihematomal edema. Stroke. 2013;44(3):627–34.
Scaggiante J, Zhang X, Mocco J, Kellner CP. Minimally invasive surgery for intracerebral hemorrhage. Stroke. 2018;49(11):2612–20.
Deng C, Ji Y, Song W, Bi J. Clinical effect of minimally invasive aspiration and drainage of intracranial hematoma in the treatment of cerebral hemorrhage. Pak J Med Sci. 2022;38(1):95–9.
Polster SP, Carrion-Penagos J, Lyne SB, Gregson BA, Cao Y, Thompson RE, et al. Intracerebral hemorrhage volume reduction and timing of intervention versus functional benefit and survival in the MISTIE III and STICH trials. Neurosurgery. 2021;88(5):961–70.
Xiao K, Chu H, Li G, Chen H, Zhong Y, Dong Q, et al. Reduction of midline shift and short-term mortality following minimal invasive surgery for spontaneous supratentorial intracerebral hemorrhage: a retrospective and case-control series. World Neurosurg. 2022;162:e645–51.
Sirh S, Park HR. Optimal surgical timing of aspiration for spontaneous supratentorial intracerebral hemorrhage. J Cerebrovasc Endovasc Neurosurg. 2018;20(2):96–105.
Acknowledgements
We would like to that the cooperation of the hospitals that took part in our program and for helping collect the information of patients.
Funding
This work was supported by the National Key R&D Program of China (2022ZD0118005), the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2019-I2M-5–029), Beijing Municipal Committee of Science and Technology (Z201100005620010), Beijing Hospitals Authority Innovation Studio of Young Staff Funding Support (202112), and the Ministry of Finance of the People’s Republic of China (issued by Finance and Social Security [2015] Document No. 82 [2016], Document No. 50 [2017], Document No. 72 [2018], Document No. 48 [2019], Document No. 77 [2020], Document No. 75 [2021], and Document No. 84, Ministry of Finance).
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafted the article or revised it critically for important intellectual content; and approved the final version to be published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics Approval/Informed Consent
This study was approved by the Institutional Review Board of Beijing Tiantan Hospital. Written informed consent was obtained from all participants or their relatives.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, J., Wang, D., Wang, A. et al. Long-Term Outcomes Following Freehand Minimally Invasive Aspiration for Deep Supratentorial Intracerebral Hemorrhage: A Multicenter Cohort Study. Neurocrit Care (2023). https://doi.org/10.1007/s12028-023-01869-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-023-01869-0