Abstract
We reviewed papers published during the past 18 months (2012-2013) focusing on micro-social contexts of gender and power inequalities as drivers of HIV risks among people who inject drugs (PWID) in intimate heterosexual relationships. Although there has been a proliferation of social and behavioral research on the micro-social contexts of drug injection in heterosexual intimate relationships, there is still a gap in knowledge of these issues, particularly in low- and middle-income countries. Research has identified couple-based approaches for PWID in intimate relationships as an effective HIV prevention strategy to address micro-social contexts driving HIV risks. While HIV incidence has declined in many countries, prevalence remains at troubling levels among PWID and transmission from PWID to their sex partners is increasing in many parts of the world. HIV prevention among drug-using couples must address the importance of the relationship dyad and micro-social contexts.
Similar content being viewed by others
Introduction
Over the past decade, injection drug use (IDU) has caused a significant proportion of new HIV infections in many parts of the world, particularly in low- and middle-income countries [1, 2]. The prevalence of IDU is particularly high in Eastern Europe and Central Asia, reaching 1.3 % of the adult population [3]. Approximately 14 million people inject drugs globally [3], with HIV prevalence among people who inject drugs (PWID) reaching 12 % in China, 16 % in the U.S., and 37 % in Russia, the three countries with the highest numbers of injectors [4]. Approximately 1.6 million PWID are living with HIV, representing a prevalence of 11.5 % among PWID worldwide [3, 5]. It is estimated that one-third of PWID are female (FWID) [6, 7] and this number is growing globally [2].
Couples who use drugs often experience both drug and sexual risks for HIV, with dual risks influencing FWID in different ways than males who inject drugs (MWID). Des Jarlais et al. [8•] reviewed 117 studies from 14 countries where HIV prevalence is above 20 % and found a significantly higher HIV prevalence among FWID when compared to MWID [8•]. Research provides a number of potential explanations for these gender disparities in HIV prevalence: 1) Male-to-female sexual transmission of HIV may be more efficient than female-to-male transmission, placing FWID at higher risk for acquiring HIV through sexual risk behaviors [9], although other research suggests female-to-male transmission may be more efficient [10]. 2) Gender power imbalances and inequalities within drug cultures exist where FWID in intimate relationships have limited control over drug injection and sharing practices [11•, 12••, 13]. 3) FWID in intimate relationships may trade sex with other partners for money or drugs [11•]. 4) Structural risk environments (e.g., drug policies, discrimination, and lack of access to harm reduction programs and gender-specific services) may impede HIV prevention efforts among FWID [14].
In this paper, we focus on results of studies published in the past 18 months (2012-2013), specifically addressing micro-social contexts as drivers of HIV risks in heterosexual intimate relationships where one or both partners inject drugs. We examine the implications of micro-social contexts on couple-based HIV prevention interventions for PWID as a promising strategy to reduce HIV transmission.
Power and Social Inequalities as Drivers of HIV Among PWID in Intimate Relationships
Within the context of heterosexual relationships, research has shown that FWID are more likely to have male partners who also inject drugs, while MWID are more likely to have female sex partners with no history of injection [8•, 15, 16].
Females are more likely than males to experience their first drug injection with an intimate partner and to have that sexual partner inject them [17•, 18]. Additionally, females are often ‘second on the needle’ because control over injection equipment is in the hands of their partner [19]. A recent study with 30 young FWID in the U.S. found IDU initiation to be characterized by a lack of control over acquisition, preparation, and injection practices, which constrained choices and decisions about risk behavior and elevated HIV risks [12••]. The male’s role in the intimate relationship often includes obtaining the drug supply and injecting their female partner [12••, 19]. In contrast, most men quickly learn to self-inject and rarely permit their female sexual partners to inject them [12••].
