Abstract
Management of Traumatic Brain Injury (TBI) focuses on controlling intracranial pressure (ICP), while other treatments, such as the use of neuromuscular blocking agents (NMBAs), need scientific evidence. We conducted a systematic review to investigate the usefulness of NMBAs in the context of TBI and/or increased ICP. We searched MEDLINE and EMBASE databases up to January 31st 2014, including both clinical and experimental findings. We found a total of 34 articles, of which 22 were prospective clinical trials. No systematic review/meta-analyses were found. Seven studies evaluated NMBA boluses in preventing stimulation-related ICP surges: paralysis was effective during tracheal suctioning and physiotherapy but not during bronchoscopy. Fourteen small studies (8 to 25 patients) assessed the effect of NMBA boluses on ICP. Two studies showed an ICP increase by succinylcholine and one found a decrease in ICP after atracurium. No ICP changes were observed in the other studies. One prospective study confirmed that discontinuing paralysis increases energy expenditure. Two retrospective studies investigated mortality/morbidity: one found that early paralysis (continued for >12 h) was not beneficial and potentially associated with extra-cranial complications, while the second demonstrated a correlation between continuous infusion of NMBA and time spent with ICP > 20 mmHg. Eight animal studies were also retrieved. In most studies, NMBA bolus was beneficial in controlling ICP, especially when performing stimulating procedures. However, retrospective evidence found potential harm by continuous NMBA infusion. In the context of TBI patients, we discuss the potentially positive effects of paralysis with its negative ones. Well-conducted randomized controlled trials and/or large pharmaco-epidemiologic studies are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
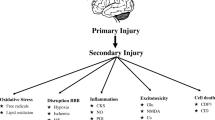
Traumatic brain injury (TBI) is the leading cause of disability in the population below 40 years of age [1]. The treatment of TBI patients focuses on the prevention of secondary brain damage. So far, several pharmacological options have been investigated, but there is still paucity of evidence for effective strategies in humans. The management of intracranial pressure (ICP) remains the cornerstone of treatment [2].
Neuromuscular blocking agents (NMBAs) are commonly considered, sometimes also at early stages, in patients with TBI and increase of ICP [3, 4]. However, their use in this category of critically ill patients seems mostly based on theoretical considerations, while there is poor evidence about their effects on long-term outcome. Early paralysis has recently shown a positive impact in patients with acute respiratory distress syndrome (ARDS) [5, 6], and a recent large pharmaco-epidemiologic study demonstrated a lower in-hospital mortality in patients with severe sepsis and respiratory infection receiving early treatment with NMBAs [7].
Paralysis may facilitate the mechanical ventilation of TBI patients, in which thorough control of CO2 and optimal oxygenation with low levels of positive end-expiratory pressure (PEEP) remains crucial. Other potential benefits of pharmacological paralysis in patients with head injury and refractory increase of ICP may include (1) prevention of shivering, if actively managing temperature in febrile patients or cooling with neuroprotective intent; (2) limitation of cough and related ICP surges after its elicitation, for instance with tracheal suctioning [8–12]; and (3) a further decrease of the energy expenditure [13].
Nevertheless, continuous paralysis can mask the presence of post-traumatic seizure activity [14]. Furthermore, patients with TBI and raised ICP are usually mechanically ventilated for prolonged periods and therefore exposed to the risk of developing critical illness polyneuropathy (CIP) and/or myopathy (CIM). While a clear link between NMBAs and the development of CIP/CIM is still uncertain [15, 16], it could be worth to carefully consider paralysis in these patients. The development of CIP/CIM may delay respiratory weaning [17, 18], as well as the rehabilitation process, and may instigate unreasonably pessimistic prognosis [18].
The scope of this systematic review was to retrieve, categorize, and summarize the presently available literature on the long-term outcomes (i.e., morbidity and mortality) of pharmacological paralysis in patients with TBI and increased ICP admitted to the intensive care unit (ICU).
Methods
We conducted a systematic web-based literature search through the NHS Library Evidence tool on the short- and long-term effects of NMBA administration in the context of TBI and raised ICP.
We followed the approach suggested by the PRISMA statement for reporting systematic reviews and meta-analyses [19]. However, due to the small number of randomized controlled studies (RCTs) published, we a priori decided to also include non-randomized prospective and retrospective clinical studies as well as the findings of experimental research. Yet, the aim of this expanded systematic search is to provide a broaden insight on the topic for supporting the design of large RCTs, and meanwhile to provide ICU clinicians with a more detailed rationale for starting/holding pharmacological paralysis in such patients, by a structured description of the possible therapeutic benefits and the potential harm of paralysis in this patients population.
