Abstract
Purpose of Review
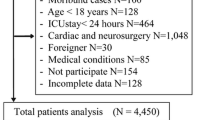
Postoperative delirium (POD) is a common phenomenon among general surgery patients, but it is not well described in urologic surgical patients. We sought to define the incidence and predictive risk factors for POD in patients undergoing urologic surgery.
Recent Findings
Eighteen articles were included for review. The pooled incidence rate of postoperative delirium after urologic surgery was 1.69% (0.69–46.97%). Longer intraoperative time, male sex, unmarried status, and age were shown to be risk factors for POD.
Summary
POD is common after many urologic surgeries and leads to worse postoperative outcomes and higher healthcare utilization. Future studies are needed to better assess for and prevent POD.

Similar content being viewed by others
Data Availability
Data supporting this study are available from corresponding author upon request. All figures and tables are original.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: Author; 2013.
Evered L, Silbert B, Knopman DS, Scott DA, DeKosky ST, Rasmussen LS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. J Alzheimers Dis. 2018;66:1–10.
Martin BJ, Buth KJ, Arora RC, Baskett RJF. Delirium as a predictor of sepsis in post-coronary artery bypass grafting patients: a retrospective cohort study. Crit Care. 2010;14:R171.
Koster S, Hensens AG, van der Palen J. The long-term cognitive and functional outcomes of postoperative delirium after cardiac surgery. Ann Thorac Surg. 2009;87:1469–74. [Internet]. The Society of Thoracic Surgeons; Available from. https://doi.org/10.1016/j.athoracsur.2009.02.080.
Gottesman RF, Grega MA, Bailey MM, Pham LD, Zeger SL, Baumgartner WA, et al. Delirium after coronary artery bypass graft surgery and late mortality. Ann Neurol. 2010;67:338–44.
Sprung J, Roberts RO, Weingarten TN, Nunes Cavalcante A, Knopman DS, Petersen RC, et al. Postoperative delirium in elderly patients is associated with subsequent cognitive impairment. Br J Anaesth. 2017;119:316–23. [Internet]. The Author(s); Available from. https://doi.org/10.1093/bja/aex130.
Robinson TN, Raeburn CD, Tran ZV, Angles EM, Brenner LA, Moss M. Postoperative delirium in the elderly: risk factors and outcomes. Ann Surg. 2009;249:173–8.
Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168:27–32.
Franco K, Litaker D, Locala J, Bronson D. The cost of delirium in the surgical patient. Psychosomatics. 2001;42:68–73.
Rudolph JL, Marcantonio ER. Postoperative delirium: acute change with long-term implications. Anesth Analg. 2011;112:1202–11.
Patel HD, Ball MW, Cohen JE, Kates M, Pierorazio PM, Allaf ME. Morbidity of urologic surgical procedures: an analysis of rates, risk factors, and outcomes. Urology. 2015;85:552–60. [internet]. Elsevier Inc. Available from. https://doi.org/10.1016/j.urology.2014.11.034.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Sterne J, Savović J, Page M, Elbers R, Blencowe N, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. 2019;366:i4898.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Clayton D, Hills M. Statistical methods in epidemiology. Oxford: Oxford University Press; 1993.
Larsen RJ, Marx ML. A introduction to mathematical statistics and its applications. Fifth. Boston: Prentice Hall; 1981.
Braga ILS, Castelo-Filho J, de Sousa Bezerra Pinheiro R, de Azevedo RB, Ponte AT, da Silveira RA, et al. Functional capacity as a predictor of postoperative delirium in transurethral resection of prostate patients in Northeast Brazil. Neuropsychiatr Dis Treat. 2019;15:2395–401.
Dai YT, Lou MF, Yip PK, Huang GS. Risk factors and incidence of postoperative delirium elderly Chinese patients. Gerontology. 2000;46:28–35.
Gani H, Domi R, Kodra N, Prifti P, Naco M, Beqiri V, et al. The incidence of postoperative delirium in elderly patients after urologic surgery. Med Arh. 2013;67:45–7.
Hamann J, Bickel H, Schwaibold H, Hartung R, Förstl H. Postoperative acute confusional state in typical urologic population: incidence, risk factors, and strategies for prevention. Urology. 2005;65:449–53.
Large MC, Reichard C, Williams JTB, Chang C, Prasad S, Leung Y, et al. Incidence, risk factors, and complications of postoperative delirium in elderly patients undergoing radical cystectomy. Urology. 2013;81:123–9. [Internet]. Elsevier Inc.; Available from. https://doi.org/10.1016/j.urology.2012.07.086.
