Abstract
Background and aims
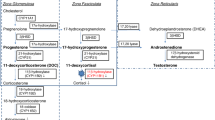
Congenital adrenal hyperplasia (CAH) is a group of disorders that affect the production of steroids in the adrenal gland and are inherited in an autosomal recessive pattern. The clinical and biochemical manifestations of the disorder are diverse, ranging from varying degrees of anomalies of the external genitalia to life-threatening adrenal insufficiency. This multicenter study aimed to determine the demographics, biochemical, clinical, and genetic characteristics besides the current status of adult patients with CAH nationwide.
Methods
The medical records of 223 patients with all forms of CAH were evaluated in the study, which included 19 adult endocrinology clinics. A form inquiring about demographical, etiological, and genetic (where available) data of all forms of CAH patients was filled out and returned by the centers.
Results
Among 223 cases 181 (81.16%) patients had 21-hydroxylase deficiency (21OHD), 27 (12.10%) had 11-beta-hydroxylase deficiency (110HD), 13 (5.82%) had 17-hydroxylase deficiency (17OHD) and 2 (0.89%) had 3-beta-hydroxysteroid-dehydrogenase deficiency. 21OHD was the most prevalent CAH form in our national series. There were 102 (56.4%) classical and 79 (43.6%) non-classical 210HD cases in our cohort. The age of the patients was 24.9 ± 6.1 (minimum-maximum: 17–44) for classical CAH patients and 30.2 ± 11.2 (minimum-maximum: 17–67). More patients in the nonclassical CAH group were married and had children. Reconstructive genital surgery was performed in 54 (78.3%) of classical CAH females and 42 (77.8%) of them had no children. Thirty-two (50.8%) NCAH cases had homogenous and 31 (49.2%) had heterogeneous CYP21A2 gene mutations. V281L pathological variation was the most prevalent mutation, it was detected in 35 (55.6%) of 21OHD NCAH patients.
Conclusion
Our findings are compatible with the current literature except for the higher frequency of 110HD and 17OHD, which may be attributed to unidentified genetic causes. A new classification for CAH cases rather than classical and non-classical may be helpful as the disease exhibits a large clinical and biochemical continuum. Affected cases should be informed of the possible complications they may face. The study concludes that a better understanding of the clinical characteristics of patients with CAH can improve the management of the disorder in daily practice.
Similar content being viewed by others
Data availability
Data can be provided when requested.
References
P.W. H.L,Claahsen-van der Grinten, S.F. Speiser, W. Ahmed, R.J. Arlt, H. Auchus, C.E. Falhammar et al. Congenital adrenal hyperplasia-current insights in pathophysiology, diagnostics, and management. Endocr. Rev. 12, 91–159 (2022). https://doi.org/10.1210/endrev/bnab016
D. El-Maouche, W. Arlt, D.P. Merke, Congenital adrenal hyperplasia. Lancet 390, 2194–2210 (2017). https://doi.org/10.1016/S0140-6736(17)31431-9
P.W. Speiser, W. Arlt, R.J. Auchus, S.L. Baskin, G.S. Conway, D.P. Merke et al. Congenital adrenal hyperplasia due to steroid 21 hydroxylase deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 103, 4043–4088 (2018). https://doi.org/10.1210/jc.2018-01865
D.P. Merke, R.J. Auchus, Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. N. Engl. J. Med 383, 1248–1261 (2020). https://doi.org/10.1056/NEJMra1909786