Inclusion criteria for clinical studies were pre-specified according to the PICOS approach (Table 1). We excluded articles referring to the pediatric population and studies performed in the pre-hospital emergency setting. Case series were included in the study if reporting at least 5 patients; series with a lower number of patients and case reports was excluded. With regard of experimental evidence, we included only animal models of TBI and/or raised ICP treated with NMBAs, excluding in vitro research.
A computerized search of the two most significant Healthcare Databases, MEDLINE (PubMed) and EMBASE, from inception until January 31st, 2014 was performed to identify relevant articles.
Our core search was structured in the combination of terms obtained from the two following groups. The first group is included in alphabetical order: “atracurium,” “cisatracurium,” “doxacurium,” “metocurine,” “mivacurium,” “neuromuscular blockade,” “neuromuscular block,” “NMB,” “pancuronium,” “pipecuronium,” “rocuronium,” “succinylcholine,” “suxamethonium,” “tubocurarine,” or “vecuronium.” The second group consisted of the following: “brain injuries,” “brain trauma,” “head injury,” “head trauma,” “intracranial injury,” “intracranial trauma,” “traumatic brain injury,” or “TBI”. The search strategy is summarized in the “Supplemental Digital Content—Appendix 1.”
Three authors (FS, CS, and MOM) and a senior librarian (see acknowledgements) independently searched these databases. Duplicates were initially filtered through automated software function and afterward screened manually by three authors (FS, CS, and MA). Study selection for determining the eligibility for inclusion in the systematic review and data extraction from the selected studies were performed independently by three reviewers (FS, CS, and MA). Discordances were resolved by involving another reviewer (MOM) and/or by consensus.
Language restrictions were applied: only articles published in English, French, German, or Italian were considered. Findings retrieved from EMBASE as conference abstract are reported only if published after January 2011 to allow a reasonable time for multiple peer-reviewed process.
A further manual search was conducted independently by two authors (FS and CS), exploring the list of references of the findings of the systematic search. Finally, we excluded from the qualitative synthesis book chapters, reviews, editorials, and letters to editor, but provided them separately (“Supplemental Digital Content—Appendix 2”).
Results
The literature search with the above-mentioned criteria produced 571 findings; of them 129 duplicates were removed via automatic software leaving a total of 442 publications. We excluded 381 findings as judged not relevant to our search target. Of the remaining 61 findings, further 15 were excluded, 14 duplicates were identified manually, and one finding was in Russian language. The manual search did not add further findings. From the entire search, we excluded seven reviews, three editorials/letters to the editor, two surveys, and two small case series (reporting 3 and 4 patients). A total of 32 articles remained for the qualitative synthesis as shown in Fig. 1.
The description of the design of the studies found is summarized in Table 2. No systematic reviews and meta-analysis assessed the effects of the NMBA use in patients with TBI. The findings of small randomized controlled trials (RCTs) and of prospective studies are also reported in Table 3.
Randomized Controlled Trials and Prospective Studies
A total of 22 prospective studies (including small RCTs) were identified. Seven of them evaluated the ability of different NMBAs (including succinylcholine) in preventing surges of ICP after patient’s stimulation with endotracheal suctioning [8–12], fiberoptic bronchoscopy [20], or physiotherapy [21]. In these studies, a bolus of different NMBAs was effective in preventing ICP increasedue to endotracheal suctioning or physiotherapy. However, a bolus of vecuronium bolus associated to sedation, analgesia, and topical anesthesia of the airways during bronchoscopy was not effective in preventing the rise of ICP.
Further 14 prospective studies targeted the effect of the bolus of a NMBA on several cerebral (mainly ICP; cerebral perfusion pressure—CPP; cerebral blood flow—CBF; electroencephalography—EEG) ± cardiovascular (i.e., mean arterial pressure—MAP; heart rate—HR; central venous pressure—CVP) parameters [22–35]. All these studies were fairly small (treatment group ranging between 8 and 25 patients), mostly outdated, and conducted in heterogeneous neurological populations, either TBI [22, 23] or other neurosurgical/neurocritical care populations [24–35]. Only two studies convincingly showed changes, in both cases being ICP increased by succinylcholine bolus administration [24, 25]. However, a third study on the effects of succinylcholine failed to demonstrate alterations in CBF velocity, EEG, or ICP [26]. With regards to the non-depolarizing NMBAs, only one of the prospective studies showed significant reduction of ICP, CPP, and MAP with a peak 2–4 min after bolus of atracurium [27]. Nevertheless, all the other studies failed to show significant changes in the above parameters by non-depolarizing NMBA boluses [28–35]. None of these studies assessed the impact of pharmacological paralysis on patients’ long-term outcomes.
