Abstract
Contact with the criminal justice system, including incarceration, is a common experience for many people living with HIV/AIDS. Optimism has recently been expressed that correctional facilities could be important locations for treatment-as-prevention (TasP)-based initiatives. We review recent findings regarding the effect of incarceration on patterns of HIV transmission, testing, treatment initiation and retention. We found that the prevalence of HIV infection among incarcerated individuals remains higher than analogous non-incarcerated populations. Recent studies have shown that voluntary HIV/AIDS testing is feasible in many correctional facilities, although the number of previously undiagnosed individuals identified has been modest. Studies have implied enhanced linkage to HIV/AIDS treatment and care in jails in the United States was associated with improvements in the HIV cascade of care. However, for many individuals living with HIV/AIDS, exposure to the correctional system remains an important barrier to retention in HIV/AIDS treatment and care. Future research should evaluate structural interventions to address these barriers and facilitate the scale-up of TasP-based efforts among individuals living in correctional settings.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Macalino GE, Vlahov D, Sanford-Colby S, Patel S, Sabin K, Salas C, et al. Prevalence and incidence of HIV, hepatitis B virus, and hepatitis C virus infections among males in Rhode Island prisons. Am J Public Health. 2004;94:1218–23.
Rotily M, Weilandt C, Bird SM, Käll K, Van Haastrecht HJ, Iandolo E, et al. Surveillance of HIV infection and related risk behaviour in European prisons. A multicentre pilot study. Eur J Pub Health. 2001;11:243–50.
Allwright S. Prevalence of antibodies to hepatitis B, hepatitis C, and HIV and risk factors in Irish prisoners: results of a national cross sectional survey. BMJ. 2000;321:78–82.
Amiya RM, Cope JE, Poudel KC, Jimba M. At the intersection of public health and criminal justice systems. Lancet. 2013;381:534.
Centers for Disease Control and Prevention (CDC). HIV transmission among male inmates in a state prison system--Georgia, 1992-2005. MMWR Morb Mortal Wkly Rep. 2006;55:421–6.
Dolan KA, Wodak A. HIV transmission in a prison system in an Australian State. Med J Aust. 1999;171:14–7.
Taylor A, Goldberg D, Emslie J, Wrench J, Gruer L, Cameron S, et al. Outbreak of HIV infection in a Scottish prison. BMJ. 1995;310:289–92.
Zack B. Correctional health and the HIV stages of care. J Correct Health Care. 2013;19:229–30.
Jürgens R, Nowak M, Day M. HIV and incarceration: prisons and detention. J Int AIDS Soc. 2011;14:26. The most comprehensive review of the epidemiological, clinical and policy implications of incarceration among individuals living with/at risk of HIV.
Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376:367–87.
Walmsley R. World prison population list. 9th ed. Essex: International Centre for Prison Studies; 2013. p. 1–6.
Incarceration and crime: a complex relationship. Washington, DC: The Sentencing Project; 2005; pp. 1–11.
Blumstein A, Beck AJ. Population growth in US prisons, 1980-1996. Crime Just. 1999;26:17.
West H, Sabol WJ, Greenman S. Prisoners in 2009. Washington, DC: United States Department of Justice; 2011. p. 1–38.
Rich JD, Diclemente R, Levy J, Lyda K, Ruiz MS, Rosen DL, et al. Correctional facilities as partners in reducing HIV disparities. J Acquir Immune Defic Syndr. 2013;63 Suppl 1:S49–53. An important call from leading US-based researchers into correctional health to engage correctional facilities in addressing HIV/AIDS-associated disparities.
Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA J Am Med Assoc. 2009;301:183–90.
Westergaard RP, Spaulding AC, Flanigan TP. HIV among persons incarcerated in the USA: a review of evolving concepts in testing, treatment, and linkage to community care. Curr Opin Infect Dis. 2013;26:10–6. A review of seek, test, treat and retain campaigns among incarcerated individuals in the United States.
Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4:A16–21.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505.
Montaner JSG, Lima VD, Barrios R, Yip B, Wood E, Kerr T, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376:532–9.
Granich R, Kahn JG, Bennett R, Holmes CB, Garg N, Serenata C, et al. Expanding ART for treatment and prevention of HIV in South Africa: estimated cost and cost-effectiveness 2011-2050. PLoS ONE. 2012;7:e30216.