T. Güran, B. Tezel, M. Çakır, A. Akıncı, Z. Orbak, M. Keskin, B.S. Eklioğlu, A. Ozon, M.N. Özbek, G. Karagüzel, N. Hatipoğlu, F. Gürbüz, F.M. Çizmecioğlu, C. Kara, E. Şimşek, F. Baş, M. Aydın, F. Darendeliler, Neonatal screening for congenital adrenal hyperplasia in Turkey: outcomes of extended pilot study in 241,083 infants. J. Clin. Res Pediatr. Endocrinol. 12, 287–294 (2020). https://doi.org/10.4274/jcrpe.galenos.2020.2019.0182
F. Keleştimur, Y. Sahin, D. Ayata, A. Tutuş A, The prevalence of non-classic adrenal hyperplasia due to 11 beta-hydroxylase deficiency among hirsute women in a Turkish population. Clin. Endocrinol. (Oxf.) 45, 381–384 (1996). https://doi.org/10.1046/j.1365-2265.1996.8150825.x
Y. Sahin, F. Keleştimur, The frequency of late-onset 21-hydroxylase and 11 beta-hydroxylase deficiency in women with polycystic ovary syndrome. Eur. J. Endocrinol. 137, 670–674 (1997). https://doi.org/10.1530/eje.0.1370670
S., Polat, S., Karaburgu, K., Unluhizarci, M., Dundar, Y., Ozkul, Y.K., Arslan, Z., Karaca, F., Kelestimur, Unexpectedly high mutation rate of cyp11b1 compared to cyp21a2 in randomly-selected Turkish women: a large screening study. Endocrinol Invest. (2023). https://doi.org/10.1007/s40618-023-02093-5
A. Nordenström, H. Falhammar, Management of endocrine disease: diagnosis and management of the patient with non-classic CAH due to 21-hydroxylase deficiency. Eur. J. Endocrinol. 180, R127–R145 (2019). https://doi.org/10.1530/EJE-18-0712
M.I. New, Extensive clinical experience: nonclassical 21-hydroxylase deficiency. J. Clin. Endocrinol. Metab. 91, 4205–4214 (2006). https://doi.org/10.1210/jc.2006-1645
K. Hagenfeldt, P.O. Janson, G. Holmdahl, H. Falhammar, H. Filipsson, L. Frisén, M. Thorén, A. Nordenskjöld, Fertility and pregnancy outcome in women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Hum. Reprod. 23, 1607–1613 (2008). https://doi.org/10.1093/humrep/den118
M. Bidet, C. Bellanné-Chantelot, M.B. Galand-Portier, J.L. Golmard, V. Tardy, Y. Morel, S. Clausen, C. Coussieu, P. Boudou, I. Mowzowicz, A. Bachelot, P. Touraine, F. Kuttenn, Fertility in women with nonclassical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J. Clin. Endocrinol. Metab. 95, 1182–1190 (2010). https://doi.org/10.1210/jc.2009-1383
K. Unluhizarci, M. Kula, M. Dundar, F. Tanriverdi, S. Israel, R. Colak, H.S. Dokmetas, H. Atmaca, M. Bahceci, M.K. Balci, A. Comlekci, H. Bilen, E. Akarsu, C. Erem, F. Kelestimur, The prevalence of non-classic adrenal hyperplasia among Turkish women with hyperandrogenism. Gynecol. Endocrinol. 26, 139–143 (2010). https://doi.org/10.3109/09513590903215466
M. Bidet, C. Bellanné-Chantelot, M.B. Galand-Portier, V. Tardy, L. Billaud, K. Laborde, C. Coussieu, Y. Morel, C. Vaury, J.L. Golmard, A. Claustre, E. Mornet, Z. Chakhtoura, I. Mowszowicz, A. Bachelot, P. Touraine, F. Kuttenn, Clinical and molecular characterization of a cohort of 161 unrelated women with nonclassical congenital adrenal hyperplasia due to 21-hydroxylase deficiency and 330 family members. J. Clin. Endocrinol. Metab. 94, 1570–1578 (2009). https://doi.org/10.1210/jc.2008-1582
H.F. Meyer-Bahlburg, C. Dolezal, S.W. Baker, M.I.New,Sexual orientation in women with classical or non-classical congenital adrenal hyperplasia as a function of degree of prenatal androgen excess. Arch. Sex. Behav. 37, 85–99 (2008). https://doi.org/10.1007/s10508-007-9265-1
H. Falhammar, H.F. Nyström, U. Ekström, S. Granberg, A. Wedell, M.Thorén, Fertility, sexuality and testicular adrenal rest tumors in adult males with congenital adrenal hyperplasia. Eur. J. Endocrinol. 166, 441–449 (2012). https://doi.org/10.1530/EJE-11-0828
G. Erdogan, R. Pabuccu, S. Ertek, S. Israel, B. Yilmaz, H. Yilmaz H, G. Caglar, Late-onset congenital adrenal hyperplasia with Cushing syndrome. Intern. Med. 53, 1955–1999 (2014). https://doi.org/10.2169/internalmedicine.53.0654