One prospective trial evaluated the impact on the energy expenditure of interrupting paralysis (pancuronium) in a population of 18 patients with severe head injury; mean energy expenditure, evaluated through indirect calorimetry, significantly increased after paralysis discontinuation [13].
Retrospective Studies
Two retrospective studies were found, one of them assessing the effect of NMBA use on morbidity and/or mortality in patients with TBI [36]. In a population of 514 patients, retrieved from the National Coma Data Bank, the authors found that early paralysis continued for at least 12 h did not improve outcome and may be detrimental by prolonging the ICU length of stay and by increasing the frequency of paralysis-related extra-cranial complications (pneumonia).
The other retrospective study is a post hoc analysis in a population of 326 patients suffering severe head injury enrolled in a RCT. The authors found a correlation between continuous infusion of NMBA and the length of time spent in the “harmful period” (defined as ICP > 20 mmHg) [37].
Experimental Studies
We found eight animal studies (dogs, swine, cats, rats, and monkeys); seven of them principally investigated the effects of one or more NMBAs (atracurium, vecuronium, succinylcholine, and pancuronium) on cerebral (i.e., ICP, CPP, and EEG) ± hemodynamic (i.e., MAP, HR, and CVP) parameters [38–44]. In four of these studies, neither succinylcholine nor non-depolarizing agents (atracurium or vecuronium) produced significant changes in ICP (±hemodynamic parameters) under conditions of normal or artificially increased ICP [38–41]. In a monkeys’ model of intracranial hypertension, Haigh et al. showed no changes in ICP after succinylcholine or atracurium administration [42]. In a swine model, Ducey et al. found no changes in ICP and hemodynamics after atracurium or vecuronium, while succinylcholine determined an increase in ICP coupled with a fall in MAP resulting in decreased CPP [43]. Lanier et al. showed stable ICP, EEG, and other cerebral parameters by different doses of pancuronium or atracurium in anesthetized dogs, and found modest cerebral stimulation induced by atracurium [44]. One study found that a curare bolus increases CBF in a case of disrupted blood–brain barrier [45]. This increase was blocked by pre-treatment with a histamine2-antagonist, indicating the role of this receptor for curare-related augmented CBF in presence of damaged brain barrier.
Discussion
Our systematic review has confirmed the lack of strong evidence about the effect of NMBAs on long-term outcome in patients with TBI and/or increased ICP. Suboptimal data are presently available on their long-term effects, and the best evidence comes from a post hoc analysis of a RCT [36].
More results are available for the short-term effects of paralysis on the ICP and on other cerebrovascular parameters. However, the small sample size of these studies (treatment group ranging between 8 and 25 patients or 6 to 18 animals), the large presence of studies mostly outdated (all of them older than 15 years), and the different NMBAs tested in each study (eight drugs in total) hardly allow to draw any firm conclusions and do not warrant a meta-analysis.
Succinylcholine increased ICP in two of three clinical studies and in one of six experimental animal studies, leaving with a degree of uncertainty about its effects on ICP. More consistent results have been found on the effect of non-depolarizing NMBAs. Only one of nine clinical studies and none of seven animal studies showed significant changes in ICP, MAP, and other variables. Therefore, non-depolarizing NMBAs may be safer in TBI patients with regard to their short-term effects on ICP.
Despite their methodological limitations, some data on long-term outcome have been extrapolated by the two retrospective studies, which showed a potential association between the use of NMBAs and prolonged ICU length of stay, higher frequency of paralysis-related complications [36], and longer time spent with high ICP [37]. Nevertheless, these two studies are not enough to draw firm conclusions.
In absence of strong data, it is not surprising that there is not a clinician’s wide agreement regarding the prolonged use of NMBA infusion in patients with TBI. Two surveys conducted in Canada and in the United Kingdom have shown some discordant results and confirm that the use of paralysis in this population relies mainly on clinicians’ preference [4, 46]. Participants to the Canadian survey considered NMBA use of uncertain appropriateness in patients with diffuse axonal injury [46]. Interestingly, the British survey showed that NMBAs were commonly used in patients with severe head injury, with 40 % of the responding centers using paralysis in 100 % of their patients [4].
The lack of strong evidence about the use of pharmacological paralysis is also common to the general ICU setting, and two surveys (Canada and United States) showed a low uptake of protocols for the usage of NMBAs (22 and 46.8 %, respectively) [47, 48], despite guidelines have been developed [49].
From the evidence retrieved and qualitatively analyzed, we believe that use of NMBAs in TBI patients has to be considered carefully, balancing the impact of positive and negative aspects of pharmacological paralysis, especially if considering a continuous infusion. For this reason, prospective RCTs are warranted to better understand not only transitory effects of NMBAs on ICP, CPP, and MAP but also the long-term impact of continuous paralysis in patients with TBI.
