Abstract
Purpose of Review
Women have an estimated 12.6% lifetime risk of undergoing surgery for pelvic organ prolapse in the USA (Wu et al. in Obstet Gynecol 123(6): 1201–6, 2014). Surgical repair of uterovaginal prolapse most commonly includes hysterectomy and vaginal vault suspension; however, the value of concomitant hysterectomy is uncertain, and there appears to be growing interest in uterine conservation. Multiple procedures have evolved using a variety of approaches. The aim of this paper is to review uterine sparing (hysteropexy) prolapse repair techniques and outcomes.
Recent Findings
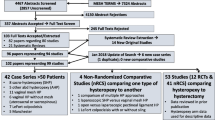
Several randomized controlled trials (RCT) have shown comparable success rates for apical compartment support with sacrospinous hysteropexy as compared to vaginal hysterectomy with uterosacral ligament suspension, with shorter hospitalization and quicker return to work. (Detollenaere et al. in BMJ 351: h3717, 2015); (Dietz et al. in Int Urogynecol J Pelvic Floor Dysfunct 21(2): 209–16, 2010). Available data suggest vaginal mesh hysteropexy is as effective as vaginal mesh with hysterectomy, with lower rates of mesh exposure. (Maher et al., 2017) To date, no RCTs have been published comparing sacral hysteropexy to hysterectomy with sacral colpopexy. Overall, there is a higher reoperation rate for sacral hysteropexy and a higher mesh exposure rate for hysterectomy with sacral colpopexy. (Maher et al., 2017) No RCTs have been published comparing hysteropexy surgical approaches.
Summary
Although hysteropexy data is expanding, there is a need for more information regarding long-term surgical durability, appropriate patient selection, and whether one approach is superior to another.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson FM. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6. https://doi.org/10.1097/AOG.0000000000000286.
Ridgeway BM, Frick AC. Chapter 26: uterine conservation for the surgical treatment of uterovaginal prolapse. In: Walters MD, Karram M, editors. Urogynecology and reconstructive pelvic surgery. Philadelphia: Saunders; 2014. p. 383–99.
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470.e1–6. https://doi.org/10.1016/j.ajog.2013.08.003.
Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD. Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg. 2013;19(2):103–9. https://doi.org/10.1097/SPV.0b013e31827d8667.
DeLancey JO. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol. 1992;166(6 Pt 1):1717–24. https://doi.org/10.1016/0002-9378(92)91562-O.
Ridgeway BM. Does prolapse equal hysterectomy? The role of uterine conservation in women with uterovaginal prolapse. Am J Obstet Gynecol. 2015;213(6):802–9. https://doi.org/10.1016/j.ajog.2015.07.035.
Pearce CL, Stram DO, Ness RB, Stram DA, Roman LD, Templeman C, et al. Population distribution of lifetime risk of ovarian cancer in the United States. Cancer Epidemiol Biomarkers Prev. 2015;24(4):671–6. https://doi.org/10.1158/1055-9965.EPI-14-1128.
Frick AC, Walters MD, Larkin KS, Barber MD. Risk of unanticipated abnormal gynecologic pathology at the time of hysterectomy for uterovaginal prolapse. Am J Obstet Gynecol. 2010;202(5):507 e1–4. https://doi.org/10.1016/j.ajog.2010.01.077.
Parker WH, Feskanich D, Broder MS, Chang E, Shoupe D, Farquhar CM, et al. Long-term mortality associated with oophorectomy compared with ovarian conservation in the nurses’ health study. Obstet Gynecol. 2013;121(4):709–16. https://doi.org/10.1097/AOG.0b013e3182864350.
Lin TY, Su TH, Wang YL, Lee MY, Hsieh CH, Wang KG, et al. Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc = Taiwanyizhi. 2005;104(4):249–53.
Harris WJ. Early complications of abdominal and vaginal hysterectomy. Obstet Gynecol Surv. 1995;50(11):795–805. https://doi.org/10.1097/00006254-199511000-00019.
