Abstract
Purpose of Review
The association between mental health, pain, and treatment-resistant hypertension is an important consideration for treating physicians. We review and discuss the connection between conditions of anxiety, depression, and chronic pain and their effect on uncontrolled hypertension.
Recent Findings
There is significant co-occurrence of hypertension with anxiety, depression, and chronic pain which may lead to undertreatment of hypertension and undertreatment of the underlying mental health disorder. The association between mental health and hypertension is complex and is modulated by physiologic and environmental factors.
Summary
Physicians treating patients with hypertension should be cognizant of the role anxiety, depression, and chronic pain play in treatment efficacy and compliance. Patients undergoing treatment should be screened for mental health disorders at treatment initiation and frequently thereafter to ensure optimal overall health and compliance.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Centers for Disease Control and Prevention (CDC). Hypertension cascade: hypertension prevalence, treatment and control estimates among US adults aged 18 years and older applying the criteria from the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2013–2016. Atlanta, GA: US Department of Health and Human Services; 2019 [cited 2020 May 8]. Available from: https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html. Accessed 7 Nov 2020. This report shows a break down in treatment modalities for American patients with hypertension and the large proportion of those patients who continue to have uncontrolled hypertension according the American College of Cardiology and American Heart Association’s (ACC/AHA) 2017 hypertension clinical practice guidelines.
Özpelit ME, Özpelit E, Doğan NB, Pekel N, Ozyurtlu F, Yılmaz A, et al. Impact of anxiety level on circadian rhythm of blood pressure in hypertensive patients. Int J Clin Exp Med. 2015;8(9):16252–8.
Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol. 2010;56(1):38–46.
Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27(23):2763–74.
Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–27.
Player MS, Mainous AG, Carnemolla M. Anxiety and unrecognized high blood pressure in U.S. ambulatory care settings: an analysis of the 2005 National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey. Int J Psychiatry Med. 2008;38(1):91–101.
Abeetha S, Sureka V, Brinda S, Ganesh M, Olickel J, Sujatha S. Prevalence of prehypertension and its association with levels of stress and anxiety among students of various disciplines in Chennai - a cross-sectional study. Natl J Physiol Pharm Pharmacol. 2018;8(9):1.
Ismail Z, Mohamad M, Isa MR, Fadzil MA, Yassin SM, Ma KT, et al. Factors associated with anxiety among elderly hypertensive in primary care setting. J Ment Health. 2015;24(1):29–32.
Yuzkat N, Soyalp C, Turk O, Keskin S, Gulhas N. Effects of showing the operating room on preoperative anxiety and hemodynamics among patients with hypertension: A randomized controlled trial. Clin Exp Hypertens. 2020;42(6):553–8.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and Management of high blood pressure in adults. J Am Coll Cardiol. 2018;71(19):e127–248.
Hamrah MS, Hamrah MH, Ishii H, Suzuki S, Hamrah MH, Hamrah AE, et al. Anxiety and depression among hypertensive outpatients in Afghanistan: a cross-sectional study in Andkhoy City. Int J Hypertens. 2018;2018:1–8.
• Schmieder RE, Grassi G, Kjeldsen SE. Patients with treatment-resistant hypertension report increased stress and anxiety: a worldwide study. J Hypertens. 2013;31(3):610–5; discussion 615. This study highlights the emotional impact that uncontrolled and treatment-resistant hypertension have on patients overall mental well-being.
Emre N, Topal K, Edirne T, Gereklioğlu Ç. Factors affecting risk of anxiety and depression among diabetic and hypertensive patients who refer to family health centers. Int J Diabetes Dev Ctries. 2018;38(3):305–11.
Lambert E, Dawood T, Straznicky N, Sari C, Schlaich M, Esler M, et al. Association between the sympathetic firing pattern and anxiety level in patients with the metabolic syndrome and elevated blood pressure. J Hypertens. 2010;28(3):543–50.
Johansen A, Holmen J, Stewart R, Bjerkeset O. Anxiety and depression symptoms in arterial hypertension: the influence of antihypertensive treatment. The HUNT study, Norway. Eur J Epidemiol. 2012;27(1):63–72.
Pickering TG. How common is white coat hypertension? JAMA. 1988;259(2):225–8.
Spruill TM, Pickering TG, Schwartz JE, Mostofsky E, Ogedegbe G, Clemow L, et al. The impact of perceived hypertension status on anxiety and the white coat effect. Ann Behav Med. 2007;34(1):1–9.
