Abstract
Background
Following non-traumatic subarachnoid hemorrhage (SAH), in-hospital delayed cerebral ischemia is predicted by two chief events on continuous EEG (cEEG): new or worsening epileptiform abnormalities (EAs) and deterioration of cEEG background frequencies. We evaluated the association between longitudinal outcomes and these cEEG biomarkers. We additionally evaluated the association between longitudinal outcomes and other in-hospital complications.
Methods
Patients with nontraumatic SAH undergoing ≥ 3 days of cEEG monitoring were enrolled in a prospective study evaluating longitudinal outcomes. Modified Rankin Scale (mRS) was assessed at discharge, and at 3- and 6-month follow-up time points. Adjusting for baseline severity in a cumulative proportional odds model, we modeled the mRS ordinally and measured the association between mRS and two forms of in-hospital cEEG deterioration: (1) cEEG evidence of new or worsening epileptiform abnormalities and (2) cEEG evidence of new background deterioration. We compared the magnitude of these associations at each time point with the association between mRS and other in-hospital complications: (1) delayed cerebral ischemia (DCI), (2) hospital-acquired infections (HAI), and (3) hydrocephalus. In a secondary analysis, we employed a linear mixed effects model to examine the association of mRS over time (dichotomized as 0–3 vs. 4–6) with both biomarkers of cEEG deterioration and with other in-hospital complications.
Results
In total, 175 mRS assessments were performed in 59 patients. New or worsening EAs developed in 23 (39%) patients, and new background deterioration developed in 24 (41%). Among cEEG biomarkers, new or worsening EAs were independently associated with mRS at discharge, 3, and 6 months, respectively (adjusted cumulative proportional odds 4.99, 95% CI 1.60–15.6; 3.28, 95% CI 1.14–9.5; and 2.71, 95% CI 0.95–7.76), but cEEG background deterioration lacked an association. Among hospital complications, DCI was associated with discharge, 3-, and 6-month outcomes (adjusted cumulative proportional odds 4.75, 95% CI 1.64–13.8; 3.4; 95% CI 1.24–9.01; and 2.45, 95% CI 0.94–6.6), but HAI and hydrocephalus lacked an association. The mixed effects model demonstrated that these associations were sustained over longitudinal assessments without an interaction with time.
Conclusion
Although new or worsening EAs and cEEG background deterioration have both been shown to predict DCI, only new or worsening EAs are associated with a sustained impairment in functional outcome. This novel finding raises the potential for identifying therapeutic targets that may also influence outcomes.
Similar content being viewed by others
Introduction
Clinical outcome after spontaneous subarachnoid hemorrhage (SAH) is influenced by various factors, including baseline clinical severity [1, 2] and subsequent secondary brain injury attributed to delayed cerebral ischemia (DCI). Prior studies have shown specific continuous electroencephalography (cEEG) findings to be predictive of impending DCI, such as new or worsening burden of epileptiform abnormalities (EAs) [3,4,5,6], and measures of cEEG background deterioration (BD), including new focal slowing, loss of alpha power, or loss of alpha variability [7, 8]
In studies of multimodal physiology, these cEEG abnormalities have been observed in association with cerebral hypermetabolism leading to metabolic crisis [9,10,11,12], or cortical spreading depolarizations [10, 13,14,15,16], suggesting these biomarkers may represent a modifiable target for preventing DCI and improving neurologic outcomes. It is not known, however, if new or worsening EAs and BD have a durable influence on functional outcomes or represent more transient phenomena.
Accordingly, we sought to determine whether these DCI-linked cEEG biomarkers predict functional outcomes in order to identify whether pathologic EEG patterns may serve as a possible target for future treatment interventions. In doing so, we evaluated the association of cEEG biomarkers of DCI with longitudinal functional outcome, ascertained by the modified Rankin Scale (mRS) at discharge, 3-, and 6-month follow-up time points. We subsequently compared how these associations compared to the relationship between functional outcomes and other in-hospital complications, including hospital-acquired infections (HAI), hydrocephalus, and DCI itself.
Methods
Patient cohort and study design
In this prospective observational cohort study, we utilized the mRS to perform serial assessments of functional outcome using the mRS at discharge, 3, and 6 months following hospital admission under a protocol approved by our institutional review board. We examined the association between longitudinal mRS and two cEEG biomarkers: (1) new or worsening EAs and (2) new BD on cEEG. We additionally examined the association of functional outcome with three in-hospital complications: (1) DCI (2) hospital-acquired infections (HAI), and 3) hydrocephalus. We followed standards of the Strengthening the Reporting of Observational Studies in Epidemiology guidelines (Supplementary Table 1) [17].