Many FWID are regularly exposed to economic pressures and poverty and are more likely than MWID to be financially dependent on their partners to obtain drugs [14]. FWID who are sex workers may acquiesce to client demands for unsafe sex, especially if they are experiencing withdrawal [20, 21]. Recent literature suggests that while relationship contexts of power and control often lead to risk among FWID, it should not be assumed that all women are passive participants in injecting contexts. Among some couples, women have more control of injection practices than their male partners [22••]. In a study by Bryant et al. [23] among 181 PWID in Australia, in 25 % of the couples, the female was primarily responsible for acquiring and preparing drugs and obtaining needles. In other cases, FWID who engage in sex trading may have higher earning potential than their male partners, which can lead to relationship conflict and structural vulnerability [11•]. While social and economic contexts vary, financial vulnerability influences power dynamics and subsequent HIV risks among drug using couples, with females especially vulnerable to economic dependence.
Trust and Commitment in Intimate Relationships and HIV Risks Among PWID
Sharing drugs, needles/syringes, and other equipment (cotton, cookers, rinse water) in intimate relationships occurs within a context of close emotional involvement, trust, and commitment [17•, 18, 23, 24••]. For women, studies demonstrate that transitioning to IDU may occur largely from a desire to increase commitment and intimacy within a romantic partnership [22••, 23]. A study by Simmons et al. conducted in New York City considering retrospective accounts of 25 drug-using couples showed that emotional closeness within the dyad offset concerns about dangers and risks [18].
Romantic love and intimacy not only shape injection experiences, they also influence ways in which PWID assess and respond to HIV risks. FWID often see the cost of putting themselves at risk for HIV as less than the cost of jeopardizing their relationship [25]. Many couples who inject drugs are more likely to share needles when they experience a stronger connection with each other [26]. Some women trust their sex partners to inject them safely, feeling that injection by a partner is less physically damaging than self-injection [22••]. Injection by a partner may also be accompanied by exclusivity, with the act of the woman being injected by another man signifying betrayal [22••].
Similar micro-social contexts exist surrounding condom use in intimate relationships, where protection is rarely used because of love, trust, and commitment [24••, 27–31]. Condom use remains low in intimate relationships when compared to sex with casual and commercial partners [27, 32]. Due to assumptions of trust and expectations of fidelity, HIV and other STIs may be transmitted back and forth between the intimate dyad. Consequently, couples that inject drugs face both drug (sharing drugs, needles, and other equipment) and sexual (low condom use, having multiple sex partners) HIV risks.
FWID who trade sex for money or drugs are at particularly high risk for acquiring and transmitting HIV. Syversten et al. found that among drug-involved couples in Mexico where the female partner engaged in sex work, couples told ‘little lies’ and avoided talking about sex trading and associated HIV risks in order to preserve their intimate relationships. Avoidance of acknowledging such risky behaviors provided an illusion of fidelity and maintained the emotional integrity of the relationship. This silencing of risks may be common among socially marginalized populations such as sex workers and their partners seeking to avoid disclosure of sexual or other risky behaviors [11•]. FWID who trade sex may also use drugs with clients, which has been independently associated with HIV transmission [21]. In situations where female sex workers have regular clients on whom they depend to supply drugs and other commodities, it may be difficult to refuse unprotected sex and the line between client and intimate partner may be blurred [33].
Issues of trust, commitment, and related drug risks have not been sufficiently incorporated into HIV prevention for PWID in intimate relationships. HIV interventions for couples who inject drugs should frame safer sex behaviors as ways to protect, care, and demonstrate respect for one another [24••].
Social Network Roles Among PWID in Intimate Relationships and HIV Risks
Although couples who inject drugs often operate as dyadic units, overlapping drug and sexual social networks influence their injection practices [34, 35]. MWID in intimate relationships often serve as protectors and sources of support for their female partners. FWID often rely on their intimate partners to access needles through exchange programs or ‘on the street,’ which allows the male partner to control their relationships with broader social networks [36, 37•]. FWID often play passive roles within their social networks and rely on their intimate partners to manage resources, network social interaction, and access support [37•]. FWID tend to have fewer friends than their partners, especially female friends, and FWID may experience social isolation due to their male partner’s controlling behavior and the stigma associated with injection drug use [34, 35]. As sharing drugs with other men in the network without the knowledge and approval of the intimate partner may create conflict [22••], FWID may avoid disclosing drug or sexual risks to their main partner [27]. Similarly, the male partner may hide injection or sex with other women in their social network because disclosure is often taboo [38].
