Abstract
Background
Ambroxol has a very high affinity for lung tissues; its concentration is approximately 20 times higher in the lung than in the serum. We aimed to evaluate the effectiveness of high-dose ambroxol (990 mg/day) in the improvement of oxygenation and prevention of postoperative respiratory complications in the patients with acute cervical spinal cord injury (CSCI).
Methods
A total of 61 acute CSCI patients admitted to the Intensive Care Unit (ICU) of our hospital between January 2009 and June 2011 were included in the study. They were graded as ASIA A and ASIA B according to the classification of the American Spinal Injury Association (ASIA) and were randomly divided into two groups: one group received intravenous ambroxol at 990 mg/day for 5 consecutive days after operation; the other group treated without ambroxol served as control. The results of arterial blood gas analysis on postoperative day 3 and 5 and occurrence of pulmonary complications within 5 days after operation were evaluated.
Results
The group treated with high-dose ambroxol showed a lower rate of postoperative pneumonia and hypoxemia within 5 days after operation. On the 3rd and 5th days, the oxygenation index in the high-dose ambroxol group (291.02 ± 34.96 and 301.28 ± 37.69) was significantly higher than in the control group (230.08 ± 26.25 and 253.82 ± 26.26), with significant differences between the two groups (P = 0.045 and 0.041).
Conclusion
Administration of high-dose ambroxol should be considered as an alternative and effective approach to reduce the postoperative respiratory complications and improve the oxygenation status in acute CSCI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ambroxol has a very high affinity for lung tissues; its concentration is approximately 20 times higher in the lung than in the serum. Thus, micromolar concentrations can be achieved in lung tissues quickly after the administration of 1 g ambroxol [1]. Ambroxol significantly reduced the bronchopulmonary complications after chest, upper abdominal, and cardiac surgeries [2–4]. Severe cervical spinal cord injury (CSCI) may result in increased or retained airway secretion, leading to pulmonary complications of atelectasis, hypoxemia, and lung infection. We conducted a randomized clinical trial to assess the influence of postoperative short-term high-dose ambroxol administration (990 mg/day for 5 consecutive days) on the improvement of oxygenation status and reduction of the postoperative pulmonary complications in CSCI patients.
Materials and Methods
This study was approved by the ethics committee of our hospital. All patients gave their informed consent to participate in the study and to use their data in a prospective database.
Patients
Sixty-one patients with acute CSCI who were admitted to the ICU of the Third Hospital of Peking University between January 2009 and June 2011 were included in this study. There were 44 males and 17 females. According to the classification of the American Spinal Injury Association (ASIA), the patients were graded as ASIA A and ASIA B [5].
The causes of injury among the patients were: motor vehicle accident (34), fall (18), and sports injury (9).
The inclusive criteria were: (1) ASIA A and ASIA B in the severity of neurologic injury according to the classification of the ASIA; (2) The highest level of injury is C4-C5; (3) All patients underwent surgical spinal cord decompression and stabilization before admission to the ICU; (4) Cervical spine injuries were confirmed by computed tomography (CT) and magnetic resonance imaging (MRI); (5) All the patients received ventilation for more than 5 consecutive days after admission to the ICU; (6) The patients had no histories of respiratory diseases (bronchial asthma, pulmonary emphysema, chronic bronchitis, chronic obstructive pulmonary disease); and (7) No pulmonary complications were found when admitted to the ICU (pneumonia, atelectasis and neumothorax). Exclusion criteria: The patients with concurrent thoracic injury, abdominal injury, and brain injury were excluded.
The patients were randomly divided into two groups: the high-dose ambroxol group and control group. Intravenous (i.v.) ambroxol was given at a dose of 990 mg/day (dissolved in 500 ml normal saline and infused i.v. consecutively for 4-6 h) in the ambroxol group; and 5% glucose in normal saline was administered i.v. without ambroxol for 4−6 h in the control group. The two groups were treated for 5 consecutive days, respectively. The patients who completed the treatment until the end of the study were evaluated.
The surgical spinal cord decompression and stabilization were performed in all the patients. All patients were transferred to the ICU soon after operation. Mechanical ventilation was established with synchronized intermittent mandatory ventilation using volume-controlled ventilation plus pressure support. Respiratory parameters were: tidal volume 8−12 mL/kg ideal body weight, mandatory respiratory rate 14−16 bpm, FiO2 40−50%, pressure support 12−15 cmH2O, and positive end-expiratory pressure 5−10 cmH2O. Respiratory rate and FiO2 were adjusted according to the arterial blood gas analysis and blood oxygen saturation index.