Enrollment criteria included: (1) nontraumatic SAH requiring admission to an intensive care unit, (2) ≥ 18 years of age, (3) clinically ordered cEEG for ischemia monitoring performed for at least 72 h according to our institutional guideline, and (4) an mRS outcome assessment performed in person or by phone longitudinally at discharge, and 3 and 6 months following admission. Our institutional guideline [6, 18] recommends cEEG monitoring for all SAH patients with either high clinical grade (Hunt and Hess Grade (HH) 4–5) or high radiologic grade (modified Fisher Scale (mFS) score 3–4). We excluded patients with arteriovenous malformations as well as those who did not have an mRS assessment performed at discharge and 3 months.
Data collection
We documented relevant clinical and demographic variables from patient electronic health records. Hospital complications, including hydrocephalus, aneurysmal rebleeding, and hospital-acquired infections, were evaluated using a combination of chart review and prospective interviews with treating clinicians, Due to sample size constraints, we binarized the presence vs. absence of any HAI during ICU admission. HAI events included pneumonia, urinary tract infections, sepsis, or Clostridium difficile (C. difficile) which were defined in accordance with CDC guidance [19,20,21,22]. Patients were considered positive for presence of HAI if they had at least one of the aforementioned types of infections during their hospitalization. Hydrocephalus and aneurysmal rebleed were ascertained clinically by the treating team and documented in the medical record. We derived the APACHE II physiologic sub-scores from APACHE II scores ascertained from information encoded in the patient’s medical record. To calculate the APACHE II physiologic sub-score, we subtracted the patient’s initial GCS from the maximum possible GCS (15) and then took the difference between that value and the compositive APACHE II score.
Continuous EEG recordings were acquired in accordance with the International 10–20 system. Twice-daily clinical EEG reports were generated and reviewed by an outcomes-blinded neurophysiologist with certification in the American Clinical Neurophysiology Society (ACNS) EEG terminology exam. New or worsening EAs were defined as an increase in duration of interictal epileptiform discharges, lateralized rhythmic delta activity (LRDA), lateralized periodic discharges (LPD), or generalized periodic discharges (GPD), defined according to the 2012 Standardized American Clinical Neurophysiology Society (ACNS) ICU EEG terminology [23]. For an increase in EAs, the alarm criterion of a “clear and persistent worsening or new emergence” was defined as appearance of a pattern absent in prior epochs (new emergence), or increase in the ACNS-defined prevalence of the pattern, for example, from “occasional” LPDs (1–9% of an epoch) to “frequent” (10–49% of an epoch) [6]
New background deterioration was defined as decreasing Alpha Delta Ratio (ADR), Relative Alpha Variability (RAV) or worsening focal slowing, consistent with previous reporting [6, 18]. Patients received anti-seizure prophylaxis until the aneurysm was secured unless the clinical team made a decision to continue treatment for a separate clinical indication.
To assess for potential referral bias, we calculated the median age, HH and mFS of SAH patients admitted during the study period who had at least 3 days of cEEG monitoring but did not undergo the prospective functional outcome assessments at the time points of interest. Additionally, we retrospectively ascertained discharge mRS from the medical records of patients not included in our cohort to determine whether there were significantly different discharge outcomes for those who were versus those who were not included in our cohort.
The occurrence of DCI was ascertained prospectively as a new focal event of neurologic deterioration lasting 2 h or more, a new decrease in Glasgow Coma Scale (GCS) score of at least 2 points lasting at least 2 h, or a new radiologic infarction, unrelated to a recent procedure, according to methods described previously [6, 18]. These methods specify that DCI due to neurologic deterioration alone can only be documented in the absence of specific exclusion criteria (e.g., hydrocephalus, escalation of sedation, infection) which may result in non-ischemic neurologic deterioration. In addition, DCI due to radiologic infarction could only be documented when a peri-procedural infarct was excluded. These criteria were applied, and DCI was adjudicated by consensus by three board-certified neurologists [6, 18].
To minimize bias, continuous EEG exposures of interest were ascertained prior to outcomes, and outcomes were assessed by examiners without knowledge of the cEEG exposures of interest.