Social network dynamics may influence a female’s dependence on her male partner as well as the locations where drug use take place. FWID may feel unable to insist on using clean needles if they are dependent on the partner to provide drugs and other support, such as a place to stay, as well as protection from harm from others in their social network [18, 27]. For couples in some parts of the world, injecting at home with the partner is seen as reducing risks that occur when injecting with less trusted individuals in their social networks [22••, 24••]. Additionally, a preference for injection in non-public locations (at home or a friend’s place) [15] may allow couples to avoid police harassment and potential arrest. Although social network contexts have been integrated into the core components of some HIV prevention strategies for PWID [34, 35], strategies in low- and middle- income countries have not integrated these contextual issues.
Intimate Partner Violence (IPV) and Injection Drug Use as Drivers of HIV Risks
Compared to women who do not use drugs, the prevalence of sexual and physical IPV is 3-5 times higher among women who use or inject drugs [27, 29, 39]. FWID are often intimidated or threatened with physical and sexual violence to engage in syringe/needle sharing and high-risk sexual behaviors [27, 29, 32, 40]. Refusal to share needles often symbolizes distrust and a denial of intimacy in the relationship, which can lead to IPV [22••]. When refusal to share needles/drug equipment threatens the relationship and their safety, women may acquiesce to partner demands to engage in unsafe injection. After experiencing IPV, women may be hesitant to negotiate with their partners about condom use and the need for safer injection practices, or to deal with suspicions about their partner’s risk behaviors [27]. Additionally, drug use can lead to sexual desire incompatibility, which may create tension between the couple and lead to sexual IPV [24••]. Both victims and perpetrators tend to believe that perpetrators who are under the influence of drugs cannot be held accountable for sexual and physical abuse. Although IPV issues have been incorporated into some HIV prevention strategies for PWID [28], integrated IPV and HIV prevention for both members of the dyad remains rare.
Gender-Specific HIV Prevention Strategies that Address Micro-social Contexts for PWID in Intimate Heterosexual Relationships
There is a growing consensus on the need for a new generation of HIV prevention strategies targeting micro-social contexts such as a couple-based modality for female and male sex partners who inject drugs [41, 42]. Despite stereotypes of PWID as undisciplined or lacking the ability to commit to a healthy relationship, research has demonstrated that many couples who inject drugs maintain commitment to healthy relationships and are willing to engage in HIV risk reduction together [15, 22••].
Recent literature [11•, 22••, 41, 42] has highlighted the following reasons to urge the design, implementation, and adoption of couple-based (sex partner-based) HIV prevention modalities in real world settings for PWID: 1) Heterosexual transmission between MWID and their female partners is increasing in many parts of the world, especially in low and middle income countries [43]. 2) Men are rarely included in HIV prevention. 3) HIV prevention strategies have mainly focused on the individual and his/her needs and concerns, seldom including the other member of the couple. 4) HIV prevention strategies generally neglect micro-social risk environments that drive HIV transmission, such as the relationship context, low condom use in intimate relationships, the priority that women place in maintaining the relationship over sexual and drug risk protection, gender imbalances, and overlapping sexual and drug risk networks.
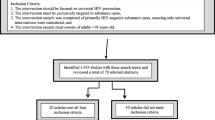
According to a systematic review conducted in 2013, 33 behavioral and biomedical couple-based HIV intervention studies have been implemented globally (Jiwatram Negron & El-Bassel, under review). Couple-based behavioral studies include: 1) skills building for sexual and drug risk reduction, 2) couple adherence to ART, and 3) couple counseling and testing. Couple biomedical studies include receiving ART as prevention, PrEP, and circumcision. Only three studies have been conducted exclusively with couples where one or both partners inject drugs, and where the dual risks of drugs and sex were addressed in the study core components [42, 44, 45]. Results from two of these are discussed below.