Montaner JSG, Hogg R, Wood E, Kerr T, Tyndall M, Levy AR, et al. The case for expanding access to highly active antiretroviral therapy to curb the growth of the HIV epidemic. Lancet. 2006;368:531–6.
Draine J, Ahuja D, Altice FL, Arriola KJ, Avery AK, Beckwith CG, et al. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. Aids Care Psychol Socio-Med Asp Aids-Hiv. 2011;23:366–77.
Westergaard RP, Kirk GD, Richesson DR, Galai N, Mehta SH. Incarceration predicts virologic failure for HIV-infected injection drug users receiving antiretroviral therapy. Clin Infect Dis. 2011;53:725–31.
Milloy M-J, Kerr T, Bangsberg DR, Buxton J, Parashar S, Guillemi S, et al. Homelessness as a structural barrier to effective antiretroviral therapy among HIV-seropositive illicit drug users in a Canadian setting. AIDS Patient Care STDS. 2012;26:60–7.
Clatts MC, Rodriguez-Diaz CE, Garcia H, Vargas-Molina RL, Jovet-Toledo GG, Goldsamt LA. Preliminary evidence of significant gaps in continuity of HIV care among excarcerated populations in Puerto Rico. J Int Assoc Physicians AIDS Care (JIAPAC). 2011;10:339–41.
Milloy MJ, Montaner J, Wood E. Barriers to HIV treatment among people who use injection drugs: implications for ‘treatment as prevention”. Curr Opin HIV AIDS. 2012;7:332–8.
Rich JD, Dickinson BP, Macalino G, Flanigan TP, Towe CW, Spaulding A, et al. Prevalence and incidence of HIV among incarcerated and reincarcerated women in Rhode Island. JAIDS J Acquir Immune Defic Syndr. 1999;22:161–6.
Burattini M, Massad E, Rozman M, Azevedo R, Carvalho H. Correlation between HIV and HCV in Brazilian prisoners: evidence for parenteral transmission inside prison. Rev Saude Publica. 2000;34:431–6.
Tyndall MW, Currie S, Spittal P, Li K, Wood E, O’shaughnessy MV, et al. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS. 2003;17:887–93.
Choopanya K, Jarlais Des DC, Vanichseni S, Kitayaporn D, Mock PA, Raktham S, et al. Incarceration and risk for HIV infection among injection drug users in Bangkok. JAIDS J Acquir Immune Defic Syndr. 2002;29:86–94.
Reekie JM, Levy MH, Richards AH, Wake CJ, Siddall DA, Beasley HM, et al. Trends in HIV, hepatitis B and hepatitis C prevalence among Australian prisoners - 2004, 2007, 2010. Med J Aust. 2014;200:277–80.
Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, Altice FL. Burden of infectious diseases, substance use disorders, and mental illness among Ukrainian prisoners transitioning to the community. PLoS ONE. 2013;8:e59643. The authors present the results from a representative survey of HIV and related matters among recently-released Ukranian prisoners.
Henostroza G, Topp SM, Hatwiinda S, Maggard KR, Phiri W, Harris JB, et al. The high burden of tuberculosis (TB) and human immunodeficiency virus (HIV) in a large Zambian prison: a public health alert. PLoS ONE. 2013;8:e67338. In the first published survey of its kind, the authors present the results of a screening programme for HIV and TB in a large Zambian prison, establishing that correctional-associated HIV transmission and pathogenesis should be an urgent priority in efforts to address the pandemic in Sub-Saharan Africa.
Mohamed HI, Saad ZM, Abd-Elreheem EM, Abd-ElGhany WM, Mohamed MS, Abd Elnaeem EA, et al. Hepatitis C, hepatitis B and HIV infection among Egyptian prisoners: seroprevalence, risk factors and related chronic liver diseases. J Infect Public Health. 2013;6:186–95.
Semaille C, Le Strat Y, Chiron E, Chemlal K, Valantin MA, Serre P, et al. Prevalence of human immunodeficiency virus and hepatitis C virus among French prison inmates in 2010: a challenge for public health policy. Euro Surveill. 2013;18.