Statistical analysis
In a univariate analysis, we examined which of the following features were associated with discharge, 3-, and 6-month mRS scores: age, gender, HH grade, mFS score, DCI during admission, HAI during admission, and the two cEEG biomarkers: (1) new or worsening EAs, (2) new BD. In the univariate analysis, mRS was binarized (0–3 vs. 4–6). A Fisher’s Exact test was utilized for categorical variables and Wilcoxon Rank sum statistics for ordinal data; p values were reported with 95% confidence intervals and two-tailed significance testing except for the association of DCI with functional outcome, which was assessed using a one-tailed test due to its accepted association with poor functional outcome [24]. Admission demographic, clinical, and radiologic features significantly associated (p ≤ 0.15) with subsequent development of EAs, BD, or discharge, 3-, or 6-month mRS in the univariate analysis were included as covariates in further multivariate models.
Our pre-specified primary outcome was the independent association between functional outcome (ordinal mRS) at discharge, 3, and 6 months and cEEG biomarkers of neurologic deterioration, specifically (1) new or worsening EAs and (2) worsening BD, using a cumulative proportional odds (CPO) ordinal logistic regression model as a shift analysis. The CPO model was subsequently repeated at each time point with the inclusion of baseline risk factors: age, HH, and mFS, which were selected using features in the univariate analysis which demonstrated a potential association with discharge outcome. We did not adjust for DCI in evaluating the association of new or worsening EAs and BD because the very strong association of these cEEG biomarkers with subsequent DCI (OR > 100) suggests that DCI, as an illness-defining in-hospital event, is likely to be an intermediate between cEEG activity and outcome rather than a confounder [6]. In a post hoc analysis, we analyzed the association between new or worsening EAs and mRS at each time point in a CPO model accounting for the APACHE II physiologic sub-score.
In a secondary analysis, the CPO model was then used to assess the relationship between DCI and HAI with ordinal mRS at discharge, 3 months, and 6 months following the same methodology described above. These individual CPO models were each fit with ascending cutoffs such that the first cutoff compared mRS = 0 with mRS ≥ 1, the second cutoff compared 0 and 1 combined with mRS ≥ 2, the third cutoff compared 0, 1 and 2 combined with mRS ≥ 3, and so on. The SAS score test was utilized to pre-test the assumption of approximate equality of proportional odds of new or worsening EAs or worsening background deterioration versus mRS across cutoffs. We specified that if the assumption was not upheld, a Partial Proportional Odds (PPO) model be run to investigate possible differential odds ratios across cutoffs.
To explore for a potential interaction of time with new or worsening EAs, we constructed a linear mixed effects model, in which mRS was treated as a continuous linear scale. We pre-specified the results of the CPO model as the primary outcome rather than the linear mixed effects model given that mRS is an ordinal scale. However, the linear mixed effects model permitted the assessment of interactions and the potential for improved statistical power by including all longitudinal outcomes in one analysis. As such, it was constructed with the following covariates: (1) new or worsening EAs, (2) time of mRS assessment, and (3) an interaction term between time and new or worsening EAs. In a sensitivity analysis, we also computed models adding age, admission HH score, mFS, or a composite risk score [6, 25] to control for admission clinical severity. In a post hoc analysis, we included the APACHE II physiologic sub-score in a linear mixed effects model assessing the association between new or worsening EAs with outcomes over time.
Post hoc analysis of changes in anti-seizure medication
In a post hoc analysis of patients with new or worsening EAs, we assessed the association of changes in anti-seizure medications (ASM) with outcome. ASM changes were documented retrospectively from the medical record. Discharge ASM was ascertained from the discharge summary. ASM increases or decreases were documented if dosage or infusion rates changed by at least 50% [6]. Increases in ASM were also documented if the frequency of administration was increased.
Results
A total of 175 mRS assessments were performed in 59 patients who were admitted over a 3-year study period and met the enrollment criteria (Fig. 1). Within the study cohort, 43 (73%) patients were female and the median age was 57 years (IQR 49–65). Additional clinical and demographic features are summarized in Table 1, including patients with and without the candidate exposure.
New or worsening EAs and new BD were detected in 35 patients (59%): 23 (39% of those enrolled) patients had new or worsening EAs, 24 (41%) had new or worsening background deterioration, 12 (20%) patients developed both findings, and 24 (41%) patients developed neither. And 25 (42%) patients had a HAI; 11 patients (19%) developed hospital-acquired or ventilator-associated pneumonia, 10 (17%) developed a hospital-acquired UTI, 1 (2%) developed sepsis, and 2 (3%) developed C. difficile-associated disease.