Matsuki M, Tanaka T, Takahashi A, Inoue R, Hotta H, Itoh N, et al. Incidence and risk factors of postoperative delirium in elderly patients undergoing urological surgery: A multi-institutional prospective study. Int J Urol. 2020;27(3):219–225. https://doi.org/10.1111/iju.14172.
Munjupong S, Sripon T, Siripoonyothai S, Jesadapatarakul N, Poojinya T, Chernsirikasem N. Incidence and risk factors of emergence delirium after general and regional anesthesia in elective non-cardiac surgery patients. J Med Assoc Thail. 2018;101:1653–8.
Sato T, Hatakeyama S, Okamoto T, Yamamoto H, Hosogoe S, Tobisawa Y, et al. Slow gait speed and rapid renal function decline are risk factors for postoperative delirium after urological surgery. PLoS One. 2016;11:e0153961.
Tai S, Xu L, Zhang L, Fan S, Liang C. Preoperative risk factors of postoperative delirium after transurethral prostatectomy for benign prostatic hyperplasia. Int J Clin Exp Med. 2015;8:4569–74.
Tognoni P, Simonato A, Robutti N, Pisani M, Cataldi A, Monacelli F, et al. Preoperative risk factors for postoperative delirium (POD) after urological surgery in the elderly. Arch Gerontol Geriatr. 2011;52:e166–9. [internet]. Elsevier Ireland Ltd; Available from. https://doi.org/10.1016/j.archger.2010.10.021.
Xue P, Wu Z, Wang K, Tu C, Wang X. Incidence and risk factors of postoperative delirium in elderly patients undergoing transurethral resection of prostate: a prospective cohort study. Neuropsychiatr Dis Treat. 2016;12:137–42.
Kim HC, Kim E, Jeon YT, Hwang JW, Lim YJ, Seo JH, et al. Postanaesthetic emergence agitation in adult patients after general anaesthesia for urological surgery. J Int Med Res. 2015;43:226–35.
Haugen CE, Mountford A, Warsame F, Berkowitz R, Bae S, Thomas AG, et al. Incidence, risk factors, and sequelae of post-kidney transplant delirium. J Am Soc Nephrol. 2018;29:1752–9.
Bandini M, Marchioni M, Preisser F, Nazzani S, Tian Z, Graefen M, et al. Comprehensive analysis of in-hospital delirium after major surgical oncology procedures: A population-based study. Can Urol Assoc J. 2020;14(3):E84–93. https://doi.org/10.5489/cuaj.6030.
Berian JR, Zhou L, Russell MM, Hornor MA, Cohen ME, Finlayson E, et al. Postoperative delirium as a target for surgical quality improvement. Ann Surg. 2018;268:93–9.
Dhakharia V, Sinha S, Bhaumik J. Postoperative delirium in Indian patients following major abdominal surgery for cancer: risk factors and associations. Indian J Surg Oncol. 2017;8:567–72.
Ha A, Krasnow RE, Mossanen M, Nagle R, Hshieh TT, Rudolph JL, et al. A contemporary population-based analysis of the incidence, cost, and outcomes of postoperative delirium following major urologic cancer surgeries. Urol Oncol Semin Orig Investig. 2018;36:341.e15–22.
Cotoia A, Mirabella L, Beck R, Matrella P, Assenzo V, Hazot TC, et al. Effects of closed-loop intravenous anesthesia guided by bispectral index in adult patients on emergence delirium: a randomized controlled study. Minerva Anestesiol. 2018;84:437–46.
Ravi B, Pincus D, Choi S, Jenkinson R, Wasserstein DN, Redelmeier DA. Association of duration of surgery with postoperative delirium among patients receiving hip fracture repair. JAMA Netw Open. 2019;2(2):e190111. https://doi.org/10.1001/jamanetworkopen.2019.0111.
Wong CL, Holroyd-Leduc J, Simel DL, Straus SE. Does this patient have delirium? value of bedside instruments. JAMA. 2010;304(7):779–86. https://doi.org/10.1001/jama.2010.1182.
Inouye S, Leo-Summer L, Zhang Y, Bogardus S, Leslie D, Agostini J. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53:312–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Ethics Approval
This article is a systematic review of literature and, therefore, there was no direct patient involvement.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
All calculations are available in a supplementary Excel file.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Lower Urinary Tract Symptoms and Voiding Dysfunction
Supplementary Information
Rights and permissions
About this article
Cite this article
Stoddard, M.D., Cho, A., Chen, S.A. et al. A Systematic Review of Postoperative Delirium in the Urologic Patient. Curr Urol Rep 21, 60 (2020). https://doi.org/10.1007/s11934-020-01010-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s11934-020-01010-0