Connect II was a RCT conducted in the U.S. with 282 HIV-negative couples who inject drugs (564 individuals) who were randomly assigned to receive one of three interventions: couple-based HIV risk reduction, individual-based HIV risk reduction, or couple-based wellness promotion, which served as an attention control condition. At 12-month follow-up, there was a reduction in the number of unprotected acts of intercourse and unsafe injection with the study partner in the couple-based arm when compared to the individual arm [44]. The core components of this intervention focused on both sexual and drug risk reduction and emphasized the micro-social context in several ways, such as: 1) encouraging both partners to disclose and identify mutual drug risks (initiation, sharing drugs) and sexual risks (condom use, forced sex, forced unprotected sex); 2) encouraging the couple to identify and address gender differences in drug initiation, drug sharing, and associated risks, and to generate safe alternatives; 3) modeling, role-playing and practicing couple communication, negotiation, and problem solving skills that both partners may use together to lessen their drug-related and sexual risks; 4) practicing technical condom use placement skills along with a broader repertoire of pleasurable safer sex activities and syringe disinfection skills; and (5) enhancing the couple's motivation to protect each other and set mutual risk-reduction goals.
Facilitators were trained to validate the relationship's strengths of commitment, love, and trust, and to empower the dyad to enact protective sexual and drug behaviors. A safe environment was created where sensitive or taboo topics (e.g., outside sexual partners) related to a couple's risks could be disclosed and addressed. Couples had the opportunity to discuss their social network composition, the nature of their relationship, healthy and unhealthy aspects of their network relationships, and ways to expand their social network.
Couple-Based HIV-CT by McMahon et al., conducted with substance using HIV negative women and their primary heterosexual partners (N = 330 couples), showed that a brief couple-based HIV counseling and testing intervention designed to address both drug and sexual risk behaviors among substance-using women and their primary male partners was more effective when couples received the intervention together. Results showed the couple was more likely to improve and sustain positive protective drug and sexual behaviors over time, compared to when one partner received the intervention [42]. The intervention’s core components included couple counseling and testing, sexual and drug risk assessment, condom use, and referrals to drug treatment.
El-Bassel and Wechsberg summarized and highlighted a number of advantages to couple-based behavioral interventions [28]. A couple-oriented modality provides an opportunity for the dyad to recognize their mutual responsibility for protecting each other from HIV transmission and to work together to stay healthy. It accentuates the relationship's context (i.e., commitment, love, trust) and connection to HIV acquisition, and redirects attention to the value of the couple's relationship and the power of the dyad in behavioral change. A couple-based modality creates a safe environment that fosters discussion of sensitive topics (sexual concurrency, power imbalances in the relationship, couple's sexual preferences, sexual coercion, the meaning of love, connectedness in HIV risk among couples, initiation of drug use, sharing drugs, and sex trading). It provides a space for the pair to learn skills in couple communication, negotiation, problem solving, and couple goal-setting, as well as technical skills in condom use. Joint processing with the facilitator promotes accountability and increases commitment to change. Couple-based behavioral interventions can be used for PWID in combination with biomedical interventions to maximize their effects and produce sustainable outcomes.
Although most couple-based behavioral HIV intervention studies have excluded couples with severe IPV to avoid escalation of partner abuse when both attend sessions together, these couples may greatly benefit from receiving couple-based services. There is a growing consensus in the literature advocating for the inclusion of couples who report current or past severe abusive relationships in the intervention, but only if they both feel safe to attend the sessions together [28, 42, 46, 47]. Prior to enrollment, it is critical to assess the couple’s potential concerns about safety when participating together in the intervention. As a standard practice in couple-based HIV prevention, a safety planning protocol must be available to the couple [27, 28].