We take the opportunity to further discuss the possible advantages and the potential harmful effects of initiation of muscle-relaxant infusion in TBI patients and refractory increase in ICP. These are as follows:
Potential Advantages of Treatment with NMBAs After Traumatic Brain Injury
Ventilation Management
TBI itself is an independent risk factor for the development of acute lung injury, and the ventilation of TBI patients can become challenging, not only for the mandatory control of PaCO2 and the limited use of PEEP. Yet, patients may develop a respiratory deterioration due to various reasons (pulmonary contusion, aspiration of gastric content, ventilator-associated pneumonia to name a few) and along with it, some ICUs also target a supra-normal PaO2 and eventually brain tissue O2 pressure >15 mmHg [50, 51].
The avoidance of asynchrony with the ventilator using pharmacological paralysis can decrease the risk of baro- and volu-trauma [52] and more specifically could prevent surges of ICP due to uncoordinated breathing and increased intra-thoracic pressures. The reduction of intra-thoracic pressures could potentially facilitate the jugular venous return adding an additional benefit on ICP control.
Neuromuscular blockers have shown their ability in preventing fluctuations of ICP due to coughing stimulating maneuvres [8–12, 21]. Nevertheless, more invasive procedures, such as fiberoptic bronchoscopy, did not get much benefit from administration of NMBA [20], even though a confounding effect by fluctuating CO2 cannot be excluded.
Another indirect benefit of paralysis is the reduction of O2 consumption (particularly by the respiratory muscles) and of the energy expenditure of patients with TBI [13], which may hold a further small positive effect on the patient with head injury.
During Temperature Management
Pyrexia may result from neuronal dysfunction post-TBI itself, or can be caused by systemic inflammatory response or on-going infections. Fever after head injury is associated with prolonged ICU stay and worsens neurocognitive outcomes [53–55]. Active temperature management is common for pyrexial TBI patients, and the infusion of NMBAs could prevent shivering (and the associated increase in metabolic rate and O2 consumption) [56, 57] while opioids and/or sedatives have the pitfall of cardiovascular instability and reduction in CPP.
Moreover, the cerebral metabolic rate of O2 consumption decreases by about 6 % for each 1 °C during hypothermia [58–60], and the role of therapeutic cooling in TBI patients is currently under investigation in two multicenter clinical studies (“Eurotherm3235” and “POLAR-RCT”) [61, 62].
Effect on Inflammation and Organ Crosstalk
The existence of an “inflammatory crosstalk” with the diffusion of inflammation between anatomically distant organs has been already shown, and the lungs seem to play a major role [63, 64]. On the route of “lung-brain crosstalk”, mechanical ventilation is associated with neurologic impairment and cognitive dysfunction [65], while different aetiologies of head injury can precipitate respiratory distress, i.e., neurogenic pulmonary edema may follow TBI [66], status epilepticus [67], or subarachnoid hemorrhage [68]. The early administration of NMBAs reduces the inflammatory surges associated with mechanical ventilation [69], and this inflammatory modulation could be intriguing for the patients with TBI, although the importance of circulating cytokines in the development of secondary brain injury is still controversial [70].
Potential Side Effects of NMBAs After Traumatic Brain Injury
NMBAs are a relatively safe class of drugs. However, some issues should be highlighted in TBI patients especially in the case of NMBA infusion:
Critical Illness, Weakness, and Weaning
Patients with TBI and raised ICP are mechanically ventilated for prolonged periods, and therefore, at higher risk of developing of critical illness polyneuropathy (CIP) and/or myopathy (CIM), two conditions often coexist and cause prolonged weaning and weakness [16].
The infusion of NMBAs was recognized as risk factor for CIP/CIM, but its role is less certain than thought before [15, 16]. The development of CIP/CIM increases the weaning period by 2- to 7-fold in the general ICU population [18]. Leijten et al. found that 76 % of patients mechanically ventilated longer than 5 days developed electrophysiological neuromuscular abnormalities [71], and the mortality in this group was at least doubled [71, 72]. Few data are available about the weaning of patients with brain injury because they have been excluded from RCTs on weaning strategies [73].
Until the relationship between NMBA and CIP/CIM will be clarified, paralysis should be carefully considered in TBI patients artificially ventilated for prolonged periods. A negative impact on weaning in turn would delay the rehabilitation process, with further negative impact on the neurological recovery [74]. In addition, a severe CIP/CIM may inappropriately instigate unwise pessimistic prognostic impressions.
Diagnosis of Post-traumatic Seizure Activity
NMBAs infusion would result in the difficulty to identify post-traumatic seizure activity, in which occurrence after TBI is relatively frequent [75, 76]. Epileptic activity can be identified by continuous EEG during paralysis, but not all protocols implement a daily EEG monitoring and not all ICUs have the facilities to provide such expert monitoring.