Postoperative chest radiography was performed within 6 h and on the 6th day after admission to the ICU or at anytime when it is necessary to determine the presence of pneumonia, atelectasis, and other complications. Liver and renal functions were tested in all the patients one hour after admission to the ICU, and retested on the 6th day. Those with abnormal liver and renal functions were excluded.
Postoperative pulmonary complications included pulmonary infection (fever with positive sputum culture and infiltration on chest X-ray), atelectasis, and hypoxemia (SaO2 < 90% for over 30 min). All these complications were assessed by an examiner blinded to patient’s group on chest X-ray and bronchoscopy. The arterial blood gas analysis was performed within one hour in the patients after admission to the ICU and blood oxygen saturation was examined every morning at 6 am. The results of the blood gas analysis at one hour, the postoperative 3rd and 5th days after admission to the ICU were collected. Arterial blood gas tensions were measured using a blood gas analyzer. The oxygenation index (PaO2/FiO2) was calculated according to the results of the arterial blood gas analysis. The results of the three blood gas analyses, including PaO2, PaCO2, and PaO2/FiO2, were compared between the two groups.
Short-term antibiotics pipericillin/sulbactam or cefminox were administered to all the patients to prevent pulmonary infection.
This study aims to assess the effect of postoperative short-term high-dose ambroxol administration (990 mg/day for 5 consecutive days) on the improvement of oxygenation status and reduction of the postoperative pulmonary complications in CSCI patients. We did not carry out a long-term follow-up of patient prognosis.
Statistical Analysis
Statistical analysis was undertaken using SPSS 13.0 statistics package. Data were expressed as mean ± SD. Data were compared with paired-sample t test and Student’s t test, where appropriate. P value <0.05 was considered statistically significant.
Results
There was no change in the severity and level of cervical spinal cord injury examined on the 6th day after surgery as compared with that upon admission to the hospital. All the patients had normal liver and renal functions tested on the 6th day after admission to the ICU. No adverse effects were observed after the high-dose ambroxol administration.
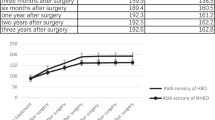
No significant differences were found in patient age, gender, ratio of smokers, the highest level, and the degree of CSCI (ASIA classification) between the two groups. There were no differences in the arterial blood gas, oxygenation index, and rate of pulmonary complications (pneumonia, atelectasis, and hypoxemia). The high-dose ambroxol group showed a lower rate of postoperative pneumonia and hypoxemia than the control group. The results of arterial blood gas analysis on admission, the 3rd and 5th days after operation were not significantly different between the two groups. The oxygenation index on admission showed no difference between the two groups. But the oxygenation index on the 3rd and 5th days after admission to the ICU was higher in the ambroxol group than in the control group ((P = 0.045 and 0.041). Demographic data of the patients and results of the blood gas analysis in both groups are shown in Table 1.
Discussion
Sputum expectoration difficulty is a major factor causing lung infection. Sputum deposition can lead to atelectasis and hypoxemia, which are demonstrated as a decreased oxygenation index in blood gas analysis. Therefore, in this study, we analyzed oxygenation index and incidence of atelectasis, hypoxemia, and lung infection in the CSCI patients in an attempt to study the effect of high-dose ambroxol in prevention and reduction of the above-mentioned pulmonary complications in CSCI patients. It is of great significance to decrease the incidence rate of lung infection and improve the oxygenation status of CSCI patients.
It was reported that in the CSCI patients, the incidence of lung infection can be as high as 40% [6]. Lung infection in the CSCI patients in the first year after injury remains the first cause of death [7]. Some authors have reported that the higher the cervical spinal cord injury level, the higher the incidence of pneumonia, and if the injury level of spinal cord controlling diaphragmatic motor is above C5, the incidence of pneumonia can reach up to 90% [8, 9]. The spinal cord injury in the patients of this study was in the plane of the highest segment C4−C5 while the most important respiratory muscle—diaphragm, is innervated by the phrenic nerve which is formed from the cervical nerves C3−C5. Therefore, the patients with severe and a higher segment level of injury are bed-ridden and usually need a longer time of mechanical ventilation after surgery, which will further increase airway secretions, leading to poor drainage and the sputum deposition in the lower lungs. These factors increase the risk of lung infection. In the early postoperative stage, CSCI patients would rely on regular stand back or vibration equipment to assist expectoration, and by the retention of the artificial airway to suction out the mucus. This is of great significance in the CSCI patients with early expectoration difficulties. Ambroxol helped to reduce the viscosity of the sputum secreted from the bronchial branches and alveoli, making easy the stand back or vibration through sputum expectoration instrument and other auxiliary equipment, thus reducing the atelectasis and hypoxemia because of poor drainage of mucus, and lowering the incidence of lung infection as well.