Farquhar CM, Sadler L, Harvey SA, Stewart AW. The association of hysterectomy and menopause: a prospective cohort study. BJOG. 2005;112(7):956–62. https://doi.org/10.1111/j.1471-0528.2005.00696.x.
•• Maher C, et al. Surgical Treatment of Uterovaginal Prolapse, IV. Committee 15: Pelvic Organ Prolapse Surgery. Incontinence, 6th ed 2017, pages 1874–1886. Editors Abrams, P, Cardoza, L, et al. International Continence Society. Summary of all available paper for all modalities of hysteropexy Tables and references of all prior studies along with critical findings Critical evaluation of the literature with recommendations for best practice based on level of evidence available at the end of the summary.
Fitzgerald MP, Richter HE, Bradley CS, et al. Pelvic support, pelvic symptoms, and patient satisfaction after colpocleisis. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(12):1603–9. https://doi.org/10.1007/s00192-008-0696-6.
Bochenska K, Leader-Cramer A, Mueller M, et al. Perioperative complications following colpocleisis with and without concomitant vaginal hysterectomy. Int Urogynecol J. 2017;28(11):1671–5.
Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow- up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21(2):209–16. https://doi.org/10.1007/s00192-009-1014-7.
Jeng CJ, Yang YC, Tzeng CR, Shen J, Wang LR. Sexual functioning after vaginal hysterectomy or transvaginal sacrospinous uterine suspension for uterine prolapse: a comparison. J Reprod Med. 2005;50(9):669–74.
Hefni M, El-Toukhy T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol. 2003;188(3):645–50. https://doi.org/10.1067/mob.2003.75.
Maher CF, Cary MP, Slack MC, Murray CJ, Milligan M, Schluter P. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(6):381–4. https://doi.org/10.1007/s001920170017.
van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH. Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(5):350–5; discussion 5. https://doi.org/10.1007/s00192-003-1084-x.
Hefni MA, El-Toukhy TA. Long-term outcome of vaginal sacrospinous colpopexy for marked uterovaginal and vault prolapse. Eur J Obstet Gynecol Reprod Biol. 2006;127(2):257–63.
Morley GW, DeLancey JO. Sacrospinous ligament fixation for eversion of the vagina. Am J Obstet Gynecol. 1988;158(4):872–81. https://doi.org/10.1016/0002-9378(88)90088-9.
Morgan DM, Rogers MAM, Huebner M, Wei JT, DeLancey JO. Heterogeneity in anatomic outcome of sacrospinous ligament fixation for prolapse: a systematic review. Obstet Gynecol. 2007;109(6):1424–33. https://doi.org/10.1097/01.AOG.0000264066.89094.21.
Rosen DMSA, Cario GM, Carlton MA, Chou D. Is hysterectomy necessary for laparoscopic pelvic floor repair? J Minim Invasive Gynecol. 2008;15(6):729–34. https://doi.org/10.1016/j.jmig.2008.08.010.
Diwan ARC, Strohsnitter WC, Weld A, Rosenblatt P, Kohli N. Laparoscopic uterosacral ligament uterine suspension compared with vaginal hysterectomy with vaginal vault suspension for uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(1):79–83. https://doi.org/10.1007/s00192-005-1346-x.
Bedford ND, Seman EI, O'Shea RT, Keirse MJ. Effect of uterine preservation on outcome of laparoscopic uterosacral suspension. J Minim Invasive Gynecol. 2013;20(2):172–7. https://doi.org/10.1016/j.jmig.2012.10.014.
Romanzi LJ, Tyagi R. Hysteropexy compared to hysterectomy for uterine prolapse surgery: does durability differ? Int Urogynecol J. 2012;23(5):625–31. https://doi.org/10.1007/s00192-011-1635-5.
Maher C, Schmid C, Baessler K, Feiner B. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;(4):CD004014. https://doi.org/10.1002/14651858.CD004014.pub5.
