Abstract
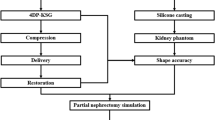
To construct patient-specific physical three-dimensional (3D) models of renal units with materials that approximates the properties of renal tissue to allow pre-operative and robotic training surgical simulation, 3D physical kidney models were created (3DSystems, Rock Hill, SC) using computerized tomography to segment structures of interest (parenchyma, vasculature, collection system, and tumor). Images were converted to a 3D surface mesh file for fabrication using a multi-jet 3D printer. A novel construction technique was employed to approximate normal renal tissue texture, printers selectively deposited photopolymer material forming the outer shell of the kidney, and subsequently, an agarose gel solution was injected into the inner cavity recreating the spongier renal parenchyma. We constructed seven models of renal units with suspected malignancies. Partial nephrectomy and renorrhaphy were performed on each of the replicas. Subsequently all patients successfully underwent robotic partial nephrectomy. Average tumor diameter was 4.4 cm, warm ischemia time was 25 min, RENAL nephrometry score was 7.4, and surgical margins were negative. A comparison was made between the seven cases and the Tulane Urology prospectively maintained robotic partial nephrectomy database. Patients with surgical models had larger tumors, higher nephrometry score, longer warm ischemic time, fewer positive surgical margins, shorter hospitalization, and fewer post-operative complications; however, the only significant finding was lower estimated blood loss (186 cc vs 236; p = 0.01). In this feasibility study, pre-operative resectable physical 3D models can be constructed and used as patient-specific surgical simulation tools; further study will need to demonstrate if this results in improvement of surgical outcomes and robotic simulation education.



Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- CT:
-
Computerized tomography
- STL:
-
Surface mesh file
- RAPN:
-
Robot-assisted partial nephrectomy
- GFR:
-
Glomerular filtration rate
- CKD:
-
Chronic kidney disease
- AR:
-
Augmented reality
References
Atug F, Castle EP, Woods M et al (2006) Robotics in urologic surgery: an evolving new technology. Int J Urol 13:857–863
Rashid HH, Leung YM, Rashid MJ et al (2006) Robotic surgical education: a systematic approach to training urology resident to perform robotic-assisted laparoscopic radical prostatectomy. J Urol 68:75–79
Grover S, Tan GY, Srivastava A et al (2010) Residency training program paradigms for teaching robotic surgical skills in urology residents. Curr Urol Rep 11:87–92
Schreuder HW, Wolswijk R, Zweemer RP et al (2012) Training and learning robotic surgery, time for a more structured approach: a systematic review. BJOG 119:137–149
Liss MA, McDougall EM (2013) Robotic surgical simulation. Cancer J 19:124–129
Sun AJ, Arong M, Hung AJ (2014) Novel training methods for robotic surgery. Indian J Urol 30(3):333–338
Mehra P, Miner J, D’Innocenzo R et al (2011) Use of 3-d stereolithographic models in oral and maxillofacial surgery. J Maxillofac Oral Surg 10:6–13
Starosolski Z, Kan JH, Rosenfeld SD et al (2014) Application of 3-D printing (rapid prototyping) for creating physical models of pediatric orthopedic disorders. Pediatr Radiol 44:216–221
Silberstein JL, Maddox MM, Dorsey P et al (2014) Physical models of renal malignancies using standard cross-sectional imaging and 3-dimensional printers: a pilot study. Urology 84:268–272
Cheung CL, Looi T, Lendvay TS et al (2014) Use of 3-dimensional printing technology and silicone modeling in surgical simulation: development and face validation in pediatric laparoscopic pyeloplasty. J Surg Educ 71(5):762–767
Zhang Y, Ge HW, Li NC et al (2016) Evaluation of three-dimensional printing for laparoscopic partial nephrectomy of renal tumors: a preliminary report. World J Urol 34(4):533–537
Petros F, Sukumar S, Haber G-P et al (2012) Multi-institutional analysis of robot-assisted partial nephrectomy for renal tumors > 4 cm versus ≤4 cm in 445 consecutive patients. J Endourol 26:642–646
Dworkin DL, Brenner BM (2004) Brenner and Rector's: the kidney, 7th edn. Elsevier, Philadelphia, PA
Thompson RH, Lane BR, Lohse CM et al (2010) Every minute counts when the renal hilum is clamped during partial nephrectomy. Eur Urol 58(3):340–345
Liss MA, McDougall EM (2013) Robotic surgical simulation. Cancer J 111(2):124–129
Hung AJ, Zehnder P, Patil MB et al (2011) Face, content and construct validity of a novel robotic surgery simulator. J Urol 186:1019–1024
Korets R, Mues AC, Graversen JA et al (2011) Validating the use of the Mimic dV-trainer for robotic surgery skill acquisition among urology residents. Urology 78:1326–1330
Seixas-Mikelus SA, Kesavadas T, Srimathveeravalli G et al (2010) Face validation of a novel robotic surgical simulator. Urology 76:357–360
Kumar A, Smith R, Patel VR (2015) Current status of robotic simulators in acquisition of robotic surgical skills. Curr Opin Urol 25(2):168–174
Hung AJ, Shah SH, Dalag L et al (2015) Development and validation of a novel robotic procedure-specific simulation platform: partial nephrectomy. J Urol 194(2):520–526
Knoedler M, Feibus A, Lange A et al (2015) Individualized physical 3-dimensional kidney tumor models constructed from 3-dimensional printers result in improved trainee anatomic understanding. Urology 85(6):1257–1262
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
None.
Ethical approval
This article does not contain any studies with animals or human participants performed by any authors.
Informed consent
Informed consent was obtained from all individual participants included in this study to use cross-sectional imaging as template for 3D models.
Rights and permissions
About this article
Cite this article
Maddox, M.M., Feibus, A., Liu, J. et al. 3D-printed soft-tissue physical models of renal malignancies for individualized surgical simulation: a feasibility study. J Robotic Surg 12, 27–33 (2018). https://doi.org/10.1007/s11701-017-0680-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-017-0680-6