In the analysis for referral bias, contemporaneously admitted patients who also had nontraumatic SAH and at least 72 h of cEEG monitoring but did not undergo prospective mRS assessments (n = 51) had a median [IQR] age (58 [48.75–67.25]), mFS score (3 [3–3]), and HH grade (3 [2–4]) similar to the study cohort. Of the patients not included in the cohort, 18 (36%) had a poor discharge mRS (0–3) which is not significantly different from that of patients who were included (p = 0.54). Additional characteristics of patients included in the cohort vs. those who were not are summarized in Supplementary Table S2.
Univariate outcome analysis
Univariate analyses with poor mRS (4–6) at discharge, 3, and 6 months are summarized in Table 2. Poor mRS at discharge was associated with age (p = 0.02), HH grade (p = 0.02), mFS score (p = 0.02), DCI [OR 7.58; 95% CI 1.88–30.6; p = 0.002], and new EAs [OR 4.24; 95% CI 1.1–16.97; p = 0.04]. Evidence of BD on cEEG was not associated with poor discharge mRS (Table 2; Fig. 2). Only 2 events of rebleeding occurred (3.4%).
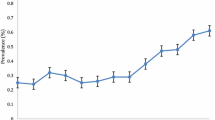
Percentage of patients achieving good outcome (mRS 0–3) at discharge, 3 months and 6 months. a Patients with new or worsening EAs had a significantly better outcome at discharge (Univariate OR 4.24; 95% CI 1.1–16.97; p = 0.04), 3 months (Univariate OR 7.77; 95% CI 2.36–25.6; p = 0.0007) and 6 months (Univariate OR 4.27; 95% CI 1.3–14.2; p = 0.02) compared to those without new or worsening EAs. b Patients with worsening background deterioration did not have a significantly different outcome at discharge (Univariate OR 0.97; 95% CI 0.31–3.1; p = 1.0), 3 months (Univariate OR 1.4; 95% CI 0.47–3.99; p = 0.59) and 6 months (Univariate OR 0.74; 95% CI 0.23–2.4; p = 0.77) compared to those without worsening background deterioration. c Delayed cerebral ischemia was significantly associated with poor outcome at discharge (Univariate OR 7.58; 95% CI 1.88–30.6; p = 0.002), 3 months (OR 4.92; 95% CI 1.55–15.64; p = 0.005) and 6 months (Univariate OR 3.25; 95% CI 0.96–10.97; p = 0.05). d HAI and e hydrocephalus were not associated with poor outcome at any time point. (*p < 0.05; **p < 0.01; ***p < 0.001)
Poor mRS at 3 months was associated with HH grade (p = 0.04), DCI [OR 4.92; 95% CI 1.55–15.64; p = 0.005] and new EAs [OR 7.77; 95% CI 2.36–25.5; p = 0.0007]. Age, cEEG evidence of BD, and HAI were not associated with poor mRS at 3 months (Table 2; Fig. 2).
Poor mRS at 6 months was associated with HH grade (p = 0.04), new EAs [OR 4.27; 95% CI 1.3–14.2; p = 0.02], and DCI [OR 3.25; 95% CI 0.96–10.97; 1-tailed p = 0.05]. BD and mFS score were not associated with poor functional outcome at 6 months (Table 2; Fig. 2).
Shift analysis utilizing the cumulative proportional odds model
In the CPO model, the absence of any new or worsening EAs was associated with a shift towards improved mRS scores at discharge [OR 7.36, 95% CI 2.52–21.5, p = 0.0003], 3 months [OR 4.65, 95% CI 1.73–12.5, p = 0.002] and 6 months [OR 3.53, 95% CI 1.33–9.41, p = 0.012]. When adjusting for age, HH, and mFS (based on the univariate selection criteria), the association between new or worsening EAs and the distribution of mRS was maintained at discharge [OR 4.99, 95% CI 1.60–15.6, p = 0.006] and 3 months [OR 3.28, 95% CI 1.14–9.5, p = 0.03] and trended towards significance at 6 months [OR 2.71, 95% CI 0.95–7.76, p = 0.06]. At the 3- and 6-month time points, the score test for CPO model assumptions indicated possible heterogeneous odds ratios across cutoffs, but a PPO analysis failed to show an interaction of EA with different mRS ordinal thresholds. Therefore, results from the unadjusted CPO were considered valid and used for each time point. In a post hoc CPO analysis, new or worsening EAs remained significantly associated with mRS at discharge [OR 6.85; 95% CI 2.34–21.95; p = 0.006], 3 months [OR 3.61; 95% CI 1.34–10.22; p = 0.01] and 6 months [OR 2.91; 95% CI 1.08–8.1; p = 0.04] when controlling for the APACHE II physiologic sub-score.
