Abstract
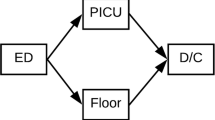
Pediatric trauma is one of the leading causes of morbidity and mortality in children in the USA. Every year, nearly 10 million children are evaluated in emergency departments (EDs) for traumatic injuries, resulting in 250,000 hospital admissions and 10,000 deaths. Pediatric trauma care in hospitals is distributed across time and space, and particularly complex with involvement of large and fluid care teams. Several clinical teams (including emergency medicine, surgery, anesthesiology, and pediatric critical care) converge to help support trauma care in the ED; this co-location in the ED can help to support communication, coordination and cooperation of team members. The most severe trauma cases often need surgery in the operating room (OR) and are admitted to the pediatric intensive care unit (PICU). These care transitions in pediatric trauma can result in loss of information or transfer of incorrect information, which can negatively affect the care a child will receive. In this study, we interviewed 18 clinicians about communication and coordination during pediatric trauma care transitions between the ED, OR and PICU. After the interview was completed, we surveyed them about patient safety during these transitions. Results of our study show that, despite the fact that the many services and units involved in pediatric trauma cooperate well together during trauma cases, important patient care information is often lost when transitioning patients between units. To safely manage the transition of this fragile and complex population, we need to find ways to better manage the information flow during these transitions by, for instance, providing technological support to ensure shared mental models.

Similar content being viewed by others
References
Center for Disease Control (CDC) (2015) Ten leading causes of death and injury. CDC. https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_age_group_2015_1050w740h.gif. Accessed 25 Jan 2018
Apker J, Mallak LA, Gibson SC (2007) Communicating in the "gray zone": perceptions about emergency physician hospitalist handoffs and patient safety. Acad Emerg Med Off J Soc Acad Emerg Med 14(10):884–894. https://doi.org/10.1197/j.aem.2007.06.037
Catchpole KR, Gangi A, Blocker RC, Ley EJ, Blaha J, Gewertz BL, Wiegmann DA (2013) Flow disruptions in trauma care handoffs. J Surg Res 184(1):586–591. https://doi.org/10.1016/j.jss.2013.02.038
Estryn-Behar M, Doppia MA, Guetarni K, Fry C, Machet G, Pelloux P, Aune I, Muster D, Lassauniere JM, Prudhomme C (2011) Emergency physicians accumulate more stress factors than other physicians-results from the French SESMAT study. Emerg Med J EMJ 28(5):397–410. https://doi.org/10.1136/emj.2009.082594
Johnston A, Abraham L, Greenslade J, Thom O, Carlstrom E, Wallis M, Crilly J (2016) Review article: staff perception of the emergency department working environment: integrative review of the literature. Emerg Med Australas EMA 28(1):7–26. https://doi.org/10.1111/1742-6723.12522
Hose B-Z, Hoonakker PLT, Wooldridge AR, Brazelton III, TB, Dean SM, Eithun B, Fackler JC, Gurses AP, Kelly MM, Kohler JE, McGeorge NM, Ross JC, Rusy DA, Carayon P (2019) Physician perceptions of the electronic problem list in pediatric trauma care. Appl Clin Inform 10(01):113-122. https://doi.org/10.1055/s-0039-1677737
Kitch BT, Cooper JB, Zapol WM, Marder JE, Karson A, Hutter M, Campbell EG (2008) Handoffs causing patient harm: a survey of medical and surgical house staff. Jt Comm J Qual Patient Saf 34(10):563–570
Dojmi Di Delupis F, Pisanelli P, Di Luccio G, Kennedy M, Tellini S, Nenci N, Guerrini E, Pini R, Franco Gensini G (2014) Communication during handover in the pre-hospital/hospital interface in Italy: from evaluation to implementation of multidisciplinary training through high-fidelity simulation. Intern Emerg Med 9(5):575–582. https://doi.org/10.1007/s11739-013-1040-9
Wooldridge AR, Carayon P, Hoonakker P, Hose B-Z, Ross J, Kohler J, Brazelton T, Eithun B, Kelly M, Dean S, Rusy D, Gurses A (2017) Understanding Team Complexity in Pediatric Trauma Care. In: Paper presented at the human factors and ergonomics in healthcare conference, New Orleans, LO, March 5–8, 2017
Durojaiye AB, McGeorge NM, Puett LL, Stewart D, Fackler JC, Hoonakker PLT, Lehmann HP, Gurses AP (2018) Mapping the flow of pediatric trauma patients using process mining on trauma registry data. Appl Clin Inform 09(03):654–666. https://doi.org/10.1055/s-0038-1668089
Wooldridge AR, Carayon P, Hoonakker PLT, Hose B-Z, Ross JC, Kohler JE, Brazelton TB, Eithun BL, Kelly MM, Dean SM, Rusy DA, Durojaiye A, Gurses AP (2018) Complexity of the pediatric trauma care process: implications for multi-level awareness. Cognit Technol Work. https://doi.org/10.1007/s10111-018-0520-0
American Academy of Pediatrics Committee on Pediatric Emergency Medicine (2016) Handoffs: transitions of care for children in the emergency department. Pediatrics 138(5):1–12. https://doi.org/10.1542/peds.2016-2680
Gandhi TK (2005) Fumbled handoffs: one dropped ball after another. Ann Intern Med 142(5):352–358