In this study, no significant difference was found between the high-dose ambroxol group and the control group in the severity and highest level of CSCI (ASIA grade). The arterial blood gas analysis of the patients one hour after transfer into the ICU showed no statistically significant difference in the average values of oxygen partial pressure (PaO2), carbon dioxide partial pressure (PaCO2), and oxygenation index (PaO2/FiO2) between the two groups. On the 3rd and 5th postoperative days, the oxygenation index was significantly higher in the high-dose ambroxol group than in the control group, and the incidence rate of pulmonary complications was significantly lower than in the control group. These results indicate that high-dose ambroxol had a positive effect in improving the oxygenation status and reducing the pulmonary complications in the patients with CSCI.
Because the patients in this study had severe CSCI at C4−C5, they all received mechanical ventilation for more than 5 days. Since the respiratory muscle strength was severely damaged in these patients, the mechanical ventilation parameters were set at a larger tidal volume (in our patients, the tidal volume was set at 8−12 mL/kg ideal body weight). It has been reported that the pressure of mechanical ventilation acted to the lungs can cause lung tissue inflammatory reactions [10, 11]. In vitro experiments have confirmed that the vast majority of alveolar cells in mechanical ventilation, especially when the tidal volume is large, cyclical expansion under positive pressure will produce inflammatory cytokines [12–14]. Three randomized controlled studies in the surgically treated patients have shown that even in the patients without lung injury, more than 10 h of mechanical ventilation may induce lung inflammation [15–18]. This indicates that even a relatively short period of mechanical ventilation may also induce ventilator-associated lung injury. A retrospective study demonstrated that a tidal volume for mechanical ventilation greater than 6 mL/kg is a ventilator-associated independent risk factor for acute lung injury [19]. A series of studies reported that when patients with normal lung function undergo mechanical ventilation in the surgical process, a tidal volume greater than 10 ml/kg can induce early response of inflammation, and may produce adverse effects in some patients [20–22]. There are definite clinical evidences which support the findings that among the ICU patients without acute respiratory distress syndrome (ARDS) before receiving mechanical ventilation, a high tidal volume is considered as an independent factor causing subsequent ARDS [23, 24]. In the present study, we set the tidal volume at > 6 mL/kg, and found that a large tidal volume and prolonged mechanical ventilation are likely to result in lung damage, which affects the patient’s oxygenation status and increases the risk of atelectasis and lung infection development. Ambroxol can directly act on the extracellular free radicals and clearance of free radicals and can inhibit bronchial alveolar macrophages, monocytes and neutrophils to release inflammatory cytokines, histamine, and leukotrienes [25–27]. Animal experiments have also confirmed that ambroxol inhibits lipopolysaccharide (LPS)-induced inflammation in a mouse model of acute lung injury (ALI), reduces lung hemorrhage, edema, exudation, neutrophil infiltration, and other inflammatory reactions [28]. We believe that high doses of ambroxol may reduce the incidence and severity of acute lung injury in the CSCI patients receiving prolonged mechanical ventilation. This study did not verify that inflammatory cytokines were significantly lower in the high-dose ambroxol group than in the control group based on the cytokine levels causing inflammatory reactions, which will be undertaken in our future research. In this study, all the patients had normal liver and renal functions after high-dose ambroxol administration for 5 consecutive days. None of the patients showed adverse effects after high-dose ambroxol administration. It indicates that high-dose ambroxol is safe to those who had normal liver and renal functions before the administration of ambroxol.
In addition, a large number of studies reported in the literature that ambroxol can improve a variety of antibiotics in bronchopulmonary tissue concentration, significantly increase their concentration in bronchial secretions, and makes them remain longer in the lung tissues [29–33], thus playing a positive role in the prevention of lung infection. Recent animal studies have shown that ambroxol has a direct inhibitory effect against Escherichia coli, Pseudomonas aeruginosa, and Staphylococcus aureus, and reduces the number of these bacteria [34–36]. It is suggested that ambroxol may inhibit bronchial pulmonary Pseudomonas aeruginosa. Pseudomonas aeruginosa, and Escherichia coli are known to be the pathogens for ventilator-associated pneumonia in the ICU patients who used ventilator for a long time [37]. Therefore, we conclude that high doses of ambroxol may be helpful in the prevention of ventilator-associated pneumonia caused by prolonged mechanical ventilation.
