Abstract
Purpose
Antithyroid drugs (ATDs) are effective in controlling hyperthyroidism due to Graves’ disease (GD); however, long-term remission rates are low. The neutrophil-to-lymphocyte ratio (NLR) is a useful prognostic marker in many inflammatory diseases. We aimed to evaluate whether NLR can be used as a prognostic marker for relapse in patients with GD after ATD therapy.
Methods
This retrospective cohort study included 108 patients with newly diagnosed GD who achieved remission after ATD therapy and were followed-up for >12 months after ATD discontinuation. The primary outcome was relapse-free survival (RFS).
Results
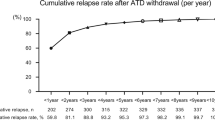
Patients were classified into two groups according to baseline NLR: low NLR group with NLR < 1.14 (n = 59; 55%) and high NLR group with NLR ≥ 1.14 (n = 49; 45%). During the median follow-up of 6.5 years, disease relapse after a year of ATD withdrawal occurred in 23 (21%) patients. The patients with high NLR had poorer RFS than those with low NLR, and RFS curves were significantly different between the two groups (p = 0.002). In multivariate analysis, a high NLR (OR = 4.22, p = 0.016) was an independent prognostic factor for relapse in patients with GD after adjusting for age, sex, goiter, orbitopathy, thyroid hormone levels, thyrotropin binding inhibiting immunoglobulin titer, and the duration of ATD therapy.
Conclusions
This study showed that NLR can be an early and cost-effective prognostic biomarker for relapse in patients with GD after ATD therapy. Further studies are needed to validate the prognostic role of NLR in GD.

Similar content being viewed by others
References
D.S. Ross, H.B. Burch, D.S. Cooper, M.C. Greenlee, P. Laurberg, A.L. Maia, S.A. Rivkees, M. Samuels, J.A. Sosa, M.N. Stan, M.A. Walter, 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. 26(10), 1343–1421 (2016). https://doi.org/10.1089/thy.2016.0229
W.G. Kim, W.B. Kim, G. Woo, H. Kim, Y. Cho, T.Y. Kim, S.W. Kim, M.H. Shin, J.W. Park, H.L. Park, K. Oh, J.H. Chung, Thyroid stimulating hormone reference range and prevalence of thyroid dysfunction in the Korean population: Korea National Health and Nutrition Examination Survey 2013 to 2015. Endocrinol. Metab. 32(1), 106–114 (2017). https://doi.org/10.3803/EnM.2017.32.1.106
H.B. Burch, K.D. Burman, D.S. Cooper, A 2011 survey of clinical practice patterns in the management of Graves’ disease. J. Clin. Endocrinol. Metab. 97(12), 4549–4558 (2012). https://doi.org/10.1210/jc.2012-2802
K.H. Yi, J.H. Moon, I.-J. Kim, H.-S. Bom, J. Lee, W.Y. Chung, J.H. Chung, Y.K. Shong, The diagnosis and management of hyperthyroidism consensus—report of the Korean thyroid association. J. Korean Thyroid Assoc. 6(1), 1–11 (2013)
P. Abraham, A. Avenell, S.C. McGeoch, L.F. Clark, J.S. Bevan, Antithyroid drug regimen for treating Graves’ hyperthyroidism. The Cochrane database of systematic reviews (1), Cd003420 (2010). https://doi.org/10.1002/14651858.CD003420.pub4
P. Anagnostis, F. Adamidou, S.A. Polyzos, S. Katergari, E. Karathanasi, C. Zouli, A. Panagiotou, M. Kita, Predictors of long-term remission in patients with Graves’ disease: a single center experience. Endocrine 44(2), 448–453 (2013). https://doi.org/10.1007/s12020-013-9895-0
E. Mohlin, H. Filipsson Nystrom, M. Eliasson, Long-term prognosis after medical treatment of Graves’ disease in a northern Swedish population 2000–2010. Eur. J. Endocrinol. 170(3), 419–427 (2014). https://doi.org/10.1530/eje-13-0811
