Abstract
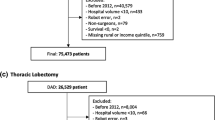
The appropriate use of the robot in surgery continues to evolve. Robotic operations (RO) are particularly advantageous for deep pelvic and retroperitoneal procedures, but the implementation of RO is unknown. We aimed to examine regional variation for the most commonly performed RO in general, gynecologic, and urologic surgery. A three-state inpatient database from 2008 to 2011 was used. Nine common robotic inpatient general, gynecologic and urologic surgery procedures were analyzed. States were divided into hospital service areas (HSAs). The percentage of RO was calculated for each operation. Hospital service areas that had < 50% or > 150% of the RO average were outliers. Hospital service areas were compared based on demographics, patterns of adoption, variation in usage, and association with population, physician and hospital density. Hysterectomies were the procedure that was performed most often robotically. Over 50% of radical prostatectomies were performed robotically. Procedures with the highest rate of RO performance were performed with the least variation. Characteristics that were significantly correlated with RO included provider and hospital density. Variation in the utilization of RO is common and differs by operation. Physician density impacts access to care and is associated with the variation in use of RO depending on procedure type. Further research is needed to understand the causes of variation and adoption of RO.
Similar content being viewed by others
References
Shah J, Vyas A, Vyas D (2014) The history of robotics in surgical specialties. Am J Robot Surg 1:12–20
Lanfranco AR, Castellanos AE, Desai JP, Meyers WC (2004) Robotic surgery: a current perspective. Ann Surg 239:14–21
Mack MJ (2001) Minimally invasive and robotic surgery. JAMA 285:568–572
Peters BS, Armijo PR, Krause C, Choudhury SA, Oleynikov D (2018) Review of emerging surgical robotic technology. Surg Endosc 32:1636–1655
California State Inpatient Database (SID). Healthcare Cost and Utilization Project (HCUP) [homepage on the Internet]. Rockville, MD: Agency for Healthcare Policy and Research. HCUP State Inpatient Databases (SID); Nov 2014 [cited 2014 Dec 30]. http://www.hcup-us.ahrq.gov/sidoverview.jsp. Accessed 20 Apr 2019
New York State Department of Health [homepage on the Internet] (2014) Albany, NY: State of New York; [cited 2014 Dec 30]. Data access—statewide planning and research cooperative system (SPARCS). https://www.health.ny.gov/statistics/sparcs/access/. Accessed 20 Apr 2019
Florida Health Finder [homepage on the Internet]. Tallahassee, FL: Florida agency for health care administration [cited 2014 Dec 30]. Order data/data dictionary. http://www.floridahealthfinder.gov/Researchers/OrderData/order-data.aspx. Accessed 20 Apr 2019
ICD-9-CM Diagnosis and Procedure Codes (2014) Abbreviated and full code titles. Secondary ICD-9-CM diagnosis and procedure codes: abbreviated and full codetitles. http://www.cms.gov/Medicare/Coding/ICD9-ProviderDiagnosticCodes/codes.html. Accessed 10 Nov 2018
Health Service Areas (2008) Secondary health service areas. http://seer.cancer.gov/seerstat/variables/countyattribs/hsa.html. Accessed 1 June 2014
Straney LD, Lim SS, Murray CJ (2012) Disentangling the effects of risk factors and clinical care on subnational variation in early neonatal mortality in the United States. PLoS One 7:e49399
Rural-urban continuum codes (2013) Documentation. Secondary rural-urban continuum codes: documentation. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx. Accessed 15 Feb 2015
Area Health Resources Files (AHRF). National, state and county health resources information database. Secondary area health resources files (AHRF). National, state and county health resources information database. http://ahrf.hrsa.gov. Accessed 15 Feb 2015
Curtin LR, Klein RJ (1995) Direct standardization (age-adjusted death rates). Healthy People 2000 Stat Notes:1–10, PMID: 11762384
Kuo LE, Murayama K, Simmons KD, Kelz RR (2017) Variation in the utilization of minimally invasive surgical operations. Ann Surg 265:514–520
Birkmeyer JD, Sharp SM, Finlayson SR, Fisher ES, Wennberg JE (1998) Variation profiles of common surgical procedures. Surgery 124:917–923
Hu JC, Wang Q, Pashos CL, Lipsitz SR, Keating NL (2008) Utilization and outcomes of minimally invasive radical prostatectomy. J Clin Oncol 26:2278–2284
Patel VR, Tully AS, Holmes R, Lindsay J (2005) Robotic radical prostatectomy in the community setting–the learning curve and beyond: initial 200 cases. J Urol 174:269–272
Berryhill R Jr, Jhaveri J, Yadav R, Leung R, Rao S, El-Hakim A, Tewari A (2008) Robotic prostatectomy: a review of outcomes compared with laparoscopic and open approaches. Urology 72:15–23