Murata T, Narita K, Hamada T, Takahashi T, Omori M, Yoshida H, et al. White coat phenomenon, anxiety and endothelial function in healthy normotensive elderly subjects. Blood Press. 2006;15(2):88–92.
Fang C, Lei J, Zhou S, Zhang Y, Yuan G, Wang J. Association of higher resistin levels with inflammatory activation and endothelial dysfunction in patients with essential hypertension. Chin Med J. 2013;126(4):646–9.
Ademola A, Boima V, Odusola A, Agyekum F, Nwafor C, Salako B. Prevalence and determinants of depression among patients with hypertension: a cross-sectional comparison study in Ghana and Nigeria. Niger J Clin Pract. 2019;22(4):558.
Mushtaq M, Najam N. Depression, anxiety, stress and demographic determinants of hypertension disease. Pak J Med Sci. 2014;30(6):1293–8.
Rantanen AT, Korkeila JJA, Löyttyniemi ES, Saxén UKM, Korhonen PE. Awareness of hypertension and depressive symptoms: a cross-sectional study in a primary care population. Scand J Prim Health Care. 2018;36(3):323–8.
Peng L, Bi S, Liu X, Long T, Zhao Y, Li F, et al. Association between depressive symptoms and arterial stiffness: a cross-sectional study in the general Chinese population. BMJ Open. 2020;10(2):e033408.
Crookes DM, Demmer RT, Keyes KM, Koenen KC, Suglia SF. Depressive symptoms, antidepressant use, and hypertension in young adulthood. Epidemiology. 2018;29(4):547–55.
• Hennein R, Hwang S-J, Au R, Levy D, Muntner P, Fox CS, et al. Barriers to medication adherence and links to cardiovascular disease risk factor control: the Framingham Heart Study. Intern Med J. 2018;48(4):414–21 This study used data from the Framingham Heart Study to show that depressive symptoms may act as a barrier to medication compliance.
MacEwan JP, Silverstein AR, Shafrin J, Lakdawalla DN, Hatch A, Forma FM. Medication adherence patterns among patients with multiple serious mental and physical illnesses. Adv Ther. 2018;35(5):671–85.
Kretchy IA, Owusu-Daaku FT, Danquah SA. Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int J Ment Heal Syst. 2014;8:25.
Giummarra MJ, Tardif H, Blanchard M, Tonkin A, Arnold CA. Hypertension prevalence in patients attending tertiary pain management services, a registry-based Australian cohort study. PLoS One. 2020;15(1):e0228173.
•• Poon SJ, Roumie CL, O'Shea CJ, Fabbri D, R Coco J, Collins SP, et al. Association of elevated blood pressure in the emergency department with chronically elevated blood pressure. J Am Heart Assoc. 2020;9(12):e015985. This study shows that patients with no history of hypertension who present to the ED and are found to have elevated blood pressure, regardless of chief complaint, are likely to have elevated blood pressure in the year following their ED visit.
Bruehl S, Burns JW, Chung OY, Magid E, Chont M, Gilliam W, et al. Hypoalgesia associated with elevated resting blood pressure: evidence for endogenous opioid involvement. J Behav Med. 2010;33(2):168–76.
Ring C, France CR, al’Absi M, Edwards L, McIntyre D, Carroll D, et al. Effects of naltrexone on electrocutaneous pain in patients with hypertension compared to normotensive individuals. Biol Psychol. 2008;77(2):191–6.
Bruehl S, Chung OY, Ward P, Johnson B, McCubbin JA. The relationship between resting blood pressure and acute pain sensitivity in healthy normotensives and chronic back pain sufferers: the effects of opioid blockade. Pain. 2002;100(1–2):191–201.
Ghione S. Hypertension-associated hypalgesia: evidence in experimental animals and humans, pathophysiological mechanisms, and potential clinical consequences. Hypertension. 1996;28(3):494–504.
Sitsen JMA, de Jong W. Observations on pain perception and hypertension in spontaneously hypertensive rats. Clin Exp Hypertens A. 1984;6(7):1345–56.
• Saccò M, Meschi M, Regolisti G, Detrenis S, Bianchi L, Bertorelli M, et al. The relationship between blood pressure and pain. J Clin Hypertens (Greenwich). 2013;15(8):600–5 This review discusses the pathophysiological mechanisms underlying pain and chronic hypertension.
Randich A, Maixner W. Interactions between cardiovascular and pain regulatory systems. Neurosci Biobehav Rev. 1984;8(3):343–67.