In the past several years, the HIV field has witnessed significant biomedical treatment advances with couples. Recent studies have shown that persons living with HIV who receive ART are much less infectious and, therefore, less likely to transmit HIV. In the HIV Prevention Trials Network (HPTN) 052 study, early initiation of ART reduced the transmission of HIV to negative partners by 96 % [48]. However, questions remain regarding barriers to recruitment and adherence and how micro-social contexts influence the participation and implementation of biomedical HIV prevention as well as ART adherence for PWID. Biomedical research has not adequately considered how these factors may play a role in promoting the participation of PWID in such interventions and how these factors affect adherence to ART. More attention needs to be paid to PWID in biomedical HIV prevention and treatment research and program implementation.
Globally, couple/partners-based approaches have yet to be broadly used, adopted, or accepted as the standard practice in HIV services at community-based organizations, primary health care settings, substance abuse treatment, and harm-reduction programs. In these settings, there is often a low level of awareness of the advantages of dyadic-based prevention interventions for PWID and a dearth of trained staff to deliver such services. To more fully understand and address risk contexts among PWID there must be a shift in the treatment ideology of staff and administrators, moving the emphasis from the individual to couple and social contexts including gender dynamics and social network characteristics. Capacity building is required in agencies that deliver this modality, including training staff to deliver couple-based interventions and ensuring that health insurance and other regulatory policies include service to both members of the couple [41].
Although a couple-based modality can be an important gender-specific HIV prevention strategy that addresses micro-social contexts, it is insufficient to be used alone without addressing other problems PWID face in dealing with risk environments driving the HIV epidemic. HIV prevention for PWID in intimate relationships must also focus on social network and structural interventions that deal with stigma, discrimination, incarceration, homelessness, lack of health insurance, and harsh drug policies [17•, 49].
Conclusion and Way Forward
While HIV incidence has declined in many countries, incidence remains at troubling levels among PWID. Transmission from PWID to their sex partners is increasing in many parts of the world [43, 50] and the number of FWID is rising [2]. The recent body of literature we reviewed identifies the following major micro-social contexts driving drug and sexual risk behaviors among PWID in intimate relationships: 1) power and social inequalities, 2) trust and commitment, 3) social support and the network’s role, and 4) IPV. Although the recent literature demonstrates an increased understanding of micro-social contexts, in many parts of the world, especially in low- and middle-income countries, this type of research remains limited. Understanding micro-social contexts in injection practices and sexual risks among PWID in intimate relationships is necessary to inform HIV prevention efforts that move beyond an individual approach [11•, 32, 39].
Current literature also underscores that a couple-based approach to HIV prevention for PWID in intimate heterosexual relationships (including those who engage in sex trading) promotes sexual and drug HIV risk reduction and encourages healthy relationships. Furthermore, the most recent advances in the use of couple-based biomedical HIV intervention research, such as the HPTN-052 study [48], demonstrate the role of couple based modalities in reducing HIV transmission from the positive to the negative partner. Despite these advances, couple-based HIV prevention for PWID remains scarce.
Recent literature consistently calls for combined (biomedical and behavioral) and multi-level (e.g., couple, community, structural) HIV prevention strategies for PWID and suggests that one HIV strategy is not sufficient to curb the HIV epidemic. In order for this shift from individual HIV interventions to those that address micro-social contexts and structural drivers of HIV, a serious investment and commitment by political leaders and funders must take place.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Jolley E, Rhodes T, Platt L, Hope V, Latypov A, Donoghoe M, et al. HIV among people who inject drugs in Central and Eastern Europe and Central Asia: a systematic review with implications for policy. BMJ Open. 2012;2(5).
UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2012. Switzerland: Joint United Nations Programme on HIV/AIDS (UNAIDS). 2012.
UNODC. World drug report: 2013. Vienna: United Nations Office on Drugs and Crime; 2013.
Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372:1733–45.
Mathers BM, Degenhardt L, Ali H, Wiessing L, Hickman M, Mattick RP, et al. HIV prevention, treatment, and care services for people who inject drugs: A systematic review of global, regional, and national coverage. Lancet. 2010;375:1014–28.
Pinkham S, Stoicescu C, Myers B. Developing effective health interventions for women who inject drugs: key areas and recommendations for program development and policy. Adv Prev Med. 2012.