Worsening background deterioration was not associated with mRS at discharge [OR 1.2; 95% CI 0.47–3.01; p = 0.72], 3 months [OR 1.3; 95% CI 0.5–3.2; p = 0.59] or 6 months [OR 1.2; 95% CI 0.45–2.93; p = 0.77] (Fig. 3). At the 6-month time point, the score test for CPO model assumptions indicated heterogenous odds ratios across cutoff; however, the PPO analysis again failed to show an interaction of BD with different mRS ordinal thresholds; therefore, results from the unadjusted CPO were considered valid and used. The association between BD and mRS at each time point was again not significant when adjusting for age, HH, and mFS at discharge (Fig. 4).
Forest Plots displaying the independent odds ratio point estimates and confidence intervals from individual cumulative proportional odds models for a discharge, b 3-month, and c 6-month outcome measured ordinally on the modified Rankin Scale. New or worsening EAs (p = 0.006; p = 0.03; p = 0.06) had a higher cumulative proportional odds for a shift to higher mRS scores, independent of age, Hunt-Hess clinical grade, and modified Fisher Scale radiologic grade. Worsening background deterioration was not associated with a shift in outcomes (p = 0.76; p = 0.81; p = 0.97, respectively) at each time point. Each model adjusts for admission factors including age, HH clinical grade, and mFS radiologic grade
In the CPO model, DCI was associated with worse mRS at discharge [OR 5.8; 95% CI 2.08–16.2; p = 0.0008], 3 months [OR 3.7; 95% CI 1.43–9.5; p = 0.007] and 6 months [OR 2.78; 95% CI 1.1–7.3; p = 0.04] (Fig. 3). While the score test for CPO model assumptions was significant at 3 and 6 months, a partial proportional odds model showed a nonsignificant interaction of time with DCI so the CPO results were again considered valid. The score test passed at the 3-month time point. When controlling for covariates age, mFS and HH, DCI was independently associated with worse mRS at discharge [OR 4.75; 95% CI 1.64–13.8; p = 0.004] and 3 months [OR 3.4; 95% CI 1.24–9.01; p = 0.02]. At 6 months, DCI was trending towards being independently associated with worse mRS [OR 2.45; 95% CI 0.94–6.6; p = 0.076].
HAI was not associated with mRS at discharge [OR 1.21; 95% CI 0.48–3.04; p = 0.69], 3 months [OR 0.84; 95% CI 0.34–2.09; p = 0.72] and 6 months [OR 0.87; 95% CI 0.34–2.19; p = 0.77]. When including age, HH, and mFS in the model, HAI was similarly not associated with mRS at any time point (Fig. 4). At the 6-month time point, the score test for CPO model assumptions indicated possible heterogeneous odds ratios across cutoffs, but a PPO analysis again failed to show a significant interaction of HAI with different mRS ordinal thresholds, and so results from the unadjusted CPO were considered valid and used.
Time-dependent analysis using linear mixed effects model
In the linear mixed effects model including time of each outcome assessment and new or worsening EAs, both new or worsening EAs [β = 1.31; 95% CI 0.39–2.24; p = 0.005] and time [β = − 0.755; 95% CI − 0.93 to − 0.58; p < 0.0001] were associated with mRS; however, the interaction between time and new or worsening EAs was not significant [β = 0.35, 95% CI − 0.35 to 1.1; p = 0.33] when added to the model. Adjusting for clinical severity on admission (HH, mFS, age, or risk score) did not change these results. In a post hoc analysis accounting for admission disease severity, new or worsening EAs [β = 0.99; 95% CI 0.22–1.76; p = 0.012] remained significantly associated with mRS over time when controlling for HH, mFS, and the APACHE II physiologic sub-score.
Post Hoc analysis of changes in anti-seizure medication
In a post hoc analysis of the 23 patients with new or worsening EAs, ASM changes were not associated with outcome at discharge, 3 months, or 6 months (Supplementary Table S3). Among patients with new or worsening EAs, the percent discharged on an ASM was numerically lower (26%, 21%, and 20%) among those with a poor outcome at discharge, 3 months, and 6 months compared to those with a good outcome at each time point (50%, 44%, and 33%), although these differences was not significant at any of these time points.