Pharmacokinetic Considerations
NMBAs are hydrophilic drugs and do not cross the blood–brain barrier. Of theoretical importance, the metabolism of the benzylisoquinolines NMBAs (cisatracurium and atracurium) generates laudanosine, an amino alkaloid with epileptogenic activity [77]. A study on anephric cats exposed to high dose of atracurium showed no brain toxicity by laudanosine accumulation [78]. However, a disrupted blood–brain barrier may allow the penetration of NMBA molecules into the brain parenchyma. An animal study investigated the neurotoxicity of NMBAs or laudanosine injected directly into the brain. Steroidal NMBAs (pancuronium and vecuronium) showed epileptogenic effects due to accumulation of cytosolic calcium, while atracurium or laudanosine did not cause shift of calcium nor epileptic activity [79]. A case series from Gwinnutt et al. in patients with severe closed head injury and exposed to atracurium did not find adverse effects attributable to the concentration of laudanosine in the cerebrospinal fluid [80].
Isolated cases of tachyphylaxis in TBI [81] and cross-resistance between steroidal and benzylisoquinolines NMBAs have been reported [82]. Other considerations, such as interaction with other drugs, are likely to be similar to those valid in the general ICU population. Finally, it is worth mentioning that NMBAs are under scrutiny in the general ICU population for a possible association with pulmonary and thrombotic complications; however, the presence of multiple confounding factors in patients with severe trauma makes the study of these complications highly challenging.
Conclusions
Our systematic review did not find satisfactory scientific evidence to support or reject the use of neuromuscular blockage in patients with TBI and increased ICP, which presently depends mainly on clinician’s preference. Non-depolarizing NMBAs could be safer than succinylcholine with regards to their short-term effects on the ICP; however, there is no available evidence of the impact of paralysis on long-term outcome of TBI patients. Among others, the positive effects of NMBAs, such as the facilitation of mechanical ventilation, should be carefully weighed against the potential to harm with continuous paralysis. Large well-designed studies are warranted in order to weigh the risk and benefit of such practice.
References
Fleminger S, Ponsford J. Long term outcome after traumatic brain injury. BMJ (Clinical research ed). 2005;331:1419–20.
Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma. 2007;24(Suppl 1):S55–8.
Helmy A, Vizcaychipi M, Gupta AK. Traumatic brain injury: intensive care management. Br J Anaesth. 2007;99:32–42.
Matta B, Menon D. Severe head injury in the United Kingdom and Ireland: a survey of practice and implications for management. Crit Care Med. 1996;24:1743–8.
Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–16.
Needham CJ, Brindley PG. Best evidence in critical care medicine: the role of neuromuscular blocking drugs in early severe acute respiratory distress syndrome. Can J anaesth. 2012;59:105–8.
Steingrub JS, Lagu T, Rothberg MB, Nathanson BH, Raghunathan K, Lindenauer PK. Treatment with neuromuscular blocking agents and the risk of in-hospital mortality among mechanically ventilated patients with severe sepsis*. Crit Care Med. 2014;42:90–6.
White PF, Schlobohm RM, Pitts LH, Lindauer JM. A randomized study of drugs for preventing increases in intracranial pressure during endotracheal suctioning. Anesthesiology. 1982;57:242–4.
Werba A, Klezl M, Schramm W, et al. The level of neuromuscular block needed to suppress diaphragmatic movement during tracheal suction in patients with raised intracranial pressure: a study with vecuronium and atracurium. Anaesthesia. 1993;48:301–3.
Werba A, Weinstabl C, Petricek W, Plainer B, Spiss CK. [Requisite muscle relaxation using vecuronium for tracheobronchial suction in neurosurgical intensive care patients]. Der Anaesthesist. 1991;40:328–31.
Kerr ME, Sereika SM, Orndoff P, et al. Effect of neuromuscular blockers and opiates on the cerebrovascular response to endotracheal suctioning in adults with severe head injuries. Am J Crit Care. 1998;7:205–17.
Chivite Fernandez N, Martinez Oroz A, Marraco Bonmcompte M, et al. [Intracranial pressure response during secretion aspiration after administration of a muscle relaxant]. Enfermeria intensiva/Sociedad Espanola de Enfermeria Intensiva y Unidades Coronarias 2005;16:143-52.
McCall M, Jeejeebhoy K, Pencharz P, Moulton R. Effect of neuromuscular blockade on energy expenditure in patients with severe head injury. JPEN. 2003;27:27–35.
Annegers JF, Hauser WA, Coan SP, Rocca WA. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338:20–4.