SAMHSA. The NSDUH Report: Injection drug use and related risk behaviors (2009). Retrieved September 6, 2013.
Des Jarlais DC, Feelemyer JP, Modi SN, Arasteh K, Hagan H. Are females who inject drugs at higher risk for HIV infection than males who inject drugs: an international systematic review of high seroprevalence areas. Drug Alcohol Depend. 2012;124:95–107. This review identifies higher levels of HIV among females who inject drugs when compared to males who inject, highlighting the need for attention to prevention and treatment particularly among FWID.
Boily M-C, Baggaley RF, Wang L, Masse B, White RG, Hayes RJ, et al. Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies. Lancet Infect Dis. 2009;9(2):118–29.
Gray RH, Wawer MJ, Brookmeyer R, Sewankambo NK, Serwadda D, Wabwire-Mangen F, et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet. 2001;357(9263):1149–53.
Syvertsen JL, Robertson AM, Rolón ML, Palinkas LA, Martinez G, Rangel MG, et al. “Eyes that don't see, heart that doesn't feel”: coping with sex work in intimate relationships and its implications for HIV/STI prevention. Soc Sci Med. 2013;87:1–8. This paper explores communication between female sex workers who inject drugs and their intimate, non-commercial partners, finding that approaches to coping with sex work may heighten risks.
Wagner K D, Jackson Bloom J, Hathazi SD, Sanders B, Lankenau SE. Control over drug acquisition, preparation, and injection: implications for HIV and HCV risk among young female injection drug users. ISRN Addiction. 2013. Examining the social context of injection initiation among young females, this study points to the role of power, control, and dependence in risk production.
Wechsberg WM, Myers B, Reed E, Carney T, Emanuel AN, Browne FA (2013). Substance use, gender inequity, violence and sexual risk among couples in Cape Town. Cult Health Sex(ahead-of-print) 1–16.
El-Bassel N, Wechsberg WM, Shaw SA. Dual HIV risk and vulnerabilities among women who use or inject drugs: no single prevention strategy is the answer. Current opinion in HIV and AIDS. 2012;7(4), 326-331.
El-Bassel N, Gilbert L, Terlikbayeva A, Wu E, Beyrer C, Shaw S, et al. HIV among injection drug users and their intimate partners in Almaty, Kazakhstan. AIDS Behav. 2013;1–11.
Roberts A, Mathers B, Degenhardt L. Women who inject drugs: A review of their risks, experiences and needs (Vol. 12). University of New South Wales, Sydney, Australia: Secretariat of the Reference Group to the UN on HIV and Injecting Drug Use. National Drug and Alcohol Research Centre (NDARC). 2010.
Rhodes T, Wagner K, Strathdee S, Davidson P, Bourgois P. Structural violence and structural vulnerability within the risk environment: theoretical and methodilogical perspectives for a social epidemiology of hiv risk among injection drug users and sex workers. In: O’Campo P, Dunn J, editors. Rethinking social epidemiology: Towards a science of change. Berlin: Springer; 2012. p. 205–30. Considering risk production in multiple settings and with multiple theoretical and methodological lenses, Rhodes and co-authors address the critical nature of structural level vulnerabilities to HIV risk.
Simmons J, Rajan S, McMahon JM. Retrospective accounts of injection initiation in intimate partnerships. Int J Drug Policy. 2012;23(4):303–11.
Harvey E, Strathdee SA, Patrick DM, Ofner M, Archibald CP, Eades G, et al. A qualitative investigation into an HIV outbreak among injection drug users in Vancouver, British Columbia. AIDS Care. 1998;10(3):313–21.
Lau JTF, Tsui HY, Zhang Y, Cheng F, Zhang L, Zhang J, et al. Comparing HIV-related syringe-sharing behaviors among female IDU engaging versus not engaging in commercial sex. Drug Alcohol Depend. 2008;97(1–2):54–63.