Discussion
In this cohort of nontraumatic SAH patients with high clinical or radiologic grade, cEEG abnormalities have a differential association with functional outcome. While both have previously been shown to predict DCI [4, 5], our results suggest that only new or worsening EAs appear to have a strong, durable association with outcome measured by the modified Rankin Scale, similar to that for DCI itself. By demonstrating that background deterioration lacks this association and that a worsening in EA burden may influence recovery more than other hospital complications such as HAI, hydrocephalus, or the rare occurrence of aneurysmal rebleeding, our results build upon prior findings linking EA burden to poor outcome following SAH [5]
These results may help elucidate potential mechanisms contributing to DCI, a dangerous complication following SAH [26]. Neurophysiologic changes have previously been proposed as one pathway contributing to DCI progression [27] and new or worsening EAs are representative of poor cerebral metabolism [9,10,11,12] and have been shown to predict DCI [4, 5]. Furthermore, these EEG abnormalities have previously been linked to cortical spreading depolarizations [10,11,12], which themselves have been associated with DCI and subsequent poor outcome [13, 28, 29]. Prior literature illustrates that new or worsening EAs are strongly co-linear with subsequent DCI, which is likely an in-hospital complication intermediate in the chain of events leading to poor outcome, rather than a confounder [6]. Given that new or worsening EAs have been shown to occur prior to DCI, our results indicate they may be a potentially modifiable target to improve functional outcome [5]. While it is possible that currently unrecognized upstream factors, such as cortical spreading depolarizations, cause both DCI and new or worsening EAs, prior studies point to a temporal association between EAs and metabolic crisis [9,10,11,12]. We speculate that the association between DCI and new or worsening EAs may represent a pathogenic mechanism related to cortical spreading depolarizations, to metabolic crisis induced by exhaustive hypermetabolism from new or worsening EAs, or alternatively to anti-seizure medication overtreatment.
Like new or worsening EAs, BD has also been shown to predict DCI in prior studies [6, 7, 30,31,32,33]; however, our results indicate that this association between BD and DCI does not extend to outcome. While medication effects or toxic metabolic causes of neurologic deterioration were strict exclusions in definitions of DCI, it is possible that unmeasured transient clinical factors, such as occult hydrocephalus, unmeasured infections, and other transient phenomena, contributed to background deterioration. Additionally, it is possible that BD results in effects on cognitive but not functional outcomes. Although our sample size may have been underpowered to detect an influence of new or worsening background deterioration on functional outcome, the effect size was small in this cohort. It is also possible that BD may be more readily treated with current interventions than new or worsening EAs or that BD is more strongly associated with cognitive sequelae, whereas the mRS scale is highly sensitive to motor symptoms. Future studies might evaluate both functional and cognitive outcomes to assess for this possibility.
Our study is subject to the typical limitations of a single-center retrospective analysis. Beyond this, there is risk of referral bias due to sampling a subpopulation of all SAH patients who underwent at least 3 days of cEEG monitoring as standard of care. However, we compared baseline admission risk severity between our cohort and all other SAH patients admitted during the study period with at least 3 days of cEEG monitoring and found similar age, mFS, and HH. Therefore, we believe that our study cohort is representative of SAH patients admitted to our institution with at least 3 days of cEEG monitoring. Given that the exposure variables were available to the treating team, it is likely that our findings are conservative if treatment triggered by cEEG findings mitigated their association with outcome. Additionally, it is unlikely that the findings were associated with “a self-fulfilling prophecy,” since new or worsening EAs and background deterioration had a differential influence on outcome despite both being monitored due to their association with DCI. Aneurysmal rebleed has been shown to be an important outcome predictor, however, we were unable to account for this due to the low rate of aneurysmal rebleed in our cohort. We did not explicitly control for ASM in our analysis because it is standard of care at our institution for all patients to receive seizure prophylaxis until the culpable aneurysm is secured. However, in a post hoc analysis among patients with new or worsening EAs, ASM changes during hospitalization did not have a significant association with outcome and the sample size did not afford the opportunity to show a significant association between ASM treatment at discharge with functional outcome. Despite this evidence, we were unable to control for sedation, which represents a limitation. Although at the time of outcome assessments, patients were no longer on sedation, there remains the possibility that that increased sedation administered to patients with new or worsening EAs could have effects on outcome, although any such effect may also represent an important intermediate in the chain of events leading poor outcome. Future outcome studies should account for ASM when analyzing the association between EEG and outcomes in SAH patients.