Stevens RD, Dowdy DW, Michaels RK, Mendez-Tellez PA, Pronovost PJ, Needham DM. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med. 2007;33:1876–91.
Latronico N, Bolton CF. Critical illness polyneuropathy and myopathy: a major cause of muscle weakness and paralysis. Lancet Neurol. 2011;10:931–41.
de Jonghe B, Lacherade JC, Sharshar T, Outin H. Intensive care unit-acquired weakness: risk factors and prevention. Crit Care Med. 2009;37:S309–15.
Latronico N, Shehu I, Seghelini E. Neuromuscular sequelae of critical illness. Curr Opin Crit Care. 2005;11:381–90.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed). 2009;339:b2700.
Kerwin AJ, Croce MA, Timmons SD, Maxwell RA, Malhotra AK, Fabian TC. Effects of fiberoptic bronchoscopy on intracranial pressure in patients with brain injury: a prospective clinical study. J Trauma. 2000;48:878–82 discussion 82–3.
Brown MM, Parr MJ, Manara AR. The effect of suxamethonium on intracranial pressure and cerebral perfusion pressure in patients with severe head injuries following blunt trauma. Eur J Anaesthesiol. 1996;13:474–7.
Schramm WM, Jesenko R, Bartunek A, Gilly H. Effects of cisatracurium on cerebral and cardiovascular hemodynamics in patients with severe brain injury. Acta Anaesthesiol Scand. 1997;41:1319–23.
Prielipp RC, Robinson JC, Wilson JA, MacGregor DA, Scuderi PE. Dose response, recovery, and cost of doxacurium as a continuous infusion in neurosurgical intensive care unit patients. Crit Care Med. 1997;25:1236–41.
Minton MD, Grosslight K, Stirt JA, Bedford RF. Increases in intracranial pressure from succinylcholine: prevention by prior nondepolarizing blockade. Anesthesiology. 1986;65:165–9.
Stirt JA, Grosslight KR, Bedford RF, Vollmer D. “Defasciculation” with metocurine prevents succinylcholine-induced increases in intracranial pressure. Anesthesiology. 1987;67:50–3.
Kovarik WD, Mayberg TS, Lam AM, Mathisen TL, Winn HR. Succinylcholine does not change intracranial pressure, cerebral blood flow velocity, or the electroencephalogram in patients with neurologic injury. Anesth Analg. 1994;78:469–73.
Schramm WM, Papousek A, Michalek-Sauberer A, Czech T, Illievich U. The cerebral and cardiovascular effects of cisatracurium and atracurium in neurosurgical patients. Anesth Analg. 1998;86:123–7.
Cafiero T, Razzino S, Mastronardi P, Mazzarella B, De Vivo P. Mivacurium in patients with intracranial pathology. Minerva Anestesiol. 1999;65:81–5.
Di Giugno G, Sanfilippo M, Orfei P, Rosa G. [Myorelaxants and intracranial pressure (ICP) in neurosurgery. Preliminary clinical results of pipecurium bromide (Arduan) on ICP and on cerebral perfusion pressure (CPP)]. Minerva Anestesiol. 1992;58:83–6.
Minton MD, Stirt JA, Bedford RF, Haworth C. Intracranial pressure after atracurium in neurosurgical patients. Anesth Analg. 1985;64:1113–6.
Rosa G, Orfei P, Sanfilippo M, Vilardi V, Gasparetto A. The effects of atracurium besylate (Tracrium) on intracranial pressure and cerebral perfusion pressure. Anesth Analg. 1986;65:381–4.
Rosa G, Sanfilippo M, Orfei P, et al. The effects of pipecuronium bromide on intracranial pressure and cerebral perfusion pressure. J Neurosurg Anesthesiol. 1991;3:253–7.
Rosa G, Sanfilippo M, Vilardi V, Orfei P, Gasparetto A. Effects of vecuronium bromide on intracranial pressure and cerebral perfusion pressure. A preliminary report. Br J Anaesth. 1986;58:437–40.
Schramm WM, Strasser K, Bartunek A, Gilly H, Spiss CK. Effects of rocuronium and vecuronium on intracranial pressure, mean arterial pressure and heart rate in neurosurgical patients. Br J Anaesth. 1996;77:607–11.
Unni VK, Gray WJ, Young HS. Effects of atracurium on intracranial pressure in man. Anaesthesia. 1986;41:1047–9.
Hsiang JK, Chesnut RM, Crisp CB, Klauber MR, Blunt BA, Marshall LF. Early, routine paralysis for intracranial pressure control in severe head injury: is it necessary? Crit Care Med. 1994;22:1471–6.
Juul N, Morris GF, Marshall SB, Marshall LF. Neuromuscular blocking agents in neurointensive care. Acta Neurochir Suppl. 2000;76:467–70.