In this study, the reason why there was no significant difference in the average partial oxygen pressure (PaO2) and carbon dioxide partial pressure (PaCO2) between the two groups, is that we adjusted the tidal volume at a range of 8−12 mL/kg ideal body weight for mechanical ventilation in accordance with patient’s oxygen saturation and blood gas analysis values, inspired oxygen concentration and positive end-expiratory pressure (PEEP) values, and maintained the PaO2 and PaCO2 at a normal range.
In summary, we believe that high-dose ambroxol for the severe CSCI patients after surgery, can effectively assist the drainage of mucus, decrease the rate of acute lung injury because of prolonged mechanical ventilation and prevent ventilator-associated pneumonia through increasing the concentration of antibiotics in the bronchial tissue, thereby reducing the incidence of atelectasis, lung infection and hypoxemia, and improving patients’ oxygenation status. Because the number of patients included in this study is small, more cases are needed to confirm our conclusions.
References
Romanini BM, Sandri MG, Tosi M, Mezzetti M, Mazzetti A. Ambroxol for prophylaxis and treatment of bronchopulmonary complications after chest surgery. Int J Clin Pharmacol Res. 1986;6:123–7.
Fegiz G. Prevention by ambroxol of bronchopulmonary complications after upper abdominal surgery: double-blind Italian multicenter clinical study versus placebo. Lung. 1991;169:69–76.
Refai M, Brunelli A, Xiumé F, Salati M, Sciarra V, Socci L, et al. Short-term perioperative treatment with ambroxol reduces pulmonary complications and hospital costs after pulmonary lobectomy: a randomized trial. Eur J Cardiothorac Surg. 2009;35:469–73.
Ulas MM, Hizarci M, Kunt A, Ergun K, Kocabeyoglu SS, Korkmaz K, et al. Protective effect of Ambroxol on pulmonary function after cardiopulmonary bypass. J Cardiovasc Pharmacol. 2008;52(6):518–23.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26(Suppl 1):S50–6.
Velmahos GC, Toutouzas K, Chan L, Tillou A, Rhee P, Murray J, et al. Intubation after cervical spinal cord injury: to be done selectively or routinely? Am Surg. 2003;69:891–4.
DeVivo MJ, Stover SL. Long-term survival and causes of death. In: Stover SL, Dehisa JA, Whiteneck G, editors. Spinal Cord Injury : Clinical Outcomes from the Model Systems. Gaithersburg: Aspen; 1995. p. 289–316.
Carter RE. Unilateral diaphragmatic paralysis in spinal cord injury patients. Paraplegia. 1980;28:267–73.
Axen K, Pineda H, Shunfenthal I, Haas F. Diaphragmatic function following cervical cord injury : neurally mediated improvement. Arch Phys Med Rehabil. 1985;66:219–22.
Tremblay LN, Slutsky AS. Ventilator-induced injury: from barotrauma to biotrauma. Proc Assoc Am Physicians. 1988;110:482–8.
Vreugdenhil HA, Heijnen CJ, Plötz FB, Zijlstra J, Jansen NJ, Haitsma JJ, Lachmann B, van Vught AJ. Mechanical ventilation of healthy rats suppresses peripheral immune function. Eur Respir J. 2004;23:122–8.
Ericsson CH, Juhász J, Mossberg B, Philipson K, Svartengren M, Camner P. Activation of human macrophages by mechanical ventilation in vitro. Am J Physiol. 1998;275(6 Pt 1):L1040–50.
Vlahakis NE, Schroeder MA, Limper AH, Hubmayr RD. Stretch induces cytokine release by alveolar epithelia cells in vitro. Am J Physiol. 1999;277(1 Pt 1):L167–73.
Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS. Injurious ventilatory strategies increase cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest. 1997;99:944–52.
Wrigge H, Uhlig U, Baumgarten G, Menzenbach J, Zinserling J, Ernst M, Dromann D. Mechanical ventilation strategies and inflammatory responses to cardiac surgery: a prospective randomized clinical trial. Intensive Care Med. 2005;31:1379–87.
Michelet P, D’Journo XB, Roch A, Doddoli C, Marin V, Papazian L, et al. Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology. 2006;105:911–9.