M. Yildiz, E. Isik, Z.Y. Abali, M. Keskin, M.N. Ozbek, F. Bas et al. Clinical and hormonal profiles correlate with molecular characteristics in patients with 11β-hydroxylase deficiency. J. Clin. Endocrinol. Metab. 18, e3714–e3724 (2021). https://doi.org/10.1210/clinem/dgab225
A. Khattab, S. Haider, A. Kumar, S. Dhawan, D. Alam, R. Romero R et al. Clinical, genetic, and structural basis of congenital adrenal hyperplasia due to 11β-hydroxylase deficiency. Proc. Natl. Acad. Sci. USA1 14, E1933–E1940 (2017). https://doi.org/10.1073/pnas.1621082114
S. Nimkarn, M.I. New, Steroid 11beta-hydroxylase deficiency congenital adrenal hyperplasia. Trends Endocrinol. Metab. 19, 96–99 (2008). https://doi.org/10.1016/j.tem.2008.01.002
M. Zachmann, D. Tassinari, A. Prader, Clinical and biochemical variability of congenital adrenal hyperplasia due to 11 beta-hydroxylase deficiency. A study of 25 patients. J. Clin. Endocrinol. Metab. 56, 222–229 (1983). https://doi.org/10.1210/jcem-56-2-222
P.J. Simm, M.R. Zacharin MR, Successful pregnancy in a patient with severe 11-beta-hydroxylase deficiency and novel mutations in CYP11B1 gene. Horm. Res 68, 294–297 (2007). https://doi.org/10.1159/000107651
N.M. Stikkelbroeck, B.J. Otten, A. Pasic, G.J. Jager, C.G. Sweep, K. Noordam et al. High prevalence of testicular adrenal rest tumors, impaired spermatogenesis, and Leydig cell failure in adolescent and adult males with congenital adrenal hyperplasia. J. Clin. Endocrinol. Metab. 86, 5721–5728 (2001). https://doi.org/10.1210/jcem.86.12.8090
F. Baş, G. Toksoy, B. Ergun-Longmire, Z.O. Uyguner, Z.Y. Abali, Ş. Poyrazoğlu et al. Prevalence, clinical characteristics and long-term outcomes of classical 11 β-hydroxylase deficiency (11BOHD) in Turkish population and novel mutations in CYP11B1 gene. J. Steroid Biochem Mol. Biol. 181, 88–97 (2018). https://doi.org/10.1016/j.jsbmb.2018.04.001
R.J. Auchus, The genetics, pathophysiology, and management of human deficiencies of P450c17. Endocrinol. Metab. Clin. North Am. 30, 101–119 (2001). https://doi.org/10.1016/s0889-8529(08)70021-5
C.E. Kater, E.G. Biglieri, Disorders of steroid 17-hydroxylase deficiency. Endocrinol. Metab. Clin. North Am. 23, 341–357 (1994)
H. Chen, Y. Chen, H. Mao, H. Huang, X. Lou, A novel homozygous CYP17A1 mutation causes partial 17 α-hydroxylase/17,20-lyase deficiency in 46, XX: a case report and literature review. Blood Press 32, 2195008 (2023). https://doi.org/10.1080/08037051.2023.2195008
A.M. Al Alawi, A. Nordenström, H. Falhammar, Clinical perspectives in congenital adrenal hyperplasia due to 3-hydroxysteroid dehydrogenase type 2 deficiency. Endocrine 63, 407–421 (2019). https://doi.org/10.1007/s12020-018-01835-3
Author information
Authors and Affiliations
Contributions
E.E., İ.A., K.Ü. study design, writing and reviewing All authors collected the data and reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Research involving human participants and/or animals
This study was conducted by the guidelines in the Declaration of Helsinki. This article does not contain any studies on human participants or animals performed by any of the authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ertorer, M.E., Anaforoglu, I., Yilmaz, N. et al. Landscape of congenital adrenal hyperplasia cases in adult endocrinology clinics of Türkiye-a nation-wide multicentre study. Endocrine (2024). https://doi.org/10.1007/s12020-024-03799-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12020-024-03799-z