Cottrell JE, Hartung J, Giffin JP, Shwiry B. Intracranial and hemodynamic changes after succinylcholine administration in cats. Anesth Analg. 1983;62:1006–9.
Thiagarajah S, Sophie S, Lear E, Azar I, Frost EA. Effect of suxamethonium on the ICP of cats with and without thiopentone pretreatment. Br J Anaesth. 1988;60:157–60.
Giffin JP, Hartung J, Cottrell JE, Capuano C, Shwiry B. Effect of vecuronium on intracranial pressure, mean arterial pressure and heart rate in cats. Br J Anaesth. 1986;58:441–3.
Giffin JP, Litwak B, Cottrell JE, Hartung J, Capuano C. Intracranial pressure mean arterial pressure and heart rate after rapid paralysis with atracurium in cats. Can Anaesth Soc J. 1985;32:618–21.
Haigh JD, Nemoto EM, DeWolf AM, Bleyaert AL. Comparison of the effects of succinylcholine and atracurium on intracranial pressure in monkeys with intracranial hypertension. Can Anaesth Soc J. 1986;33:421–6.
Ducey JP, Deppe SA, Foley KT. A comparison of the effects of suxamethonium, atracurium and vecuronium on intracranial haemodynamics in swine. Anaesth Intensive Care. 1989;17:448–55.
Lanier WL, Milde JH, Michenfelder JD. The cerebral effects of pancuronium and atracurium in halothane-anesthetized dogs. Anesthesiology. 1985;63:589–97.
Vesely R, Hoffman WE, Gil KS, Albrecht RF, Miletich DJ. The cerebrovascular effects of curare and histamine in the rat. Anesthesiology. 1987;66:519–23.
Jacka MJ, Zygun D. Survey of management of severe head injury in Canada. Can J Neurol Sci. 2007;34:307–12.
Mehta S, Burry L, Fischer S, et al. Canadian survey of the use of sedatives, analgesics, and neuromuscular blocking agents in critically ill patients. Crit Care Med. 2006;34:374–80.
Rhoney DH, Murry KR. National survey of the use of sedating drugs, neuromuscular blocking agents, and reversal agents in the intensive care unit. J Intensive Care Med. 2003;18:139–45.
Murray MJ, Cowen J, DeBlock H, et al. Clinical practice guidelines for sustained neuromuscular blockade in the adult critically ill patient. Crit Care Med. 2002;30:142–56.
Bohman LE, Heuer GG, Macyszyn L, et al. Medical management of compromised brain oxygen in patients with severe traumatic brain injury. Neurocrit Care. 2011;14:361–9.
Nangunoori R, Maloney-Wilensky E, Stiefel M, et al. Brain tissue oxygen-based therapy and outcome after severe traumatic brain injury: a systematic literature review. Neurocrit Care. 2012;17:131–8.
Slutsky AS. Neuromuscular blocking agents in ARDS. N Engl J Med. 2010;363:1176–80.
Childs C. Human brain temperature: regulation, measurement and relationship with cerebral trauma: part 1. Br J Neurosurg. 2008;22:486–96.
Childs C, Wieloch T, Lecky F, Machin G, Harris B, Stocchetti N. Report of a consensus meeting on human brain temperature after severe traumatic brain injury: its measurement and management during pyrexia. Front Neurol. 2010;1:146.
Li J, Jiang JY. Chinese Head Trauma Data Bank: effect of hyperthermia on the outcome of acute head trauma patients. J Neurotrauma. 2012;29:96–100.
Manthous CA, Hall JB, Olson D, et al. Effect of cooling on oxygen consumption in febrile critically ill patients. Am J Respir Crit Care Med. 1995;151:10–4.
Hata JS, Shelsky CR, Hindman BJ, Smith TC, Simmons JS, Todd MM. A prospective, observational clinical trial of fever reduction to reduce systemic oxygen consumption in the setting of acute brain injury. Neurocrit Care. 2008;9:37–44.
McCullough JN, Zhang N, Reich DL, et al. Cerebral metabolic suppression during hypothermic circulatory arrest in humans. Ann Thorac Surg. 1999;67:1895–9 discussion 919–21.
Nilsson L, Kogure K, Busto R. Effects of hypothermia and hyperthermia on brain energy metabolism. Acta Anaesthesiol Scand. 1975;19:199–205.
Rosomoff HL, Holaday DA. Cerebral blood flow and cerebral oxygen consumption during hypothermia. Am J Physiol. 1954;179:85–8.