Haya N, Baessler K, Christmann-Schmid C, de Tayrac R, Dietz V, Guldberg R, et al. Prolapse and continence surgery in countries of the Organization for Economic Cooperation and Development in 2012. Am J Obstet Gynecol. 2015;212(6):755 e1–e27. https://doi.org/10.1016/j.ajog.2015.02.017.
Huang KHCF, Fu HC, Kung FT. Polypropylene mesh as an alternative option for uterine preservation in pelvic reconstruction in patients with uterine prolapse. J Obstet Gynaecol Res. 2012;38(1):97–101. https://doi.org/10.1111/j.1447-0756.2011.01647.x.
Neuman M, Lavy Y. Conservation of the prolapsed uterus is a valid option: medium term results of a prospective comparative study with the posterior intravaginal slingoplasty operation. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(8):889–93. https://doi.org/10.1007/s00192-006-0262-z.
Chu LC, Chuang FC, Kung FT, Huang KH. Comparison of short-term outcomes following pelvic reconstruction with perigee and apogee systems: hysterectomy or not? Int Urogynecol J. 2012;23(1):79–84. https://doi.org/10.1007/s00192-011-1513-1.
Vu MK, Letko J, Jirschele K, Gafni-Kane A, Nguyen A, Du H, et al. Minimal mesh repair for apical and anterior prolapse: initial anatomical and subjective outcomes. Int Urogynecol J. 2012;23(12):1753–61. https://doi.org/10.1007/s00192-012-1780-5.
Roovers J, van der Vaart C, van der Bom J, van Leeuwen J, Scholten P, Heintz A. A randomized controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG. 2004;111(1):50–6. https://doi.org/10.1111/j.1471-0528.2004.00001.x.
Rahmanou P, Price N, Jackson SR. Laparoscopic hysteropexy versus vaginal hysterectomy for the treatment of uterovaginal prolapse: a prospective randomized pilot study. Int Urogynecol J. 2015;26(11):1687–94. https://doi.org/10.1007/s00192-015-2761-2.
Costantini E, Mearini L, Bini V, Zucchi A, Mearini E, Porena M. Uterus preservation in surgical correction of urogenital prolapse. Eur Urol. 2005;48(4):642–9. https://doi.org/10.1016/j.eururo.2005.04.022.
Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A. Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J. 2013;24(9):1481–7. https://doi.org/10.1007/s00192-012-2041-3.
Pan K, Cao L, Ryan NA, Wang Y, Xu H. Laparoscopic sacral hysteropexy versus laparoscopic sacrocolpopexy with hysterectomy for pelvic organ prolapse. Int Urogynecol J. 2016;27(1):93–101. https://doi.org/10.1007/s00192-015-2775-9.
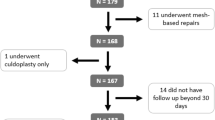
Kow N, Goldman HB, Ridgeway B. Uterine conservation during prolapse repair: 9-year experience at a single institution. Female Pelvic Med Reconstruct Surg. 2016;22(3):126–31. https://doi.org/10.1097/SPV.0000000000000221.
• Gutman RE, Rardin CR, Sokol ER, Matthews C, Park AJ, Iglesia CB, et al. Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 2017;216(1):38.e1–11. Well-designed cohort study and the only prospective study comparing efficacy and adverse effects of two hysteropexy approaches outcomes at 12 months of subjective, objective, and composite criteria. https://doi.org/10.1016/j.ajog.2016.08.035.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
Sarah Bradley, Robert E. Gutman, and Lee A. Richter each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Female Urology
Rights and permissions
About this article
Cite this article
Bradley, S., Gutman, R.E. & Richter, L.A. Hysteropexy: an Option for the Repair of Pelvic Organ Prolapse. Curr Urol Rep 19, 15 (2018). https://doi.org/10.1007/s11934-018-0765-4
Published:
DOI: https://doi.org/10.1007/s11934-018-0765-4