Honarvar B, Odoomi N, Moghadami M, Afsar Kazerooni P, Hassanabadi A, Zare Dolatabadi P, et al. Blood-borne hepatitis in opiate users in Iran: a poor outlook and urgent need to change nationwide screening policy. PLoS ONE. 2013;8:e82230.
Vagenas P, Azbel L, Polonsky M, Kerimi N, Mamyrov M, Dvoryak S, et al. A review of medical and substance use co-morbidities in Central Asian prisons: implications for HIV prevention and treatment. Drug Alcohol Depend. 2013;132 Suppl 1:S25–31.
Telisinghe L, Fielding KL, Malden JL, Hanifa Y, Churchyard GJ, Grant AD, et al. High tuberculosis prevalence in a South African prison: the need for routine tuberculosis screening. PLoS ONE. 2014;9:e87262.
Winetsky DE, Almukhamedov O, Pulatov D, Vezhnina N, Dooronbekova A, Zhussupov B. Prevalence, risk factors and social context of active pulmonary tuberculosis among prison inmates in Tajikistan. PLoS ONE. 2014;9:e86046.
Margolis B, Al-Darraji HAA, Wickersham JA, Kamarulzaman A, Altice FL. Prevalence of tuberculosis symptoms and latent tuberculous infection among prisoners in northeastern Malaysia. Int J Tuberc Lung Dis. 2013;17:1538–44.
Skrahina A, Hurevich H, Zalutskaya A, Sahalchyk E, Astrauko A, Hoffner S, et al. Multidrug-resistant tuberculosis in Belarus: the size of the problem and associated risk factors. Bull World Health Organ. 2013;91:36–45.
Milloy M-J, Wood E, Tyndall M, Lai C, Montaner J, Kerr T. Recent incarceration and use of a supervised injection facility in Vancouver, Canada. Addict Res Theory. 2009;17:538–45.
Buavirat A. Risk of prevalent HIV infection associated with incarceration among injecting drug users in Bangkok, Thailand: case-control study. BMJ. 2003;326:308.
Epperson M, El-Bassel N, Gilbert L, Orellana ER, Chang M. Increased HIV risk associated with criminal justice involvement among men on methadone. AIDS Behav. 2007;12:51–7.
Widman L, Noar SM, Golin CE, Willoughby JF, Crosby R. Incarceration and unstable housing interact to predict sexual risk behaviours among African American STD clinic patients. Int J STD AIDS. 2014;25:348–54.
Brewer RA, Magnus M, Kuo I, Wang L, Liu T-Y, Mayer KH. Exploring the relationship between incarceration and HIV among black men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2014;65:218–25.
Brewer RA, Magnus M, Kuo I, Wang L, Liu T-Y, Mayer KH. The high prevalence of incarceration history among Black men who have sex with men in the United States: associations and implications. Am J Public Health. 2014;104:448–54. An important analysis of the effects of mass incarceration on Black men who have sex with men in the United States.
Alexander M. The new Jim Crow. The New Press; 2013.
Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96:1007–19.
Halkitis PN, Kapadia F, Siconolfi DE, Moeller RW, Figueroa RP, Barton SC, et al. Individual, psychosocial, and social correlates of unprotected anal intercourse in a new generation of young men who have sex with men in New York City. Am J Public Health. 2013;103:889–95.
Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm. Rep. 2006;1–17.
Branson BM, Viall A, Marum E. Expanding HIV testing: back to the future. JAIDS J Acquir Immune Defic Syndr. 2013;63:S117.
Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373:48–57.
Yang Q, Boulos D, Yan P, Zhang F, Remis RS, Schanzer D, et al. Estimates of the number of prevalent and incident human immunodeficiency virus (HIV) infections in Canada, 2008. Can J Public Health. 2010;101:486–90.
Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA J Am Med Assoc. 2009;301:2380–2.
Gagnon M, Jacob JD, Cormier L. Total control: a critical analysis of mandatory HIV testing in U.S. prisons. J Forensic Nurs. 2013;9:154–61. The authors summarize the substantial ethical, legal and human rights concerns around HIV testing in US correctional settings.
Seal DW, Eldridge GD, Zack B, Sosman J. HIV testing and treatment with correctional populations: people, not prisoners. J Health Care Poor Underserved. 2010;21:977–85.