Coelho RF, Rocco B, Patel MB, Orvieto MA, Chauhan S, Ficarra V, Melegari S, Palmer KJ, Patel VR (2010) Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a critical review of outcomes reported by high-volume centers. J Endourol 24:2003–2015
Barakat EE, Bedaiwy MA, Zimberg S, Nutter B, Nosseir M, Falcone T (2011) Robotic-assisted, laparoscopic, and abdominal myomectomy: a comparison of surgical outcomes. Obstet Gynecol 117:256–265
Barnett JC, Judd JP, Wu JM, Scales CD Jr, Myers ER, Havrilesky LJ (2010) Cost comparison among robotic, laparoscopic, and open hysterectomy for endometrial cancer. Obstet Gynecol 116:685–693
Walters MD, Ridgeway BM (2017) Increasing utilization of minimally invasive hysterectomy. Clin Obstet Gynecol 60:273–285
Morgan DM, Kamdar NS, Swenson CW, Kobernik EK, Sammarco AG, Nallamothu B (2018) Nationwide trends in the utilization of and payments for hysterectomy in the United States among commercially insured women. Am J Obstet Gynecol 218:425 (e421–425 e418)
Marcus HJ, Hughes-Hallett A, Payne CJ, Cundy TP, Nandi D, Yang GZ, Darzi A (2017) Trends in the diffusion of robotic surgery: a retrospective observational study. Int J Med Robot 13(4):p.e1870
Aarts JW, Nieboer TE, Johnson N, Tavender E, Garry R, Mol BW, Kluivers KB (2015) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 8:CD003677.
Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, Buda A, Yan X, Shuzhong Y, Chetty N, Isla D, Tamura M, Zhu T, Robledo KP, Gebski V, Asher R, Behan V, Nicklin JL, Coleman RL, Obermair A (2018) Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med 379:1895–1904
Armijo PR, Pagkratis S, Boilesen E, Tanner T, Oleynikov D (2018) Growth in robotic-assisted procedures is from conversion of laparoscopic procedures and not from open surgeons’ conversion: a study of trends and costs. Surg Endosc 32:2106–2113
Wormer BA, Dacey KT, Williams KB, Bradley JF 3rd, Walters AL, Augenstein VA, Stefanidis D, Heniford BT (2014) The first nationwide evaluation of robotic general surgery: a regionalized, small but safe start. Surg Endosc 28:767–776
Jung M, Morel P, Buehler L, Buchs NC, Hagen ME (2015) Robotic general surgery: current practice, evidence, and perspective. Langenbecks Arch Surg 400:283–292
Tam MS, Kaoutzanis C, Mullard AJ, Regenbogen SE, Franz MG, Hendren S, Krapohl G, Vandewarker JF, Lampman RM, Cleary RK (2016) A population-based study comparing laparoscopic and robotic outcomes in colorectal surgery. Surg Endosc 30:455–463
Halabi WJ, Kang CY, Jafari MD, Nguyen VQ, Carmichael JC, Mills S, Stamos MJ, Pigazzi A (2013) Robotic-assisted colorectal surgery in the United States: a nationwide analysis of trends and outcomes. World J Surg 37:2782–2790
Thiele RH, Rea KM, Turrentine FE, Friel CM, Hassinger TE, McMurry TL, Goudreau BJ, Umapathi BA, Kron IL, Sawyer RG, Hedrick TL (2015) Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg 220:430–443
Coffey JC, Dockery P (2016) Colorectal cancer: surgery for colorectal cancer—standardization required. Nat Rev Gastroenterol Hepatol 13:256–257
Daes J (2015) Standardization of hernia surgery. Hernia 19:1039–1040
Eto K, Urashima M, Kosuge M, Ohkuma M, Noaki R, Neki K, Ito D, Takeda Y, Sugano H, Yanaga K (2018) Standardization of surgical procedures to reduce risk of anastomotic leakage, reoperation, and surgical site infection in colorectal cancer surgery: a retrospective cohort study of 1189 patients. Int J Colorectal Dis 33:755–762
Cooper RA (2009) States with more physicians have better-quality health care. Health Aff (Millwood) 28:w91–102
Funding
This manuscript did not receive independent funding. State databases from California, Florida and New York were utilized for this manuscript with permission for use of data and appropriate citations provided in the reference section of the manuscript. All authors listed meet the criteria for authorship and have approved this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Jennifer H. Fieber, Dr. Lindsay E. Kuo, Dr. Rachel R. Kelz, and Mr. Chris Wirtalla declare that they have no conflicts of interest. A portion of material in this manuscript was previously presented in the form of a published abstract and poster presentation at the Surgical Forum of the American College of Surgeons in Boston, Massachusetts on October 22nd 2018.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fieber, J.H., Kuo, L.E., Wirtalla, C. et al. Variation in the utilization of robotic surgical operations. J Robotic Surg 14, 593–599 (2020). https://doi.org/10.1007/s11701-019-01003-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-019-01003-3