Andrews PJ, Sinclair HL, Battison CG, et al. European society of intensive care medicine study of therapeutic hypothermia (32–35 degrees C) for intracranial pressure reduction after traumatic brain injury (the Eurotherm3235Trial). Trials. 2011;12:8.
http://clinicaltrials.gov/ct2/show/NCT00987688. The Prophylactic Hypothermia Trial to Lessen Traumatic Brain Injury (POLAR-RCT). ClinicalTrials.gov Identifier: NCT00987688.
Quilez ME, Lopez-Aguilar J, Blanch L. Organ crosstalk during acute lung injury, acute respiratory distress syndrome, and mechanical ventilation. Curr Opin Crit Care. 2012;18:23–8.
Pelosi P, Rocco PR. The lung and the brain: a dangerous cross-talk. Crit Care (London, England). 2011;15:168.
Morandi A, Brummel NE, Ely EW. Sedation, delirium and mechanical ventilation: the ‘ABCDE’ approach. Curr Opin Crit Care. 2011;17:43–9.
Bahloul M, Chaari AN, Kallel H, et al. Neurogenic pulmonary edema due to traumatic brain injury: evidence of cardiac dysfunction. Am J Crit Care. 2006;15:462–70.
Brambrink AM, Tzanova I. Neurogenic pulmonary edema after generalized epileptic seizure. Eur J Emerg Med. 1998;5:59–66.
Macmillan CS, Grant IS, Andrews PJ. Pulmonary and cardiac sequelae of subarachnoid haemorrhage: time for active management? Intensive Care Med. 2002;28:1012–23.
Forel JM, Roch A, Marin V, et al. Neuromuscular blocking agents decrease inflammatory response in patients presenting with acute respiratory distress syndrome. Crit Care Med. 2006;34:2749–57.
Morganti-Kossmann MC, Rancan M, Stahel PF, Kossmann T. Inflammatory response in acute traumatic brain injury: a double-edged sword. Curr Opin Crit care. 2002;8:101–5.
Leijten FS, Harinck-de Weerd JE, Poortvliet DC, De Weerd AW. The role of polyneuropathy in motor convalescence after prolonged mechanical ventilation. JAMA. 1995;274:1221–5.
Leijten FS, De Weerd AW, Poortvliet DC, De Ridder VA, Ulrich C, Harink-De Weerd JE. Critical illness polyneuropathy in multiple organ dysfunction syndrome and weaning from the ventilator. Intensive Care Med. 1996;22:856–61.
Lazaridis C, DeSantis SM, McLawhorn M, Krishna V. Liberation of neurosurgical patients from mechanical ventilation and tracheostomy in neurocritical care. J Crit Care. 2012;27(417):e1–8.
Andelic N, Bautz-Holter E, Ronning P, et al. Does an early onset and continuous chain of rehabilitation improve the long-term functional outcome of patients with severe traumatic brain injury? J Neurotrauma. 2012;29:66–74.
Temkin NR, Dikmen SS, Winn HR. Management of head injury. Posttraumatic seizures. Neurosurg Clin N Am. 1991;2:425–35.
Yablon SA. Posttraumatic seizures. Arch Phys Med Rehabil. 1993;74:983–1001.
Standaert FG. Magic bullets, science, and medicine. Anesthesiology. 1985;63:577–8.
Ingram MD, Sclabassi RJ, Cook DR, Stiller RL, Bennett MH. Cardiovascular and electroencephalographic effects of laudanosine in “nephrectomized” cats. Br J Anaesth. 1986;58(Suppl 1):14S–8S.
Cardone C, Szenohradszky J, Yost S, Bickler PE. Activation of brain acetylcholine receptors by neuromuscular blocking drugs. A possible mechanism of neurotoxicity. Anesthesiology. 1994;80:1155–61 discussion 29A.
Gwinnutt CL, Eddleston JM, Edwards D, Pollard BJ. Concentrations of atracurium and laudanosine in cerebrospinal fluid and plasma in three intensive care patients. Br J Anaesth. 1990;65:829–32.
Haddad S. Tachyphylaxis to cisatracurium—case reports and literature review. Middle East J Anesthesiol. 2008;19:1079–92.
Fish DN, Singletary TJ. Cross-resistance to both atracurium- and vecuronium-induced neuromuscular blockade in a critically ill patient. Pharmacotherapy. 1997;17:1322–7.
Acknowledgments
The authors thank Professor Nino Stocchetti for his invaluable input in the preparation of the manuscript. We are also grateful to Ms Tatjana Petrinic of the Oxford Bodleian Libraries for her support on literature search and on reference management
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sanfilippo, F., Santonocito, C., Veenith, T. et al. The Role of Neuromuscular Blockade in Patients with Traumatic Brain Injury: A Systematic Review. Neurocrit Care 22, 325–334 (2015). https://doi.org/10.1007/s12028-014-0061-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0061-1