S. Park, E. Song, H.S. Oh, M. Kim, M.J. Jeon, W.G. Kim, T.Y. Kim, Y.K. Shong, D.M. Kim, W.B. Kim, When should antithyroid drug therapy to reduce the relapse rate of hyperthyroidism in Graves’ disease be discontinued? Endocrine 65(2), 348–356 (2019). https://doi.org/10.1007/s12020-019-01987-w
S. Chittawar, D. Dutta, Z. Qureshi, V. Surana, S. Khandare, T.N. Dubey, Neutrophil-lymphocyte ratio is a novel reliable predictor of nephropathy, retinopathy, and coronary artery disease in Indians with type-2 diabetes. Indian J. Endocrinol. Metab. 21(6), 864–870 (2017). https://doi.org/10.4103/ijem.IJEM_197_17
A.J. Templeton, M.G. McNamara, B. Seruga, F.E. Vera-Badillo, P. Aneja, A. Ocana, R. Leibowitz-Amit, G. Sonpavde, J.J. Knox, B. Tran, I.F. Tannock, E. Amir, Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J. Natl Cancer Inst. 106(6), dju124 (2014). https://doi.org/10.1093/jnci/dju124
A. Kucuk, A.U. Uslu, Y. Ugan, S. Bagcaci, A.Y. Karahan, A. Akarmut, A. Sahin, S. Kucuksen, Neutrophil-to-lymphocyte ratio is involved in the severity of ankylosing spondylitis. Bratisl. Lekarske Listy 116(12), 722–725 (2015)
Z.A. Ozturk, M.E. Kuyumcu, Y. Yesil, E. Savas, H. Yildiz, Y. Kepekci, S. Ariogul, Is there a link between neutrophil-lymphocyte ratio and microvascular complications in geriatric diabetic patients? J. Endocrinol. Investig. 36(8), 593–599 (2013). https://doi.org/10.3275/8894
I. Kocyigit, E. Eroglu, A. Unal, M.H. Sipahioglu, B. Tokgoz, O. Oymak, C. Utas, Role of neutrophil/lymphocyte ratio in prediction of disease progression in patients with stage-4 chronic kidney disease. J. Nephrol. 26(2), 358–365 (2013). https://doi.org/10.5301/jn.5000152
B. Biondi, L. Bartalena, D.S. Cooper, L. Hegedus, P. Laurberg, G.J. Kahaly, The 2015 European Thyroid Association Guidelines on Diagnosis and Treatment of Endogenous Subclinical Hyperthyroidism. Eur. thyroid J. 4(3), 149–163 (2015). https://doi.org/10.1159/000438750
World Health Organization. Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers, 3rd ed. (2007).
L. Bartalena, L. Baldeschi, A.J. Dickinson, A. Eckstein, P. Kendall-Taylor, C. Marcocci, M.P. Mourits, P. Perros, K. Boboridis, A. Boschi, N. Curro, C. Daumerie, G.J. Kahaly, G. Krassas, C.M. Lane, J.H. Lazarus, M. Marino, M. Nardi, C. Neoh, J. Orgiazzi, S. Pearce, A. Pinchera, S. Pitz, M. Salvi, P. Sivelli, M. Stahl, G. von Arx, W.M. Wiersinga, Consensus statement of the European group on Graves’ orbitopathy (EUGOGO) on management of Graves’ orbitopathy. Thyroid. 18(3), 333–346 (2008). https://doi.org/10.1089/thy.2007.0315
F. Lee, P.S. Yang, M.N. Chien, J.J. Lee, C.H. Leung, S.P. Cheng, An increased neutrophil-to-lymphocyte ratio predicts incomplete response to therapy in differentiated thyroid cancer. Int. J. Med. Sci. 15(14), 1757–1763 (2018). https://doi.org/10.7150/ijms.28498
F. Imtiaz, K. Shafique, S.S. Mirza, Z. Ayoob, P. Vart, S. Rao, Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int. Arch. Med. 5(1), 2 (2012). https://doi.org/10.1186/1755-7682-5-2
R. Zahorec, Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl. Lekarske Listy 102(1), 5–14 (2001)
E. Turan, Evaluation of neutrophil-to-lymphocyte ratio and hematologic parameters in patients with Graves’ disease. Bratisl. lekarske listy 120(6), 476–480 (2019). https://doi.org/10.4149/bll_2019_076
M. Dağdeviren, T. Akkan, D. Yapar, S. Karakaya, T. Dağdeviren, D. Ertuğrul, M. Altay, Can neutrophil/lymphocyte ratio be used as an indicator of inflammation in patients with hyperthyroidism? (2019). https://doi.org/10.2478/jomb-2019-0004