HIV testing and counselling in prisons and other closed settings. Geneva: United Nations Office on Drug Control and Crime; 2009 pp. 1–72.
Pope JL. HIV testing in state correctional systems. JL Health. 2009;22:17.
HIV/AIDS prevention, care, treatment and support in prison settings. New York City: United Nations Office on Drugs and Crime; 2006, pp. 1–50.
Spaulding AC, Booker CA, Freeman SH, Ball SW, Stein MS, Jordan AO, et al. Jails, HIV testing, and linkage to care services: an overview of the EnhanceLink initiative. AIDS Behav. 2013;17 Suppl 2:S100–7.
de Voux A, Spaulding AC, Beckwith C, Avery A, Williams C, Messina LC, et al. Early identification of HIV: empirical support for jail-based screening. PLoS ONE. 2012;7.
Beckwith CG, Nunn A, Baucom S, Getachew A, Akinwumi A, Herdman B, et al. Rapid HIV testing in large urban jails. Am J Public Health. 2012;102 Suppl 2:S184–6.
Centers for Disease Control and Prevention (CDC). Routine HIV screening during intake medical evaluation at a County Jail - Fulton County, Georgia, 2011-2012. MMWR Morb Mortal Wkly Rep. 2013;62:495–7.
Solomon L, Montague BT, Beckwith CG, Baillargeon J, Costa M, Dumont D, et al. Survey finds that many prisons and jails have room to improve HIV testing and coordination of postrelease treatment. Health Aff (Millwood). 2014;33:434–42. This survey of prison and jail systems in the United States reveals that a low proportion of settings offer HIV testing and linkage consistent with official guidelines.
Wohl DA, Golin C, Rosen DL, May JM, White BL. Detection of undiagnosed HIV among state prison entrants. JAMA J Am Med Assoc. 2013;310:2198–9.
Springer S, Friedland G, Doros G, Pesanti E, Altice F. Antiretroviral treatment regimen outcomes among HIV-infected prisoners. HIV Clin Trials. 2007;8:205–12.
Babudieri S, Aceti A, D’Offizi GP, Carbonara S, Starnini G. Directly observed therapy to treat HIV infection in prisoners. JAMA J Am Med Assoc. 2000;284:179–80.
Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of human immunodeficiency virus treatment during incarceration: viral suppression at the prison gate. JAMA Intern Med. 2014. doi:10.1001/jamainternmed.2014.601. This retrospective review of all known individuals living with HIV/AIDS in a US state correctional system found substantial improvements in virologic control during incarceration.
Davies N, Karstaedt AS. Antiretroviral outcomes in South African prisoners: a retrospective cohort analysis. PLoS ONE. 2012;7. This small study of individuals in the South African prison system reported virologic outcomes comparable to that observed in high-resource settings.
Baillargeon J, Giordano TP, Rich JD, Wu ZH, Wells K, Pollock BH, et al. Accessing antiretroviral therapy following release from prison. JAMA J Am Med Assoc. 2009;301:848–57.
Wakeman SE, McKinney ME, Rich JD. Filling the gap: the importance of medicaid continuity for former inmates. J Gen Intern Med. 2009;24:860–2.
Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, et al. Release from prison–a high risk of death for former inmates. N Engl J Med. 2007;356:157–65.
Booker CA, Flygare CT, Solomon L, Ball SW, Pustell MR, Bazerman LB, et al. Linkage to HIV care for jail detainees: findings from detention to the first 30 days after release. AIDS Behav. 2013;17 Suppl 2:S128–36. This study identified important correlates of successful linkage following incarceration, including stable housing, in individuals participating in the EnhanceLink initiative.
Small W, Wood E, Betteridge G, Montaner J, Kerr T. The impact of incarceration upon adherence to HIV treatment among HIV-positive injection drug users: a qualitative study. AIDS Care. 2009;21:708–14.
Milloy M-J, Kerr T, Buxton J, Rhodes T, Guillemi S, Hogg R, et al. Dose-response effect of incarceration events on nonadherence to HIV antiretroviral therapy among injection drug users. J Infect Dis. 2011;203:1215–21.