Bruehl S, Chung OY, Jirjis JN, Biridepalli S. Prevalence of clinical hypertension in patients with chronic pain compared to nonpain general medical patients. Clin J Pain. 2005;21(2):147–53.
Saavedra JM. Naloxone reversible decrease in pain sensitivity in young and adult spontaneously hypertensive rats. Brain Res. 1981;209(1):245–9.
Schobel HP, Handwerker HO, Schmieder RE, Heusser K, Dominiak P, Luft FC. Effects of naloxone on hemodynamic and sympathetic nerve responses to pain in normotensive vs. borderline hypertensive men. J Auton Nerv Syst. 1998;69(1):49–55.
Guasti L, Zanotta D, Diolisi A, Garganico D, Simoni C, Gaudio G, et al. Changes in pain perception during treatment with angiotensin converting enzyme-inhibitors and angiotensin II type 1 receptor blockade. J Hypertens. 2002;20(3):485–91.
Chung OY, Bruehl S, Diedrich L, Diedrich A. The impact of blood pressure and baroreflex sensitivity on wind-up. Anesth Analg. 2008;107(3):1018–25.
Bruehl S, Olsen RB, Tronstad C, Sevre K, Burns JW, Schirmer H, et al. Chronic pain-related changes in cardiovascular regulation and impact on comorbid hypertension in a general population: the Tromsø study. Pain. 2018;159(1):119–27.
Tracy LM, Ioannou L, Baker KS, Gibson SJ, Georgiou-Karistianis N, Giummarra MJ. Meta-analytic evidence for decreased heart rate variability in chronic pain implicating parasympathetic nervous system dysregulation. Pain. 2016;157(1):7–29.
Bruehl S, McCubbin JA, Harden RN. Theoretical review: altered pain regulatory systems in chronic pain. Neurosci Biobehav Rev. 1999;23(6):877–90.
Ring C, France CR, al’Absi M, Beesley L, Edwards L, McIntyre D, et al. Effects of opioid blockade with naltrexone and distraction on cold and ischemic pain in hypertension. J Behav Med. 2007;30(1):59–68.
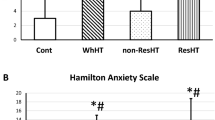
•• Kruk PJ, Nowicki M. Effect of the physical activity program on the treatment of resistant hypertension in primary care. Prim Health Care Res Dev. 2018;19(6):575–83. This study shows that regular exercise improves pain and anxiety and reduces blood pressure in patients with treatment-resistant hypertension, which can be a beneficial adjunct in the treatment plan of these patients.
Wang Y, Metri KG, Singh A, Raghuram N. Immediate effect of mind sound resonance technique (MSRT - a yoga-based relaxation technique) on blood pressure, heart rate, and state anxiety in individuals with hypertension: a pilot study. J Complement Integr Med. 2018;17(2).
Hagins M, States R, Selfe T, Innes K. Effectiveness of yoga for hypertension: systematic review and meta-analysis. Evid Based Complement Alternat Med. 2013;2013:1–13.
Jefferson LL. Exploring effects of therapeutic massage and patient teaching in the practice of diaphragmatic breathing on blood pressure, stress, and anxiety in hypertensive African-American women: an intervention study. J Natl Black Nurses Assoc. 2010;21(1):17–24.
Li L, Zhang K, Shi N. Effects of the traditional Chinese auricular point therapy combined with relaxation training on patients with hypertension and anxiety. Biomed Res India. 2017;28(12):5224–8.
Yang J, Chen J, Yang M, Yu S, Ying L, Liu GJ, et al. Acupuncture for hypertension. Cochrane Database Syst Rev. 2018;11(11):CD008821.
Serafini G, Pompili M, Innamorati M, Iacorossi G, Cuomo I, Della Vista M, et al. The impact of anxiety, depression, and suicidality on quality of life and functional status of patients with congestive heart failure and hypertension: an observational cross-sectional study. Prim Care Companion J Clin Psychiatry. 2010;12(6).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Hypertension and Emergency Medicine
Rights and permissions
About this article
Cite this article
Hamam, M.S., Kunjummen, E., Hussain, M.S. et al. Anxiety, Depression, and Pain: Considerations in the Treatment of Patients with Uncontrolled Hypertension. Curr Hypertens Rep 22, 106 (2020). https://doi.org/10.1007/s11906-020-01117-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s11906-020-01117-2