Abstract
Background
Glucose control status after cardiac arrest depending on chronic glycemic status and the association between chronic glycemic status and outcome in cardiac arrest survivors are not well known. We investigated the association between glycated hemoglobin (HbA1c) and 6-month neurologic outcome in cardiac arrest survivors undergoing therapeutic hypothermia (TH) and whether mean glucose, area under curve (AUC) of glucose during TH, and neuron-specific enolase (NSE) are different between normal and high HbA1c groups.
Methods
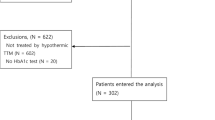
This retrospective single-center study included adult comatose cardiac arrest survivors who underwent TH from September 2011 to December 2017. HbA1c and glucose were measured after return of spontaneous circulation (ROSC), and normal or high HbA1c was defined using cutoff value of 6.4% of HbA1c. Blood glucose was measured at least every 4 h and treated with a written protocol to maintain the range of 80–200 mg/dL. Hypoglycemia and hyperglycemia were defined with glucose < 70 or > 180 mg/dL. Mean glucose during induction and rewarming phase and AUC of glucose during every 6 h of maintenance were calculated, and NSE at 48 h after cardiac arrest was recorded. The primary outcome was unfavorable neurologic outcome, defined as Glasgow Pittsburgh Cerebral Performance Category scale 3–5 at 6 months after cardiac arrest.
Results
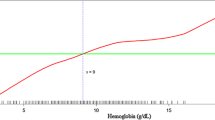
Of 384 included patients, 81 (21.1%) had high HbA1c and 247 (64.3%) had an unfavorable neurologic outcome. Patients with high HbA1c were more common in the unfavorable group than in favorable group (27.5% vs 9.5%, p < 0.001), and the unfavorable group had significantly higher HbA1c level (5.8% [5.4–6.8%] vs 5.6% [5.3–6.0%], p = 0.007). HbA1c level was independently associated with worse neurologic outcome (odds ratio 1.414; 95% confidence interval 1.051–1.903). High HbA1c group had higher glucose after ROSC, glucose AUC during maintenance, and rewarming phase than normal HbA1c group. High HbA1c group had significantly higher incidence of hyperglycemia throughout the TH, while normal HbA1c group had significantly higher incidence of normoglycemia. However, no glucose parameter remained as an independent predictor of neurologic outcome after adjustment, irrespective of HbA1c level. NSE showed good prognostic performance (area under curve 0.892; cutoff value 26.3 ng/mL). Although NSE level was not different between HbA1c groups, high HbA1c group had higher proportion of patient having NSE over cutoff.
Conclusions
Higher HbA1c was independently associated with unfavorable neurologic outcome. Glycemic status during TH was different between normal and high HbA1c groups.




Similar content being viewed by others
References
Nolan JP, Soar J, Cariou A, et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines for post-resuscitation care 2015: section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation. 2015;95:202–22.
Callaway CW, Donnino MW, Fink EL, et al. Part 8: post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S465–82.
Gaieski DF, Band RA, Abella BS, et al. Early goal-directed hemodynamic optimization combined with therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest. Resuscitation. 2009;80(4):418–24.
Sunde K, Pytte M, Jacobsen D, et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73(1):29–39.
McCowen KC, Malhotra A, Bistrian BR. Stress-induced hyperglycemia. Crit Care Clin. 2001;17(1):107–24.
Daviaud F, Dumas F, Demars N, et al. Blood glucose level and outcome after cardiac arrest: insights from a large registry in the hypothermia era. Intensive Care Med. 2014;40(6):855–62.
Kim SH, Choi SP, Park KN, et al. Association of blood glucose at admission with outcomes in patients treated with therapeutic hypothermia after cardiac arrest. Am J Emerg Med. 2014;32(8):900–4.
Nielsen N, Hovdenes J, Nilsson F, et al. Outcome, timing and adverse events in therapeutic hypothermia after out-of-hospital cardiac arrest. Acta Anaesthesiol Scand. 2009;53(7):926–34.
Beiser DG, Carr GE, Edelson DP, Peberdy MA, Hoek TL. Derangements in blood glucose following initial resuscitation from in-hospital cardiac arrest: a report from the national registry of cardiopulmonary resuscitation. Resuscitation. 2009;80(6):624–30.
Larsson M, Thoren AB, Herlitz J. A history of diabetes is associated with an adverse outcome among patients admitted to hospital alive after an out-of-hospital cardiac arrest. Resuscitation. 2005;66(3):303–7.
Ro YS, Shin SD, Song KJ, et al. Risk of diabetes mellitus on incidence of out-of-hospital cardiac arrests: a case-control study. PLoS ONE. 2016;11(4):e0154245.
Ro YS, Shin SD, Song KJ, et al. Interaction effects between hypothermia and diabetes mellitus on survival outcomes after out-of-hospital cardiac arrest. Resuscitation. 2015;90:35–41.
Voruganti DC, Chennamadhavuni A, Garje R, et al. Association between diabetes mellitus and poor patient outcomes after out-of-hospital cardiac arrest: a systematic review and meta-analysis. Sci Rep. 2018;8:17921.
Nathan DM, Turgeon H, Regan S. Relationship between glycated haemoglobin levels and mean glucose levels over time. Diabetologia. 2007;50(11):2239–44.
Hempe JM, Gomez R, McCarter RJ Jr, Chalew SA. High and low hemoglobin glycation phenotypes in type 1 diabetes: a challenge for interpretation of glycemic control. J Diabetes Complicat. 2002;16(5):313–20.