Kerr T, Marshall A, Walsh J, Palepu A, Tyndall M, Montaner J, et al. Determinants of HAART discontinuation among injection drug users. AIDS Care. 2005;17:539–49.
Milloy M-J, Kerr T, Buxton J, Rhodes T, Krusi A, Guillemi S, et al. Social and environmental predictors of plasma HIV RNA rebound among injection drug users treated with antiretroviral therapy. J Acquir Immune Defic Syndr. 2012;59:393–9.
Youmans E, Burch J, Moran R, Smith L, Duffus WA. Disease progression and characteristics of HIV-infected women with and without a history of criminal justice involvement. AIDS Behav. 2013;17:2644–53. This study describes how women with a history of involvement in the criminal justice system exhibit faster disease progression.
Westergaard RP, Hess T, Astemborski J, Mehta SH, Kirk GD. Longitudinal changes in engagement in care and viral suppression for HIV-infected injection drug users. AIDS. 2013;27:2559–66.
Pecoraro A, Royer-Malvestuto C, Rosenwasser B, Moore K, Howell A, Ma M, et al. Factors contributing to dropping out from and returning to HIV treatment in an inner city primary care HIV clinic in the United States. AIDS Care. 2013;25:1399–406.
Izenberg JM, Bachireddy C, Soule M, Kiriazova T, Dvoryak S, Altice FL. High rates of police detention among recently released HIV-infected prisoners in Ukraine: implications for health outcomes. Drug Alcohol Depend. 2013;133:154–60.
Springer SA, Qiu JJ, Saber-Tehrani AS, Altice FL. retention on buprenorphine is associated with high levels of maximal viral suppression among HIV-infected opioid dependent released prisoners. PLoS ONE. 2012;7.
Wickersham JA, Zahari MM, Azar MM, Kamarulzaman A, Altice FL. Methadone dose at the time of release from prison significantly influences retention in treatment: implications from a pilot study of HIV-infected prisoners transitioning to the community in Malaysia. Drug Alcohol Depend. 2013;132:378–82. This study reveals how methadone dose at time of release from prison improved retention in treatment among formerly-incarcerated prisoners in Malaysia.
Springer SA, Altice FL, Herme M, Di Paola A. Design and methods of a double blind randomized placebo-controlled trial of extended-release naltrexone for alcohol dependent and hazardous drinking prisoners with HIV who are transitioning to the community. Contemp Clin Trials. 2014;37:209–18.
Meyer JP, Zelenev A, Wickersham JA, Williams CT, Teixeira PA, Altice FL. Gender disparities in HIV treatment outcomes following release from jail: results from a multicenter study. Am J Public Health. 2014;104:434–41.
Althoff AL, Zelenev A, Meyer JP, Fu J, Brown S-E, Vagenas P, et al. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS Behav. 2013;17 Suppl 2:S156–70.
Avery AK, Ciomcia RW, Lincoln T, Desbrais M, Jordan AO, Rana AI, et al. Jails as an opportunity to increase engagement in HIV care: findings from an observational cross-sectional study. AIDS Behav. 2013;17 Suppl 2:S137–44.
Chen NE, Meyer JP, Avery AK, Draine J, Flanigan TP, Lincoln T, et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2013;17:2654–66.
Chitsaz E, Meyer JP, Krishnan A, Springer SA, Marcus R, Zaller N, et al. Contribution of substance use disorders on HIV treatment outcomes and antiretroviral medication adherence among HIV-infected persons entering jail. AIDS Behav. 2013;17 Suppl 2:S118–27.
Jordan AO, Cohen LR, Harriman G, Teixeira PA, Cruzado-Quiñones J, Venters H. Transitional care coordination in New York City jails: facilitating linkages to care for people with HIV returning home from Rikers Island. AIDS Behav. 2013;17 Suppl 2:S212–9.
Krishnan A, Wickersham JA, Chitsaz E, Springer SA, Jordan AO, Zaller N, et al. Post-release substance abuse outcomes among HIV-infected jail detainees: results from a multisite study. AIDS Behav. 2013;17 Suppl 2:S171–80.
Spaulding AC, Pinkerton SD, Superak H, Cunningham MJ, Resch S, Jordan AO, et al. Cost analysis of enhancing linkages to HIV care following jail: a cost-effective intervention. AIDS Behav. 2013;17 Suppl 2:S220–6.