Wolthuis EK, Choi G, Dessing MC, Bresser P, Lutter R, Dzoljic M. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology. 2008;108:46–54.
Parsons PE, Eisner MD, Thompson BT, Matthay MA, Ancukiewicz M, Bernard GR, et al. Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med. 2005;33:1–6.
Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32:1817–24.
Wolthuis EK, Choi G, Dessing MC, Bresser P, Lutter R, Dzoljic M, et al. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology. 2008;108:46–54.
Determann RM, Wolthuis EK, Choi G, Bresser P, Bernard A, Lutter R, et al. Lung epithelial injury markers are not influenced by use of lower tidal volumes during elective surgery in patients without preexisting lung injury. Am J Physiol. 2008;294:L344–50.
Schultz MJ, Haitsma JJ, Slutsky AS, Gajic O. What tidal volumes should be used in patients without acute lung injury? Anesthesiology. 2007;106:1226–31.
Gajic O, Frutos-Vivar F, Esteban A, Hubmayr RD, Anzueto A. Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med. 2005;31:922–6.
Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32:1817–24.
Pfeifer S, Zissel G, Kienast K, Muller-Quernheim J. Reduction of cytokine release from blood and bronchoalveolar mononuclear cells by ambroxol. Eur J Med Res. 1997;2:129–32.
Gibbs BF, Schmutzler W, Vollrath IB, Brosthardt P, Braam U, Wolff HH, et al. Ambroxol inhibits the release of histamine, leukotrienes and cytokines from human leukocytes and mast cells. Inflamm Res. 1999;48:86–93.
Beeh KM, Beier J, Esperester A, Paul LD. Antiinflammatory properties of ambroxol. Eur J Med Res. 2008;13:557–62.
Su X, Wang L, Song Y, Bai C. Inhibition of inflammatory responses by ambroxol, a mucolytic agent, in a murine model of acute lung injury induced by lipopolysaccharide. Intensive Care Med. 2004;30:133–40. [Epub 2003 Sep 20].
Paganin F, Bouvet O, Chanez P, Fabre D, Galtier M, Godard P, et al. Evaluation of the effects of ambroxol on the ofloxacin concentrations in bronchial tissues in COPD patients with infectious exacerbation. Biopharm Drug Dispos. 1995;16:393–401.
Derelle J, Bertolo-Houriez E, Marchal F, Weber M, Virion JM, Vidailhet M. Respiratory evolution of patient with mucoviscidosis treated with mucolytic agents plus domase alfa. Arch-Pediatr. 1998;5:371–7.
Gené R, Poderoso JJ, Corazza C, Lasala MB, Wiemeyer JC, Fernández M, et al. Influence of ambroxol on amoxicillin levels in bronchoalveolar lavage fluid. Arzneimittelforschung. 1987;37:967–8.
Spátola J, Poderoso JJ, Wiemeyer JC, Fernández M, Guerreiro RB, Corazza C. Influence of ambroxol on lung tissue penetration of amoxicillin. Arzneimittelforschung. 1987;37:965–6.
Wiemeyer JC. Influence of ambroxol on the bronchopulmonary level of antibiotics. Arzneimittelforschung. 1981;31:974–6.
Li F, Wang W, Hu L, Li L, Yu J. Effect of Ambroxol on pneumonia caused by Pseudomonas aeruginosa with biofilm formation in an endotracheal intubation rat model. Chemotherapy. 2011;57:173–80. [Epub 2011 April 1].
Lu Q, Yu J, Yang X, Wang J, Wang L, Lin Y, et al. Ambroxol interferes with Pseudomonas aeruginosa quorum sensing. Int J Antimicrob Agents. 2010;36:211–5. [Epub 2010 Jun 26].
Hafez MM, Aboulwafa MM, Yassien MA, Hassouna NA. Activity of some mucolytics against bacterial adherence to mammalian cells. Appl Biochem Biotechnol. 2009;158:97–112. Epub 2008 Aug 12.
Xie DS, Xiong W, Lai RP, Liu L, Gan XM, Wang XH, et al. Ventilator-associated pneumonia in intensive care units in Hubei Province, China: a multicentre prospective cohort survey. J Hosp Infect. 2011;78:284–8. [Epub 2011 April 20].
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Q., Yao, G. & Zhu, X. High-dose Ambroxol Reduces Pulmonary Complications in Patients with Acute Cervical Spinal Cord Injury After Surgery. Neurocrit Care 16, 267–272 (2012). https://doi.org/10.1007/s12028-011-9642-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9642-4