In conclusion, our results demonstrate that the occurrence of new or worsening epileptiform abnormalities following SAH has a unique and durable association with functional outcome, similar to that of DCI itself. Utilizing these findings for patient enrichment strategies, including new or worsening EAs as a criterion for clinical trial enrollment, may improve the power to demonstrate a benefit by applying targeted treatments to those patients with the greatest opportunity to benefit. Future studies are needed to validate our findings in a larger cohort that can control for sedation, physiologic disease severity, and aneurysmal rebleed. This will enable us to better understand and validate these findings and to allow the full potential of this monitoring modality to be realized in the SAH population.
Data availability statement
The original data are available from the authors upon reasonable request.
References
Witsch J, Frey HP, Patel S, et al. Prognostication of long-term outcomes after subarachnoid hemorrhage: The FRESH score. Ann Neurol. 2016;80:46–58.
Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968;28(1):14–20.
De Marchis GM, Pugin D, Meyers E, et al. Seizure burden in subarachnoid hemorrhage associated with functional and cognitive outcome. Neurology. 2016;86(3):253–60.
Kim JA, Rosenthal ES, Biswal S, et al. Epileptiform abnormalities predict delayed cerebral ischemia in subarachnoid hemorrhage. Clin Neurophysiol [Internet]. 2017;128(6):1091–9.
Zafar SF, Postma EN, Biswal S, et al. Effect of epileptiform abnormality burden on neurologic outcome and antiepileptic drug management after subarachnoid hemorrhage. Clin Neurophysiol. 2018;129(11):2219–27.
Rosenthal ES, Biswal S, Zafar SF, et al. Continuous electroencephalography predicts delayed cerebral ischemia after subarachnoid hemorrhage: a prospective study of diagnostic accuracy. Ann Neurol. 2018;83(5):958–69.
Rots ML, van Putten MJAM, Hoedemaekers CWE, Horn J. Continuous EEG monitoring for early detection of delayed cerebral ischemia in subarachnoid hemorrhage: a pilot study. Neurocrit Care. 2016;24:207–16.
Claassen J, Hirsch LJ, Frontera JA, et al. Prognostic significance of continuous EEG monitoring in patients with poor-grade subarachnoid hemorrhage. Neurocrit Care. 2006;4:103–112.
Struck AF, Westover MB, Hall LT, Deck GM, Cole AJ, Rosenthal ES. Metabolic correlates of the ictal-interictal continuum: FDG-PET during continuous EEG. Neurocrit Care. 2016;24(3):324–31.
Subramaniam T, Jain A, Hall LT, et al. Lateralized periodic discharges frequency correlates with glucose metabolism. Neurol. 2019:92(7);e670–74.
Witsch J, Frey HP, Schmidt JM, et al. Electroencephalographic periodic discharges and frequency-dependent brain tissue hypoxia in acute brain injury. JAMA Neurol. 2017;74:301–9.
Vespa P, Tubi M, Claassen J, et al. Metabolic crisis occurs with seizures and periodic discharges after brain trauma. Ann Neurol. 2016;79:579–90.
Dreier JP, Woitzik J, Fabricius M, et al. Delayed ischemic neurological deficits after subarachnoid haemorrhage are associated with clusters of spreading depolarizations. Brain. 2006;129(12):3224–37.
Dreier JP. The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat Med. 2011;17:439–447.
Drenckhahn C, Winkler MKL, Major S, et al. Correlates of spreading depolarization in human scalp electroencephalography. Brain. 2012;135(4):853–68.
Hartings JA, Watanabe T, Bullock MR, et al. Spreading depolarizations have prolonged direct current shifts and are associated with poor outcome in brain trauma. Brain. 2011;134(5):1529–40.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. UroToday Int J. 2009;2(2):20–2.
Muniz C, Shenoy A, O’Connor KL, et al. Clinical development and implementation of an institutional guideline for prospective EEG monitoring and reporting of delayed cerebral ischemia CF. J Clin Neurophysiol. 2017;33(3):217–26.
Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. Guidelines for preventing health-care--associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep 2004
CDC C for DC and P. Clostridioides difficile (C. diff). CDC, Centers Dis. Control Prev. Clostridioides difficle. 2018
Sheet SF. CDC. WwwCdcGov: Sepsis Fact Sheet; 2015.
Centers for Disease Control and Prevention. Urinary Tract Infection (Catheter-Associated Urinary Tract Infection [CAUTI] and Non-Catheter-Associated Urinary Tract Infection [UTI]) and Other Urinary System Infection [USI]) Events. In: 2016 NHSN Patient Safety Component Manual. 2016.