Strathdee SA, Lozada R, Martinez G, Vera A, Rusch M, Nguyen L, et al. Social and structural factors associated with HIV infection among female sex workers who inject drugs in the Mexico-US border region. PLoS ONE. 2011;6(4):e19048.
Seear K, Gray R, Fraser S, Treloar C, Bryant J, Brener L. Rethinking safety and fidelity: the role of love and intimacy in hepatitis C transmission and prevention. Health Sociol Rev. 2012;12(3):272–86. Examining HCV among injection drug users in relationships, this qualitative study examines a key neglected are of research by exploring the importance of love and intimacy, and how romantic love influences and is influenced by drug use behaviors.
Bryant J, Brener L, Hull P, Treloar C. Needle sharing in regular sexual relationships: an examination of serodiscordance, drug using practices, and the gendered character of injecting. Drug Alcohol Depend. 2010;107(2–3):182–7.
Syvertsen JL, Robertson AM, Palinkas LA, Rangel MG, Martinez G, Strathdee SA. ‘Where sex ends and emotions begin’: love and HIV risk among female sex workers and their intimate, non-commercial partners along the Mexico-US border. Cult Health Sex. 2013;15(5):540–54. This study among female sex workers utilizes qualitative data to understand emotional relationships between females and their non-commercial partners, pointing to the role of intimacy in decisions about drug and sexual risk behaviors.
Lam NT. Drugs, sex and AIDS: sexual relationships among injecting drug users and their sexual partners in Vietnam. Cult Health Sex. 2008;10(S1):S123–37.
MacRae R, Aalto E. Gendered power dynamics and HIV risk in drug-using sexual relationships. AIDS Care. 2000;12(4):505–16.
El-Bassel N, Gilbert L, Witte S, Wu E, Chang M. Intimate partner violence and HIV among drug-involved women: contexts linking these two epidemics—challenges and implications for prevention and treatment. Subst Use Misuse. 2011;46(2–3):295–306.
El-Bassel N, Wechsberg WM. Couple-based behavioral HIV interventions: placing HIV risk-reduction responsibility and agency on the female and male dyad. Couple Fam Psychol Res Pract. 2012;1(2):94.
Gilbert L, El-Bassel N, Chang M, Shaw SA, Wu E, Roy L. Risk and protective factors for drug use and partner violence among women in emergency care. J Community Psychol. 2013;41(5):565–81.
Stockman JK, Morris MD, Martinez G, Lozada R, Patterson TL, Ulibarri MD, et al. Prevalence and correlates of female condom use and interest among injection drug-using female sex workers in two Mexico–US border cities. AIDS Behav. 2012;16(7):1877–86.
Uusküla A, Abel-Ollo K, Markina A, McNutt L-A, Heimer R. Condom use and partnership intimacy among drug injectors and their sexual partners in Estonia. Sex Transm Infect. 2012;88(1):58–62.
El-Bassel N, Wechsberg WM, Shaw SA. Dual HIV risk and vulnerabilities among women who use or inject drugs: no single prevention strategy is the answer. Curr Opin HIV AIDS. 2012;7(4):326–31.
Robertson AM, Syvertsen JL, Amaro H, Martinez G, Rangel MG, Patterson TL, et al. Can't buy my love: a typology of female sex workers’ commercial relationships in the Mexico-U.S. border region. J Sex Res. 2013;40:1–10.
Latkin C, Donnell D, Liu T-Y, Davey-Rothwell M, Celentano D, Metzger D. The dynamic relationship between social norms and behaviors: the results of an HIV prevention network intervention for injection drug users. Addiction. 2013;108:934–43.
Latkin C, Yang C, Srikrishnan AK, Solomon S, Mehta SH, Celentano DD, et al. The relationship between social network factors, HIV, and Hepatitis C among injection drug users in Chennai, India. Drug Alcohol Depend. 2011;117(1):50–4.
Cruz MF, Mantsios A, Ramos R, Case P, Brouwer KC, Ramos ME, et al. A qualitative exploration of gender in the context of injection drug use in two US–Mexico border cities. AIDS Behav. 2007;11(2):253–62.