Williams CT, Kim S, Meyer J, Spaulding A, Teixeira P, Avery A, et al. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV-positive clients leaving jail. AIDS Behav. 2013;17 Suppl 2:S195–202.
Zelenev A, Marcus R, Kopelev A, Cruzado-Quiñones J, Spaulding A, Desabrais M, et al. Patterns of homelessness and implications for HIV health after release from jail. AIDS Behav. 2013;17 Suppl 2:S181–94.
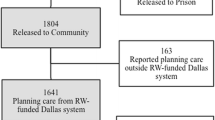
Spaulding AC, Messina LC, Kim BI, Chung K-W, Lincoln T, Teixeira P, et al. Planning for success predicts virus suppressed: results of a non-controlled, observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS Behav. 2013;17 Suppl 2:S203–11.
Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52:793–800.
Milloy M-J, Kerr T, Salters K, Samji H, Guillemi S, Montaner J, et al. Incarceration is associated with used syringe lending among active injection drug users with detectable plasma HIV-1 RNA: a longitudinal analysis. BMC Infect Dis. 2013;13:565.
Prellwitz IM, Alves BM, Ikeda MLR, Kuhleis D, Picon PD, Jarczewski CA, et al. HIV behind bars: human immunodeficiency virus cluster analysis and drug resistance in a reference correctional unit from southern Brazil. PLoS ONE. 2013;8:e69033.
Menezes P, Rosen D, Wohl DA, Kiziah N, Sebastian J, Eron JJJ, et al. Low prevalence of antiretroviral resistance among HIV type 1-positive prisoners in the Southeast United States. AIDS Res Hum Retrovir. 2013;29:136–41.
Montaner JSG, Lima VD, Harrigan PR, Lourenço L, Yip B, Nosyk B, et al. Expansion of HAART coverage is associated with sustained decreases in HIV/AIDS morbidity, mortality and HIV transmission: the “HIV treatment as prevention” experience in a Canadian setting. PLoS ONE. 2014;9:e87872.
Cescon A, Kanters S, Brumme CJ, Lepik KJ, Forrest JI, Hull M, et al. Trends in plasma HIV-RNA suppression and antiretroviral resistance in British Columbia, 1997-2010. J. Acquir Immune Defic Syndr. 2013.
Jürgens R, Betteridge G. Prisoners who inject drugs: public health and human rights imperatives. Health Hum Rights. 2005;8:46–74.
Acknowledgements
We thank Deborah Graham, Carmen Rock and Kristie Starr for their administrative assistance. This work was supported by the National Institutes of Health (R01 DA021525.) Dr. Milloy is supported by fellowships from the Canadian Institutes of Health Research and the Michael Smith Foundation for Health Research. This work was supported in part by a Tier 1 Canada Research Chair in Inner-City Medicine awarded to Dr. Wood.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
M-J Milloy and Evan Wood declare that they have no conflicts of interest.
Julio S.G. Montaner has received grants from Abbott, Biolytical, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck and ViiV Healthcare. He is also is supported: by the Ministry of Health Services and the Ministry of Healthy Living and Sport, from the Province of British Columbia; through a Knowledge Translation Award from the Canadian Institutes of Health Research (CIHR); and through an Avant-Garde Award (No. 1DP1DA026182) from the National Institute of Drug Abuse, at the US National Institutes of Health. He has also received support from the International AIDS Society, United Nations AIDS Program, World Health Organization, National Institute on Drug Abuse, National Institutes of Health Research-Office of AIDS Research, National Institute of Allergy & Infectious Diseases, the United States President’s Emergency Plan for AIDS Relief (PEPfAR), Bill & Melinda Gates Foundation, French National Agency for Research on AIDS & Viral Hepatitis (ANRS), Public Health Agency of Canada.
Human and Animal Rights and Informed Consent
This article does not contain primary reporting of any studies by the authors involving human or animal subjects.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Milloy, MJ., Montaner, J.S.G. & Wood, E. Incarceration of People Living with HIV/AIDS: Implications for Treatment-as-Prevention. Curr HIV/AIDS Rep 11, 308–316 (2014). https://doi.org/10.1007/s11904-014-0214-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-014-0214-z