Calleja P, Aitken LM, Cooke ML (2011) Information transfer for multi-trauma patients on discharge from the emergency department: mixed-method narrative review. J Adv Nurs 67(1):4–18. https://doi.org/10.1111/j.1365-2648.2010.05494.x
Joint Commission (2012) Joint Commission Center for Transforming Healthcare releases targeted solutions tool for hand-off communications. Jt Comm Perspect Jt Comm Accredit Healthc Organ 32(8):1–3
Arora VM, Johnson JK, Meltzer DO, Humphrey HJ (2008) A theoretical framework and competency-based approach to improving handoffs. Qual Saf Health Care 17(1):11–14. https://doi.org/10.1136/qshc.2006.018952
Abraham J, Kannampallil T, Patel VL (2014) A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc 21(1):154–162. https://doi.org/10.1136/amiajnl-2012-001351
Horwitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jenq GY (2009) Dropping the Baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med 53(6):701–710.e704. https://doi.org/10.1016/j.annemergmed.2008.05.007
Arora VM, Johnson JK, Lovinger D, Humphrey HJ, Meltzer DO (2005) Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care 14(6):401–407. https://doi.org/10.1136/qshc.2005.015107
Sharma A, Lo V, Lapointe-Shaw L, Soong C, Wu PE, Wu RC (2017) A time-motion study of residents and medical students performing patient discharges from general internal medicine wards: a disjointed, interrupted process. Intern Emerg Med 12(6):789–798. https://doi.org/10.1007/s11739-017-1654-4
Beach C, Croskerry P, Shapiro M (2003) Profiles in patient safety: emergency care transitions. Acad Emerg Med Off J Soc Acad Emerg Med 10(4):364–367
Bigham MT, Logsdon TR, Manicone PE, Landrigan CP, Hayes LW, Randall KH, Grover P, Collins SB, Ramirez DE, O’Guin CD, Williams CI, Warnick RJ, Sharek PJ (2014) Decreasing handoff-related care failures in Children’s hospitals. Pediatrics 134(2):e572–e579. https://doi.org/10.1542/peds.2013-1844
Notrica DM, Brown D, Garcia-Filion P (2011) Development of a pediatric Level 1 trauma center at a freestanding children's hospital: staff attitudes and perceptions before and after trauma designation. J Pediatr Surg 46(9):1764–1770
Acosta CD, Delgado MK, Gisondi MA, Raghunathan A, D’Souza PA, Gilbert G, Spain DA, Christensen P, Wang NE (2010) Characteristics of pediatric trauma transfers to a level I trauma center: implications for developing a regionalized pediatric trauma system in California. Acad Emerg Med 17(12):1364–1373
Sorra J, Gray L, Streagle S, Famolaro T, Yount N, Behm J (2016) AHRQ Hospital Survey on Patient Safety Culture: User’s Guide. Agency for Healthcare Research and Quality (AHRQ), Rockville, MD
Zakrison TL, Rosenbloom B, McFarlan A, Jovicic A, Soklaridis S, Allen C, Schulman C, Namias N, Rizoli S (2016) Lost information during the handover of critically injured trauma patients: a mixed-methods study. BMJ Qual Saf 25(12):929–936. https://doi.org/10.1136/bmjqs-2014-003903
Joy BF, Elliott E, Hardy C, Sullivan C, Backer CL, Kane JM (2011) Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 12(3):304–308. https://doi.org/10.1097/PCC.0b013e3181fe25a1
Bernstein J, MacCourt DC, Jacob DM, Mehta S (2010) Utilizing information technology to mitigate the handoff risks caused by resident work hour restrictions. Clin Orthop Relat Res 468(10):2627–2632. https://doi.org/10.1007/s11999-010-1376-7
Sanchez LD, Chiu DT, Nathanson L, Horng S, Wolfe RE, Zeidel ML, Boyd K, Tibbles C, Calder S, Dufresne J, Yang JJ (2017) A model for electronic handoff between the emergency department and inpatient units. J Emerg Med 53(1):142–150. https://doi.org/10.1016/j.jemermed.2017.03.027
Starmer AJ, Landrigan CP (2015) Changes in medical errors with a handoff program. N Engl J Med 372(5):490–491. https://doi.org/10.1056/NEJMc1414788
Commission Joint (2017) Inadequate hand-off communication. Sentinel Alert Event 58:1–6
Keebler JR, Lazzara EH, Patzer BS, Palmer EM, Plummer JP, Smith DC, Lew V, Fouquet S, Chan YR, Riss R (2016) Meta-analyses of the effects of standardized handoff protocols on patient, provider, and organizational outcomes. Hum Factors 58(8):1187–1205. https://doi.org/10.1177/0018720816672309
Acknowledgements
Funding for this research was provided by the Agency for Healthcare Research and Quality (AHRQ) [Grant no. R01 HS023837]. The project described was supported by the Clinical and Translational Science Award (CTSA) program, through the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS), [Grant UL1TR002373]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. We thank the study participants, as our research would not be possible without them.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Human and animal rights statement
The study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects and was reviewed by University of Wisconsin - Madison Institutional Review Board.
Informed consent
Informed consent was obtained from all individuals participating in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoonakker, P.L.T., Wooldridge, A.R., Hose, BZ. et al. Information flow during pediatric trauma care transitions: things falling through the cracks. Intern Emerg Med 14, 797–805 (2019). https://doi.org/10.1007/s11739-019-02110-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-019-02110-7