Nathan DM, Singer DE, Hurxthal K, Goodson JD. The clinical information value of the glycosylated hemoglobin assay. N Engl J Med. 1984;310(6):341–6.
Gornik I, Gornik O, Gasparovic V. HbA1c is outcome predictor in diabetic patients with sepsis. Diabetes Res Clin Pract. 2007;77(1):120–5.
Kompoti M, Michalia M, Salma V, et al. Glycated hemoglobin at admission in the intensive care unit: clinical implications and prognostic relevance. J Crit Care. 2015;30(1):150–5.
International Expert C. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327–34.
Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2014;132:1286–300.
Lehot JJ, Piriz H, Villard J, Cohen R, Guidollet J. Glucose homeostasis comparison between hypothermic and normothermic cardiopulmonary bypass. Chest. 1992;102(1):106–11.
Borgquist O, Wise MP, Nielsen N, et al. Dysglycemia, glycemic variability, and outcome after cardiac arrest and temperature management at 33 °C and 36 °C. Crit Care Med. 2017;45(8):1337–43.
Jaisson S, Leroy N, Guillard E, Desmons A, Gillery P. Analytical performances of the D-100™ hemoglobin testing system (Bio-Rad) for HbA1c assay. Clin Chem Lab Med. 2015;53(9):1473–9.
Lee BK, Lee HY, Jeung KW, et al. Association of blood glucose variability with outcomes in comatose cardiac arrest survivors treated with therapeutic hypothermia. Am J Emerg Med. 2013;31(3):566–72.
Vincent JL, deMendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793–800.
Wang C, Chang J, Huang C, et al. The association between long-term glycaemic control, glycaemic gap and neurologic outcome of in-hospital cardiac arrest in diabetes: a retrospective cohort study. Resuscitation. 2018;133:18–24.
Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ, et al. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31(8):1473–8.
Booth CM, Boone RH, Tomlinson G, Detsky AS. Is this patient dead, vegetative, or severely neurologically impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004;291(7):870–9.
Luethi N, Cioccari L, Tanaka A, et al. Glycated hemoglobin A1c levels are not affected by critical illness. Crit Care Med. 2016;44(9):1692–4.
Timmer JR, Hoekstra M, Nijsten MW, et al. Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST-segment-elevation myocardial infarction treated with percutaneous coronary intervention. Circulation. 2011;124(6):704–11.
Borai A, Livingstone C, Abdelaal F, et al. The relationship between glycosylated haemoglobin (HbA1c) and measures of insulin resistance across a range of glucose tolerance. Scand J Clin Lab Invest. 2011;71(2):168–72.
Sen S, Kar M, Roy A, Chakraborti AS. Effect of nonenzymatic glycation on functional and structural properties of hemoglobin. Biophys Chem. 2005;113(3):289–98.
Virtue MA, Furne JK, Nuttall FQ, Levitt MD. Relationship between GHb concentration and erythrocyte survival determined from breath carbon monoxide concentration. Diabetes Care. 2004;27(4):931–5.
Ameloot K, Genbrugge C, Meex I, et al. Low hemoglobin levels are associated with lower cerebral saturations and poor outcome after cardiac arrest. Resuscitation. 2015;96:280–6.
Kim D, Kim SH, Park KN, et al. Hemoglobin concentration is associated with neurologic outcome after cardiac arrest in patients treated with targeted temperature management. Clin Exp Emerg Med. 2018;5(3):150–5.
Johnson NJ, Rosselot B, Perman SM, et al. The association between hemoglobin concentration and neurologic outcome after cardiac arrest. J Crit Care. 2016;36:218–22.
Albaeni A, Eid SM, Akinyele B, et al. The association between post resuscitation hemoglobin level and survival with good neurological outcome following Out Of Hospital cardiac arrest. Resuscitation. 2016;99:7–12.
Krinsley JS, Egi M, Kiss A, et al. Diabetic status and the relation of the three domains of glycemic control to mortality in critically ill patients: an international multicenter cohort study. Crit Care. 2013;17(2):R37.
Acknowledgements
This work was approved by Chonnam National University Hospital Institutional Review Board (Protocol No. CNUH-2018-207).
Funding
There was no support for this work.
Author information
Authors and Affiliations
Contributions
BK Lee contributed to project development, data analysis, data interpretation, and manuscript writing; JC Rittenberger contributed to data interpretation and manuscript writing; DH Lee contributed to data collection and manuscript edition; SW Yun contributed to data collection and manuscript edition; KW Jeung contributed to data analysis and manuscript edition; CW Callaway contributed to data interpretation and manuscript edition.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12028_2019_758_MOESM1_ESM.tif
Supplemental figure. Receiver operating characteristics of HbA1c for neurologic outcome and mortality. (A) HbA1c showed an area under curve of 0.583 (95% confidence interval, 0.532–0.633; p = 0.004) for unfavorable neurologic outcome and the cutoff value by Youden index was 6.3% (sensitivity, 30.4%; specificity, 89.8%). (B) HbA1c showed an area under curve of 0.593 (95% confidence interval, 0.542–0.642; p = 0.001) for 6-month mortality and the cutoff value by Youden index was 6.3% (sensitivity, 32.9%; specificity, 88.5%) (TIFF 536 kb)
Rights and permissions
About this article
Cite this article
Lee, B.K., Lee, D.H., Jeung, K.W. et al. Glycated Hemoglobin is Associated with Glycemic Control and 6-Month Neurologic Outcome in Cardiac Arrest Survivors Undergoing Therapeutic Hypothermia. Neurocrit Care 32, 448–458 (2020). https://doi.org/10.1007/s12028-019-00758-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00758-9