Hirsch LJ, Laroche SM, Gaspard N, et al. American clinical neurophysiology society’s standardized critical care EEG terminology: 2012 version. J Neurophysiol. 2013;30(1):1–27.
Foreman B. The pathophysiology of delayed cerebral ischemia. J Clin Neurophysiol. 2016;33(3):174–82.
Ogilvy CS, Carter BS. A proposed comprehensive grading system to predict outcome for surgical management of intracranial aneurysms. Neurosurgery. 1998;42(5):959–68.
Eagles ME, Tso MK, Macdonald RL. Cognitive impairment, functional outcome, and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2019;124:e558–62.
Dreier JP. The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat Med. 2011;17(4):439–47.
Sugimoto K, Nomura S, Shirao S, et al. Cilostazol decreases duration of spreading depolarization and spreading ischemia after aneurysmal subarachnoid hemorrhage. Ann Neurol. 2018;84:873–85.
Woitzik J, Dreier JP, Hecht N, et al. Delayed cerebral ischemia and spreading depolarization in absence of angiographic vasospasm after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2012;32(2):203–12.
Labar DR, Fisch BJ, Pedley TA, Fink ME, Solomon RA. Quantitative EEG monitoring for patients with subarachnoid hemorrhage. Electroencephalogr Clin Neurophysiol. 1991;78(5):325–32.
Vespa PM, Nuwer MR, Juhász C, et al. Early detection of vasospasm after acute subarachnoid hemorrhage using continuous EEG ICU monitoring. Electroencephalogr Clin Neurophysiol. 1997;103(6):607–15.
Claassen J, Hirsch LJ, Kreiter KT, et al. Quantitative continuous EEG for detecting delayed cerebral ischemia in patients with poor-grade subarachnoid hemorrhage. Clin Neurophysiol. 2004;115(12):2699–710.
Yu Z, Wen D, Zheng J, et al. Predictive accuracy of alpha-delta ratio on quantitative electroencephalography for delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage: meta-analysis. World Neurosurg. 2019;126:e510–6.
Funding
NIH/NINDS K23NS105950, American Heart Association, Andrew David Heitman Neurovascular Research Foundation.
Author information
Authors and Affiliations
Contributions
IAL conceptualized the study design and carried out the data analysis and interpretation, drafting and manuscript revisions. JJL contributed to the data analysis, interpretation and manuscript revisions. SFZ assisted with data acquisition, interpretation and manuscript revisions. RLS contributed to data analysis and manuscript revisions. ABP, TLM, CJS, MJK participated in interpretation and manuscript revisions. JAK assisted with data acquisition and manuscript revisions. KA contributed to data acquisition and data management. JR assisted with data interpretation and manuscript revisions. MBW and WTK carried out data acquisition and manuscript revisions. ESR conducted study design conceptualization, data analysis and interpretation as well as manuscript drafting and revisions.
Corresponding author
Ethics declarations
Ethical approval
The authors have adhered to ethical guidelines, and this study was approved by the institutional IRB.
Conflicts of interest
India Lissak has nothing to disclose. Dr. Locascio has nothing to disclose. Dr. Zafar reports grants from Sage therapeutics, grants from K23NS114201, outside the submitted work. Riana Schleicher has nothing to disclose. Dr. Patel reports personal fees from Penumbra, personal fees from Microvention, personal fees from Medtronic, outside the submitted work. Dr. Leslie-Mazwi has nothing to disclose. Dr. Stapleton has nothing to disclose. Dr. Koch has nothing to disclose. Dr. Kim has nothing to disclose. Kasey Anderson has nothing to disclose. Dr. Rosand reports grants from National Institutes of Health, grants from OneMind for Research, grants from American Heart Association, personal fees from Boehringer Ingelheim, outside the submitted work. Dr. Westover reports grants from NIH, during the conduct of the study. Dr. Kimberly reports grants and personal fees from Biogen, grants and personal fees from NControl Therapeutics, outside the submitted work; In addition, Dr. Kimberly has a patent 62/460,229 licensed to NControl Therapeutics. Dr. Rosenthal reports personal fees from UCB Pharmaceuticals, personal fees from Ceribell, Inc, grants from Department of Defense, outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lissak, I.A., Locascio, J.J., Zafar, S.F. et al. Electroencephalography, Hospital Complications, and Longitudinal Outcomes After Subarachnoid Hemorrhage. Neurocrit Care 35, 397–408 (2021). https://doi.org/10.1007/s12028-020-01177-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01177-x