D.L. Eakin, R.L. Peake, G.B. Weiss, Effect of therapy on the neutropenia of hyperthyroidism. South. Med. J. 76(3), 335–337, 340 (1983). https://doi.org/10.1097/00007611-198303000-00017
N. Aggarwal, S.A. Tee, W. Saqib, T. Fretwell, G.P. Summerfield, S. Razvi, Treatment of hyperthyroidism with antithyroid drugs corrects mild neutropenia in Graves’ disease. Clin. Endocrinol. 85(6), 949–953 (2016). https://doi.org/10.1111/cen.13133
K. Van der Weerd, P.M. Van Hagen, B. Schrijver, D.J. Kwekkeboom, W.W. De Herder, M.R. Ten Broek, P.T. Postema, J.J. Van Dongen, F.J. Staal, W.A. Dik, The peripheral blood compartment in patients with Graves’ disease: activated T lymphocytes and increased transitional and pre-naive mature B lymphocytes. Clin. Exp. Immunol. 174(2), 256–264 (2013). https://doi.org/10.1111/cei.12183
H. Keskin, Y. Kaya, K. Cadirci, C. Kucur, E. Ziypak, E. Simsek, H. Gozcu, S. Arikan, A. Carlioglu, Elevated neutrophil-lymphocyte ratio in patients with euthyroid chronic autoimmune thyreotidis. Endocr. Regul. 50(3), 148–153 (2016). https://doi.org/10.1515/enr-2016-0017
C.L. Liu, J.J. Lee, T.P. Liu, Y.C. Chang, Y.C. Hsu, S.P. Cheng, Blood neutrophil-to-lymphocyte ratio correlates with tumor size in patients with differentiated thyroid cancer. J. Surgical Oncol. 107(5), 493–497 (2013). https://doi.org/10.1002/jso.23270
B. McIver, J.C. Morris, The pathogenesis of Graves’ disease. Endocrinol. Metab. Clin. North Am. 27(1), 73–89 (1998)
H.C. Ford, J.M. Carter, The haematology of hyperthyroidism: abnormalities of erythrocytes, leucocytes, thrombocytes and haemostasis. Postgrad. Med. J. 64(756), 735–742 (1988). https://doi.org/10.1136/pgmj.64.756.735
M.J. Kaplan, Role of neutrophils in systemic autoimmune diseases. Arthritis Res. Ther. 15(5), 219 (2013). https://doi.org/10.1186/ar4325
A.J. Klecha, M.L. Barreiro Arcos, L. Frick, A.M. Genaro, G. Cremaschi, Immune-endocrine interactions in autoimmune thyroid diseases. Neuroimmunomodulation 15(1), 68–75 (2008). https://doi.org/10.1159/000135626
D. Villagelin, J.H. Romaldini, R.B. Santos, A.B. Milkos, L.S. Ward, Outcomes in relapsed Graves’ disease patients following radioiodine or prolonged low dose of methimazole treatment. Thyroid 25(12), 1282–1290 (2015). https://doi.org/10.1089/thy.2015.0195
A. Allahabadia, J. Daykin, R.L. Holder, M.C. Sheppard, S.C. Gough, J.A. Franklyn, Age and gender predict the outcome of treatment for Graves’ hyperthyroidism. J. Clin. Endocrinol. Metab. 85(3), 1038–1042 (2000). https://doi.org/10.1210/jcem.85.3.6430
B.G. Nedrebo, P.I. Holm, S. Uhlving, J.I. Sorheim, S. Skeie, G.E. Eide, E.S. Husebye, E.A. Lien, S. Aanderud, Predictors of outcome and comparison of different drug regimens for the prevention of relapse in patients with Graves’ disease. Eur. J. Endocrinol. 147(5), 583–589 (2002)
A.K. Eckstein, H. Lax, C. Losch, D. Glowacka, M. Plicht, K. Mann, J. Esser, N.G. Morgenthaler, Patients with severe Graves’ ophthalmopathy have a higher risk of relapsing hyperthyroidism and are unlikely to remain in remission. Clin. Endocrinol. 67(4), 607–612 (2007). https://doi.org/10.1111/j.1365-2265.2007.02933.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the institutional review board of PNUH, Busan, the Republic of Korea (No. 1906-013-080).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Kim, M., Kim, B.H., Jang, M.H. et al. High neutrophil-to-lymphocyte ratio is associated with relapse in Graves’ disease after antithyroid drug therapy. Endocrine 67, 406–411 (2020). https://doi.org/10.1007/s12020-019-02137-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-02137-y