Lazuardi E, Worth H, Saktiawati AMI, Spooner C, Padmawati R, Subronto Y. Boyfriends and injecting: the role of intimate male partners in the life of women who inject drugs in Central Java. Cult Health Sex. 2012;14(5):491–503. This qualitative study with females in Indonesia closely examines the roles of their male partners in injection drug use practices, highlighting dynamics of power and isolation, and discussing the need for tailoring prevention approaches to address these realities.
Lyons T, Madkins K, Karia P, Garner G. Intimate strangrs? Social networks in HIV-prevention groups for drug users. J Groups Addict Recover. 2013;8(2):129–48.
Stockman JK, Lucea MB, Campbell JC. Forced sexual initiation, sexual intimate partner violence and HIV risk in women: a global review of the literature. AIDS Behav. 2013;17(3):832–47.
El-Bassel N, Terlikbaeva A, Pinkham S. HIV and women who use drugs: double neglect, double risk. Lancet (Br Ed). 2010;376(9738):312.
El-Bassel N, Remien RH. Couple-based HIV prevention and treatment: state of science, gaps, and future directions family and HIV/AIDS: Cultural and contextual issues in prevention and treatment. New York: Springer; 2012. p. 153–72.
McMahon JM, Tortu S, Pouget ER, Torres L, Rodriguez W, Hamid R. Effectiveness of couple-based HIV counseling and testing for women substance users and their primary male partners: a randomized trial. Adv Prev Med. 2013;2013:1–15.
Des Jarlais DC, Feelemyer JP, Modi SN, Arasteh K, Mathers BM, Degenhardt L, et al. Transitions from injection-drug-use-concentrated to self-sustaining heterosexual HIV epidemics: patterns in the international data. PLoS ONE. 2012;7:e31227.
El-Bassel N, Gilbert L, Wu E, Witte SS, Chang M, Hill J, et al. Couple-based HIV prevention for low-income drug users from New York City: a randomized controlled trial to reduce dual risks. JAIDS J Acquir Immune Defic Syndr. 2011;58(2):198–206.
Gilbert L, El-Bassel N, Terlikbayeva A, Rozental Y, Chang M, Brisson A, et al. Couple-based HIV prevention for injecting drug users in Kazakhstan: a pilot intervention study. J Prev Interv Community. 2010;38(2):162–76.
Simmons J, McMahon JM. Barriers to drug treatment for IDU couples: the need for couple-based approaches. J Addict Dis. 2012;31(3):242–57.
Wechsberg WM, Luseno WK. The need for culturally appropriate, gender-specific global HIV prevention efforts with vulnerable women. J Prev Interv Community. 2010;38(2):85–8.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, et al. HIV and risk environment for injecting drug users: the past, present, and future. Lancet (Br Ed). 2010;376(9737):268.
Boltaev A, El-Bassel N, Deryabina A, Terlikbaeva A, Gilbert L, Hunt T, et al. The scaling up of HIV prevention for people who inject drugs in Central Asia: a review of structural challenges and ways forward. Drug Alcohol Depend. 2014;132:S41–7.
Acknowledgments
Nabila El-Bassel acknowledges the partial institutional support received from R01 (R01DA033168 funded by the National Institute of Drug Abuse.
Anindita Dasgupta acknowledges institutional support received from National Institute on Drug Abuse Grant T32DA023356 (pre-doctoral training grant; PI: Steffanie Strathdee).
Steffanie A. Strathdee acknowledges the partial institutional support from the National Institute on Drug Abuse (R37 DA019829) and from the National Institute of Health through HIV Prevention Trials Network (UM1 068619).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Nabila El-Bassel, Stacey A. Shawa, Anindita Dasguptab, and Steffanie A. Strathdeeb declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Bassel, N., Shaw, S.A., Dasgupta, A. et al. People Who Inject Drugs in Intimate Relationships: It Takes Two to Combat HIV. Curr HIV/AIDS Rep 11, 45–51 (2014). https://doi.org/10.1007/s11904-013-0192-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-013-0192-6